Believe you can and you’re halfway there.”
– Theodore Roosevelt
Meralgia Paresthetica (MP)
Meralgia paresthetica (MP) is a condition associated with tingling, numbness and burning pain in the anterolateral part of the thigh, though sometimes characterized by lightning or electric pain, deep muscle achiness or, rarely, local hair loss in the anterolateral thigh. Usually unilateral, up to 20% of patients have bilateral symptoms.
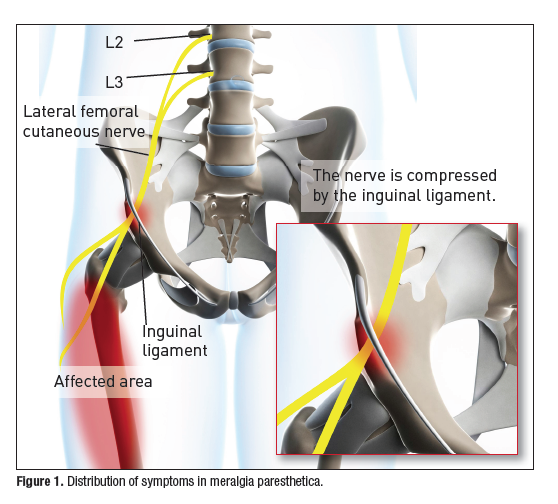
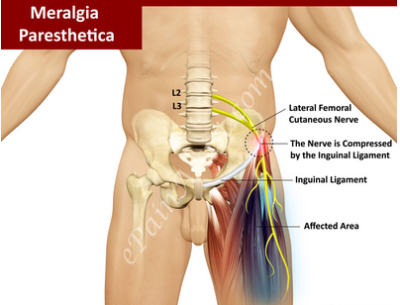
MP is usually caused by compression of the lateral femoral cutaneous nerve (LCFN), the nerve that supplies sensation to the skin surface of your thigh. It can also be associated with nerve dysfunction from diabetes or as a result of nerve injury sustained during surgery or other trauma.
See Also:
.
Meralgia Paresthetica
Meralgia paresthetica is uncommon but not rare and is identified more often in males than in females. It is observed in all age groups, but most commonly in middle-aged adults, age 40-60. Changes in posture or prolonged sitting or standing may cause a fluctuation of symptoms, either incresing or decreasing severity and symptoms may resolve spontaneously and reappear.
Pathophysiology
The lateral femoral cutaneous nerve (LFCN), formed by the fusion of branches of the second and third lumbar nerves, provides purely sensory function to the anterolateral thigh. However individual variants in the derivation of the LFCN occur, including several different combinations of lumbar nerves, including L2 and L3, L1 and L2, L2 alone, and L3 alone. The LFCN nerve traverses from the L2 & L3 vertebrae through the retroperitoneum and around the lateral pelvis where it passes underneath the inguinal ligament and enters the anterior thigh. There are also many individual variations in the anatomy of the course of the LFCN, such as splitting by the inguinal ligament, that are believed to predispose an individual to meralgia paresthetica.
Compression of the LFCN can occur at 3 possible sites:
(1) beside the spinal column
(2) within the abdominal cavity as the nerve courses along the pelvis
(3) as the nerve exits the pelvis. This is the most common site of compression, either with nerve entrapment by the sartorius muscle, or by compression superficially near the iliac crest and anterior superior iliac spine.
Common causes of this compression include any condition that increases pressure on the groin, including:
(1) Tight clothing or belt
(2) Obesity
(3) Pregnancy
(4) Ascites
(5) Scoliosis
(6) Walking, cycling or standing for long periods of time
It can also occur as a result of:
(1) Nerve dysfunction due to diabetes, hypothyroidism, alcohol or lead poisoning
(2) Nerve dysfunction due to Vitamin B12 or folate deficiency
(3) Nerve injury such as a seat belt injury in a motor vehicle accident
(4) Nerve trauma resulting in a neuroma, an overgrowth of nerve fibers and connective tissue
(5) Nerve injury during surgery, especially laparoscopic inguinal hernia repair
(6) Scar tissue near the inguinal ligament, due to injury or past surgery of the lower abdomen/pelvis
Physical Exam
Isolated compression or lesions of the LFCN result only in abnormalities on sensory examination. Typically, reduced response to pinprick or dysesthesias (abnormal sensations) or hypersensitivity within the distribution of the LFCN is found. The patient can often outline the cutaneous boundaries of the symptoms with an ink marker on their thigh.
Hip extension may elicit or worsen symptoms, while flexion may relieve them. Appliying pressure over the LFCN at the inguinal ligament may elicit tenderness or worsen the symptoms. Tapping over the upper and lateral aspects of the inguinal ligament (Tinel’s sign) may elicit symptoms that reproduce complaints. Extending the thigh posteriorly, which stretches the nerve, may reproduce or worsen the paresthesias.Deep palpation just below the anterior superior iliac spine usually reproduces the symptoms.
Pelvic Compression Testing
The pelvic compression test is a diagnostic tool that involves placing the patient in the lateral recumbent position while an external downward force is applied with the examiner’s hands over the lateral aspect of the ASIS. The pressure is held for 45 seconds to determine if the patient’s symptoms improved. Symptom amelioration is considered a positive test result and helps to rule out lumbosacral radicular pain. A study in 45 patients found that the pelvic compression test had a sensitivity of 95% and a specificity of 93.3% for meralgia paresthetica.
Because the LFCN is purely sensory, any other neurologic abnormalities on exam such as abnormalities in reflexes, strength, gait, or sensation outside the boundaries of the LFCN, indicate a process beyond just the LFCN. Motor strength in the involved leg should be normal. For example, reduced patellar reflex and weak leg extension accompanying symptoms of MP indicate possible pathology within the lumbar plexus (a plexopathy) or lumbar nerve root(s) compressio. This condition require greater evaluation.
Diagnostic Tests
The diagnosis of MP can generally by established by history and physical exam though the specific cause or site of compression may not be evident. An MRI of the lumbar spine can help identify other pathology such as nerve root compression but is ineffective in visualizing the affected portion of the LFCN. A more specific nerve assessment can be obtained with an EMG/NCS (electromyogram and nerve conduction study) to identify dysfunction of the LFCN vs. nerve root involvment but is not always diagnostic.
Anesthetizing the LFCN by an ultrasound-guided nerve block is helpful in confirming the diagnosis in 80% – 100% of rep0rted case studies and may be curative, but it is also useful in allowing the patient to experience the anticipated results of a nerve resection. Attempting to perform the block blindly, without ultrasound guidance, has about a 60% failure rate compared with ultrasound-guidance.
Treatment
Conservative Measures
A conservative approach is effective for most people, with pain usually going away on its own within a few months. Conservative measures include:
(1) Wearing looser clothing and belts
(2) Remove wallets, bulky items from pockets
(3) Losing weight
(4) Use of nonsteroid anti-inflammatory medications (NSAIDs)
Physical Therapy
Individual assements should be performed by a physical therapist to identify specific findings to direct treatment
Radiofrequency Nerve Ablations
A case study published in 2009 reported that pulsed radiofrequency ablations resulted in complete and sustained cessation of pain in MP. No side effects were evident. Pulsed radiofrequency of the LFCN may offer an effective, low risk treatment in patients with meralgia paresthetica who are refractory to conservative medical management or are unwilling or unfit to undergo surgery.
Surgery
Rarely, patients who fail to respond to more conservative therapy should be considered for surgery, but there is no consensus as to the best surgical treatment.
Resources:
References
Meralgia Paresthetica – Overviews
- Meralgia Paresthetica, The Elusive Diagnosis – 2000
- Meralgia_Paresthetica A_Common_Cause_of_Thigh_Pain_-_2014
Meralgia Paresthetica – Pulsed Radiofrequency Ablation
Meralgia Paresthetica – Ultrasound-guided Nerve Block
.
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.