THC
THC Pharmacokinetics
Pharmacokinetics refers to what the body does to a drug, how the drug moves into, through, and out of the body: the time course of its absorption, bioavailability, distribution, metabolism, and excretion.
Understanding the pharmacokinetics of Δ-9 tetrahydrocannabinol (THC) and other cannabis constituents allows for identifying the pros and cons of the different formulations of cannabis/cannabinoids available as well as avoiding unintended responses and adverse effects associated with taking cannabis/cannabinoid products.
Links to other Pertinent Educational Pages:
See also:
Marijuana (Cannabis): Side Effects and Drug Interactions
The medical information on this site is provided as a resource for information only, and is not to be used or relied upon for any diagnostic or treatment purposes and is not intended to create any patient-physician relationship. Readers are advised to seek professional guidance regarding the diagnosis and treatment of their medical concerns.
Key to Links:
Grey text – handout
Red text – another page on this website
Blue text – Journal publication
.
THC (Δ-9 tetrahydrocannabinol) Pharmacokinetics
Botanical Cannabis and THC
Botanical cannabis is highly variable in its chemical composition and content of THC. Fresh cannabis plants in actuality contain little to no THC but instead contain tetrahydrocannabinolic acid (THCA), the precursor or pro-drug to THC. THCA is the main constituent in cannabis resin concentrates, such as hashish and hash oil, comprising between 50% and 90% by weight. THCA is not psychoactive like THC but does have some immuno-modulating effects but they are not mediated by the cannabinoid CB1 and CB2 receptor pathways. For THCA to become activated and converted to THC for therapeutic use, it must be exposed to intense heat such as when cannabis is smoked or cooked into cannabis edibles.
These acid cannabinoids have had much less research, but are known to possess pharmacological properties in their own right. CBDA is a powerful anti-emetic and anti-anxiety agent (at least in rodents), and has anecdotal reports of benefit on skin and tumors. THCA produces anti-inflammatory effects and is a strong anti-emetic with neuroprotective and anticonvulsant effects.
THCA and CBDA concentrations depend on the species, strain, cultivation, and storage of the plant. The average concentrations in more than 30,000 cannabis preparations confiscated in the U.S. between 1980 and 1997 were 3.1% THCA and only 0.3% CBDA. Various strains and marijuana-based products are now available that contain substantially higher contents of these constituents, especially THC.
∆9-THC is thermolabile and photolabile, meaning they are broken down (oxidized) when exposed to heat or light. Storage leads to a decrease in total THC content via oxidation of THC to CBN. Within 1 year, the THC content of dried cannabis leaves and flowers decreases by 7% with dark and dry storage at 5°C, and by 13% at 20°C. With additional light exposure, the loss increases threefold to 36%. Degradation in hashish occurs much more quickly since the cannabinoids are no longer protected against oxidation by the glandular trichome structures in the flower.
Bioavailability
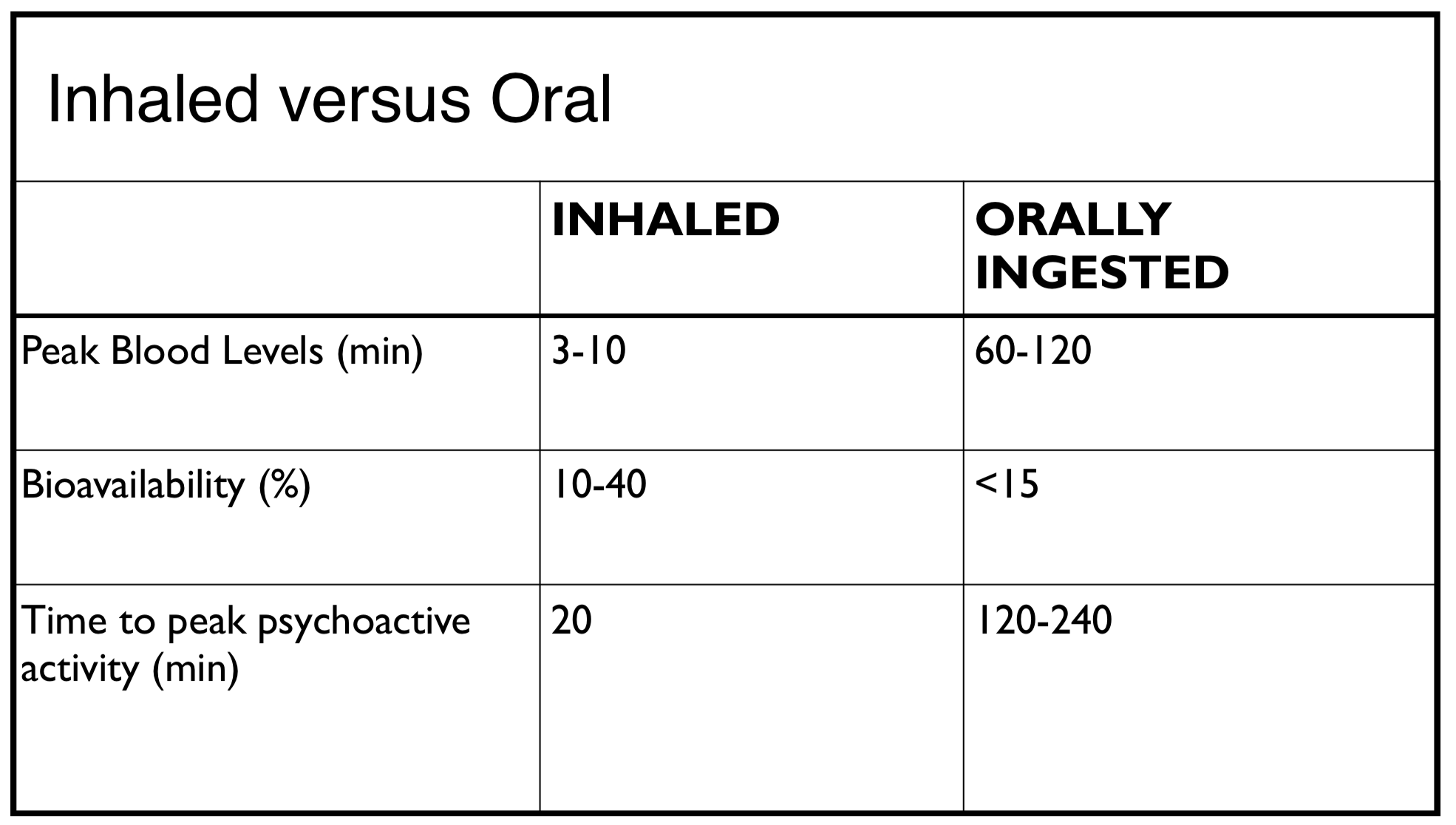
The “bioavailability” of a medication is the measure of how effectively administration of that medicine achieves blood levels. As a standard of definition, the bioavailability of a medication given directly intravenously is 100%. Other forms of administration, such as smoking, eating and application to skin, will be associated with less bioavailability. With inhaling, THC bioavailability averages 30%. With a 3.55% THC cigarette, a peak plasma level of 152±86 ng/mL is reached approximately 10 min after inhalation. Oral THC, on the other hand, is only 4 to 12% bioavailable and absorption is highly variable.
Bioavailability is generally described in terms of maximum time in the blood (Cmax) and maximum overall absorption into the blood (AUC – Area under the Curve). Tmax is the time necessary to reach the maximum blood concentration after administration of a medication.
- Smoking: 25-30% bioavailability (Reports vary from 2-56%)
- Vaporization: 30-60% bioavailability
- Tinctures (sublingual): 40-50% bioavailability
- Edibles: 5-12% bioavailability (Reports vary from 4-20%)
- Intranasal: 6.4–9.1% bioavailability
- Transdermal:
Inhalation vs. Sublingual/Buccal Route vs. Oral Use of THC
The pharmacokinetics of THC are very different depending on the method of use. Inhalation provides the most rapid onset, but the shortest duration of effect. Oral ingestion provides the slowest onset but the longest duration of effect, whereas the sublingual route, holding the medicine under the tongue for 1-2 minutes to allow for buccal absorption directly into the blood, is in-between inhalation and oral. But there is more to it than this quantitative difference, there are also qualitative differences in therapeutic effects.
Inhalation: Smoking and Vaping
When cannabis is inhaled via smoking or vaping, THC is absorbed directly from the lungs (where little to no metabolism takes place) into the bloodstream almost immediately. Inhaled use of THC leads to near immediate maximum blood levels but these levels are markedly reduced in 2 hours or less.
Inhalation and 11-OH-THC.
THC quickly distributes from the blood to other body tissues and only a small fraction of it remains in the blood. The THC that remains available in the blood passes through the liver where it is converted to 11-OH-THC and other metabolites. However, the larger fraction of THC in other tissues does not contribute significantly to blood levels of 11-OH-THC and therefore, overall, not much 11-OH-THC is initially formed with inhalation. The levels of 11-OH-THC in the blood after smoking cannabis is only about 5% of THC levels, probably not enough to contribute significant psychoactive effects from the 11-OH-THC
(See: 11-OH-THC below).
Sublingual/Buccal Route
Sublingual administration leads to peak blood levels in about an hour but duration of levels markedly drop off in about 4 hours, depending on the dose. Mean AUC and Cmax are one to three-fold higher for THC (and 11-OH-THC) with eating, although there is large inter-subject variability, particularly for THC.
Oral Use of THC
Oral administration (swallowing) leads to peak levels that may be not peak up to 4 hours or longer and may take more than 8-12 hours before dropping off. The presence of high-fat food when ingesting THC significantly enhances time to peak plasma concentration (T max) and area under the curve (AUC0-24) for both THC and 11-OH-THC. It is noted also that females appear to have a significantly greater peak plasma concentration (C max) compared with males after 5 mg THC in a fasted state.
Gastric Emptying
THC delays gastric emptying of solid foods, although not liquids. This may nevertheless impact alcohol absorption because although alcohol is absorbed to some extent from the stomach, it has to reach the small intestine to be fully absorbed, and a delay in gastric emptying slows the absorption of alcohol.
Transdermal Route
The steady-state blood concentrations of transdermal THC maintain throughout 48 hours of gel application, starting to decline at about 6 hours after gel removal, indicating a skin reservoir effect in guinea pigs. The skin reservoir property of THC is because of the high lipophilic property of the drug that makes it easier to cross the stratum corneum but makes it difficult to traverse through the aqueous dermis.
Because THC is more lipophilic than CBD, the skin reservoir effect is higher with THC, but steady-state blood concentrations of THC are lower than thoseachieved with CBD. With the use of the enhancer, CBD is delivered up to 3.7 times better than without, suggesting this would be the case with transdermal THC.
Intranasal Route
The major problem associated with THC is the abuse potential and other central nervous system side effects seen with high doses. This is especially important to avoid with intranasal delivery, which may result in high concentrations in the brain through rapid absorption.
THC Metabolism
THC Metabolism – Liver
Most of the THC that enters the body is metabolized in the liver into over 100 metabolites, with 11-OH- THC and THC-COOH being the two major metabolites. The primary metabolite, 11-OH-THC, is psychoactive, contributing to the effects of THC on thought processing, mood and euphoria. 11-OH-THC diffuses into the brain more readily than THC does and its effects are perceived more rapidly than with THC. 11-OH-THC is subsequently metabolized into THC-COOH, which is inactive, and ultimately excreted into feces (65%) and urine (20%). THC is significantly metabolized with just one pass through the liver, the “first pass effect,” which is why formulations that are ingested orally and must pass through the liver before entering the blood have less bioavailability than other formulations.
Liver enzyme CYP450 2C9 is thought to be primarily responsible for the formation of 11-OH-THC from THC and for the transformation of 11-OH-THC into THC-COOH, whereas CYP450 3A breaks down the other minor metabolites. After smoking cannabis, THC-COOH concentrations gradually increase, and are greater than THC concentrations within 30−45 min. This compares with ingestion of a single oral dose of Marinol® (10 mg THC), when plasma THC- COOH concentrations are higher than those of THC and 11-OH-THC 1 hour or more after dosing. Unlike after smoking, THC and 11-OH-THC concentrations are similar after oral THC administration. Much lower plasma 11-OH- THC concentrations (about 10% of THC concentrations) are found after cannabis smoking than after oral administration.
THC Metabolism – Outside the Liver
Other tissues, including brain, intestine, and lung, also metabolize THC. THC is metabolized in the brain with 11-OH-THC being the primary metabolite. Levels of 11-OH-THC can persist in the brain contributing to prolonged effects after administration of THC.
Additionally, CYP enzymes 2c9 and 3A4 are present in the intestines and contribute to the metabolism of THC into 11-OH- THC and other metabolites. Overall, the liver and intestinal metabolism of THC contribute to the significanty different effects of taking THC products orally vs. inhalation and buccal preparations.
11-OH-THC
Subsequent to oral ingestion, the gut and liver metabolizes THC into 11-OH-THC, a very potent THC metabolite of equal or greater potency than THC, It is formed at much higher levels after ingesting edibles compared with inhalation and buccal/sublingual administration. It has been reported that only 20% of inhaled THC is metabolized into 11-OH-THC whereas nearly 100% of orally ingested THC is converted to 11-OH-THC, mostly on its first pass through the liver when initially absorbed from the gut.
After taking cannabis orally, the average blood levels of 11-OH-THC vary from 25% of THC to more than 300% of THC levels, depending on the study and an individual’s metabolic differences. The 11-OH-THC is likely responsible for the stronger and longer-lasting drug effect of edibles. Given that some people will have 3 times higher blood levels of 11-OH-THC than THC after ingesting cannabis-based products, the therapeutic response, especially the psychoactive effects, may be quite different from inhaling them. The presence of high-fat food when ingesting THC significantly enhances time to peak plasma concentration (T max) and area under the curve (AUC0-24) for both THC and 11-OH-THC.
11-OH-THC, the Psychoactive and Therapeutic Effects of THC
11-OH-THC is likely responsible for many of the differences in the effects of oral ingestion of THC compared to inhaling or sublingual use. Whether 11-OH-THC contributes to qualitative or quantitative psychoactive differences from THC is as of yet unclear, although because 11-OH-THC enters the brain from the blood more quickly than THC, onset of effects are faster with 11-OH-THC. Experienced cannabis users will most often attest to a significantly different psychoactive experience from ingesting vs. inhaling the same cannabis product. (See: 11-OH-THC below).
11-OH-THC contributes to the effects of THC on thought processing, mood and euphoria, the “high” of marijuana, but may offer a calmer or different manifestation of the high. It may also contribute to some of the side effects of cannabis ingestion, including anxiety. Humans with 11- OH-THC concentrations in the 2–20 ng/mL concentrations will begin to exhibit cognitive and memory issues when tested, even without any physiological changes.
What is not yet known is what contribution 11-OH-THC makes toward other therapeutic effects, including those commonly contributed to THC. The full profile of benefits and side effects of 11-OH-THC is not known at this time.
Pharmacokinetics of 11-OH-THC
11-OH-THC diffuses into the brain more readily than THC does and its effects are perceived more rapidly than with THC. 11-OH-THC is subsequently metabolized into THC-COOH, which is inactive, and ultimately excreted into feces (65%) and urine (20%). THC is significantly metabolized with just one pass through the liver, the “first pass effect,” which is why formulations that are ingested orally and must pass through the liver before entering the blood have less bioavailability than other formulations. THC is also metabolized in the brain, with 11-OH-THC being the primary metabolite. Levels of 11-OH-THC can persist in the brain contributing to prolonged effects after administration of THC. As such, 11-OH-THC is a significant contributor to the effects of ingested THC products but not so much with vaped or buccal administered products.
After THC enters the blood, it quickly distributes from the blood to other body tissues and only a small fraction of it remains in the blood. The THC that remains available in the blood passes through the liver where it is converted to 11-OH-THC and other metabolites. However, the larger fraction of THC in other tissues does not contribute significantly to blood levels of 11-OH-THC and therefore, overall, not much 11-OH-THC is initially formed with inhalation. The levels of 11-OH-THC in the blood after smoking cannabis is only about 5% of THC levels, probably not enough to contribute significant psychoactive effects from the 11-OH-THC.
However, after taking cannabis orally, the average levels of 11-OH-THC vary from 25% of THC to more than 300% of THC levels, depending on the study and an individual’s metabolic differences. Given that some people will have 3 times higher blood levels of 11-OH-THC than THC after ingesting cannabis-based products, the therapeutic response, especially the psychoactive effects, may be quite different from inhaling them. Whether 11-OH-THC contributes qualitative or quantitative differences psychoactively from THC is as of yet unclear, although because 11-OH-THC enters the brain from the blood more quickly than THC, onset of effects are faster with 11-OH-THC.
THC Distribution in the Body
THC is widely distributed after reaching blood, particularly to fatty tissues, but less than 1% of an administered dose reaches the brain, while the spleen and body fat are long-term storage sites. THC and its metabolites are predominantly found in the plasma fraction of blood, where 95−99% are bound to lipoproteins. Because only about 10% of these cannabinoids are found in erythrocytes (red blood cells), whole-blood cannabinoid concentrations are approximately one-half the concentrations found in plasma specimens.
THC plasma concentrations decrease rapidly due to rapid distribution into tissues and metabolism in the liver. THC is highly lipophilic and is initially taken up by tissues that are highly perfused, such as the lung, heart, brain, and liver with what is considered a large volume of distribution of THC along with slow elimination from body stores. Studies of the distribution of THC into brain are especially important for understanding the relationships between THC dose and behavioral effects. After single intra-muscular injection of THC, maximal levels are reached in brain after 2−4 hours while after smoking THC, maximal brain levels are reached even faster. Importantly, THC concentrates in fat cells, especially with prolonged drug exposure. The ratio of fat to brain THC concentration is approximately 21:1 after 7 days of daily exposure, and 64:1 after 27 days. These fat stores are responsible for the prolonged finding of the THC metabolite THC-COOH in the urine for up to 3 months after chronic use of THC.
THC Metabolism and CBD
CBD is metabolized in the liver with primary oxidation to the inactive metabolite, THC-COOH. Like THC, CBD has a significant first-pass effect in the liver although, unlike THC, a large proportion of the dose is excreted unchanged in the feces. It has been reported that CBD inhibits THC metabolism but it is believed that the pharmacokinetics of THC are not meaningfully affected by CBD, except for a slight slowing of the metabolism of 11-OH- THC to THC-COOH. Co-administration of CBD does not significantly affect the total clearance, volume of distribution, or terminal elimination half-lives of THC or its metabolites.
Elimination of THC and Metabolites
The slow release of THC from fat storage compartments and significant enterohepatic circulation contribute to a long terminal half-life of THC in plasma, and even longer in urine. Up to 10−15% of a THC dose can be enterohepatically circulated (excreted into the feces, then reabsorbed into the blood again). Urinary THC-COOH concentrations drop rapidly until reaching about 20−50 ng/ml, where they may intermittently slightly increase or decrease depending on inconsistent release of stored cannabinoids in brain and fat tissues until the stores are finally completely depleted.
In chronic cannabis users who discontinue use, the THC-COOH metabolite may be detected in the urine for up to 30 days or even longer thus triggering a positive urine drug screen for marijuana use. It has been suggested that measuring THC and/or 11-OH-THC in the urine might provide a reliable marker of recent cannabis use, but it has been found that 11-OH-THC may be excreted in the urine of chronic cannabis users for a long period of time, beyond the period of pharmacologic effects and performance impairment. Additional research is necessary to determine the validity of estimating time of cannabis use from THC and 11-OH- THC concentrations in urine.
Interpretation of Cannabinoid Concentrations in Biological Fluids
Blood and Serum Levels
Compared to many other drugs, analysis of cannabinoids is difficult because THC and 11-OH-THC are highly lipophilic, and are present in very low concentrations in body fluids. Complex specimen matrices, i.e., blood, sweat, or hair, may require multi-steps to separate out the cannabinoids. THC and THC-COOH are predominantly found in the plasma fraction of blood and 95−99% are bound to lipoproteins. Only about 10% of either compound is found in blood cells so whole-blood cannabinoid concentrations are approximately one-half the concentrations found in plasma.
Interpreting drug effect, whether therapeutic effect or physical or mental impairment is particularly difficult due to a lack of correlation between drug effect and biologic levels as well as there being a wide variability from person to person, even with the same person at different times. It has been reported that the therapeutic window of pain relief occurs between 16-31 ng/ml plasma level of THC. However, it is likely that this determination is much over-simplified.
Prediction models have been proposed for estimation of cannabis exposure but there is controversy in the interpretation of cannabinoid results from blood analysis. THC effects appear rapidly after initiation of smoking. A dose-response relationship has been established for smoked THC and THC plasma concentrations and it is well-established that plasma THC concentrations begin to decline prior to the time of its peak effects.
Individual drug concentrations and ratios of cannabinoid metabolite to parent drug concentration have been suggested as potentially useful indicators of recent use. 45 min after smoking cannabis, the ratio (THC-COOH)/(THC) in the plasma has reported to be >1. It has been reported also that peak effects occur when THC and THC-COOH concentrations reach equivalency, within 30−45 min after initiation of smoking. Recent exposure (6−8 hours) and possible impairment have been linked to plasma THC concentrations in excess of 2−3 ng/ml.
However, interpretation is complicated by residual THC and THC-COOH concentrations found in blood of frequent cannabis users who may have residual plasma THC concentrations of 2 ng/ml some 12 h after smoking cannabis and significantly higher residual concentrations of THC-COOH may be found. These findings also likely apply to chronic use of all forms of cannabinoids. Furthermore, studies of drug effect and level of impairment do not correlate well with plasma levels due to differences in acute vs chronic exposure and other individual variables.
Urine Levels
Detection of cannabinoids in urine is indicative of prior cannabis exposure, but the long excretion half-life of THC-COOH in the body, especially in chronic cannabis users, makes it difficult to predict the timing of past drug use. In extreme cases, an individual’s urine may be positive for THC-COOH at concentrations >20 ng/ml up to 2 months or longer after last exposure. As such, a positive urine test for cannabinoids indicates only that THC exposure has occurred. The result does not provide information on the route of administration, the amount of drug exposure, when drug exposure occurred, or the degree of impairment.
Urinary THC-COOH concentrations drop rapidly until reaching about 20−50 ng/ml, where they may intermittently slightly increase or decrease depending on inconsistent release of stored cannabinoids in brain and fat tissues until the stores are finally completely depleted.
Oral-Fluid Testing
Oral fluid can be used for monitoring cannabinoid exposure and is being evaluated for the assessment of driving under the influence and for workplace drug testing. Adequate sensitivity is best achieved by testing for THC, rather than of 11-OH-THC or THC-COOH. The oral mucosa is exposed to high concentrations of THC during smoking which serves as the source of THC found in oral fluid. THC may be detected at low concentrations by radioimmunoassay for up to 24 h after use and longer by GC/MS analysis. In general, only minor amounts of drug and metabolites diffuse from the plasma into oral fluid and no measurable 11-OH-THC or THC-COOH are found in oral fluid for up to 7 days following cannabis smoking. Even following intravenous THC, no THC can be found in oral fluid.
Detection times of THC in oral fluid are shorter than in urine, and more indicative of recent cannabis use. Oral-fluid THC concentrations temporally correlate with plasma cannabinoid concentrations and behavioral and physiological effects, but wide intra- and inter-individual variation precludes the use of oral-fluid concentrations as indicators of drug impairment. THC may be detected at low concentrations by radioimmunoassay for up to 24 h after use and somewhat longer by GC/MS analysis.
NOTES
THC Pharmacokinetics
Absorption – THC
Inhalation (Smoking & Vaping) of THC
Smoking provides a very rapid and efficient means of delivery of cannabanoids from the lungs to the brain which can be intensely pleasurable and strongly reinforcing due to almost immediate drug exposure to the brain and central nervous system (CNS). Bioavailability with smoking ranges widely from 2−56%, due to intra- and inter-subject variability in smoking dynamics, including the number, duration, and spacing of puffs, hold time, and inhalation volume.
Peak THC plasma concentrations are reached about 9 minutes after smoking, dropping to about 60% and 20% of peak levels in 15 and 3o minutes, respectively. Depending on the potency of the inhaled product, mean plasma peak THC concentrations have been measured at 94.3, 107.4, and 155.1 ng/ml after smoking single cigarettes of 1.32, 1.97, or 2.54% THC potencies, respectively. These potencies are low; higher THC concentrations are found with higher potency cigarettes.
The clinical impact of THC is dose-dependent and may be related to plasma levels, but there is a great range of variability from one person to the next depending on the individual’s experience and frequency of use. Furthermore, the clinical effects of THC continue even after plasma levels drop to very low levels. Efforts to establish plasma levels of THC and/or its metabolites that correlate with physical and mental impairment how they have been established with alcohol have failed to be determined with marijuana.
Oral Ingestion of THC
There are fewer studies on the disposition of THC and its metabolites after oral use of cannabis/cannabinoids as compared to the smoked route. THC is readily absorbed when ingested but absorption is slower compared with smoking, with lower and more-delayed peak THC concentrations. Oral THC bioavailability is reported to be 10−20% due to variable absorption, degradation of drug in the stomach, CYP enzyme metabolism in the intestine and significant first-pass metabolism to active 11-OH-THC and inactive metabolites in the liver. In one study, patients dosed with either 15 mg (women) or 20 mg (men) of THC dissolved in sesame oil and contained in gelatin capsules reached peak THC plasma concentrations in 4−6 hours. In another study peak THC concentrations ranged from 4.4 to 11 ng/ml, occurring 1−5 hours following ingestion of 20 mg of THC in a chocolate cookie; the oral bioavailability was estimated to be 6%.
THC Metabolites (11-OH-THC & THC-COOH) with Ingestion
While the THC and other cannabinoids and pharmacologically active cannabis constituents are absorbed directly into the blood and to the brain after smoking, when ingesting cannabis or cannabinoids orally they undergo significant metabolism before reaching the blood and brain. This metabolism begins in the stomach and gut and continues in the liver before getting to the blood.
THC is primarily metabolized to 11-OH-THC, another psychoactive compound that contributes significantly to the psychoactive effects associated with cannabis use. Whether 11-OH-THC contributes to other therapeutic benefits is uncertain but it is known that 11-OH-THC crosses the blood-brain barrier even more quickly than THC. 11-OH-THC is then further metabolized into THC-COOH, a pharmacologically inactive compound which is then eliminated in the urine and feces. Thus, orally ingesting cannabis or THC results in higher blood levels of the 11-OH-THC metabolite compared with smoking.
THC concentrations decrease in brain tissue slower than in blood but the slowest THC elimination is seen in fat tissue, where THC may still be present for months after chronic use. 11-OH-THC is only found at high concentrations in the liver.
After taking cannabis orally, the average levels of 11-OH- THC vary from 25% of THC to more than 300% of THC levels, depending on the study. This compares with blood levels of 11-OH-THC in the blood after smoking cannabis that are only about 5% of THC levels, which is probably not enough to feel any effects from the 11-OH-THC.
The pharmacokinetics of an oral synthetic THC, (Marinol®), which is approved and available in the U.S., have been evaluated. In a study of the plasma concentrations of THC and its metabolites 11-OH-THC (active) and THC-COOH (inactive) were measured after ingestion of a single Marinol® capsule (10 mg of THC). Mean peak plasma concentrations of 3.8 ng/ml of THC (range 1.1 −12.7 ng/ml), 3.4 ng/ml of 11-OH-THC (range 1.2−5.6 ng/ml), and 26 ng/ml of THC-COOH (range 14−46 ng/ml) were found 1−2 hours after ingestion. Thus similar THC and 11-OH-THC concentrations were noted with consistently higher THC-COOH concentrations. Also, two THC peaks were frequently observed due to enterohepatic circulation.
After oral THC dosing, THC-COOH concentrations are generally higher than those of THC almost immediately after dosing, in contrast to what is found after smoking. Concentrations of 11-OH-THC also are higher than those of THC, with an extended detection window. It is suggested that ratio of (11-OH-THC)/(THC) >1 – 1.5 within 2 hours after consumption is a strong indications for oral intake of THC.
Due to low bioavailability of oral THC formulations, alternative routes of drug administration, including oromucosal or sublingual dosing and rectal administration, have been developed to improve the amount of delivered cannabinoids.
When THC is ingested orally as compared to smoking, onset of clinical effects are delayed, peak concentrations are lower, and duration of clinical effects generally are longer with a delayed return to baseline.
THC-containing bakery items and foods, i.e., hemp oil, beer, and other products, are commercially available for oral consumption in other states. Incidentally, hemp oil produced from cannabis seed, is an excellent source of essential amino acids and ω-linoleic and linolenic fatty acids (omega-3). The THC content depends upon the cannabis-seed-cleaning and oil-filtration processes but hemp oil without THC is available in Louisiana.
Oro-mucosal & Sublingual THC
Due to significant loss of bioavailability associated with oral ingestion and the breakdown of cannabis/cannabinoids by the stomach and liver, formulations designed to be absorbed from buccal (cheek) or sublingual (under the tongue) applications offer beneficial alternatives. Products of this nature, tinctures, are available in Louisiana in different formulations. Sativex® an oral spray prescription cannabis-based drug is approved in Canada for the treatment of neuropathic pain associated with multiple sclerosis, and in three European countries for a number of other indications.
Sativex® contains two standardized cannabis extract preparations, Tetranabinex®, which is high in THC, and Nabidiolex®, which is high in CBD. Sativex® contains equal proportions of Tetranabinex® and Nabidiolex®, and, hence, almost equal amounts of THC and CBD. THC and CBD represent approximately 70% of the product, with 5% of other cannabinoids, the remainder being terpenoids, flavonoids, sterols, alkanes, and other chemicals.
See Sativex information: Prescription Cannabis-based Products
Rectal THC
The bioavailability of the rectal route is approximately twice that of the oral route due to higher absorption and lower first-pass metabolism by the liver. Rectal administration of 2.5−5 mg of THC (Marinol®) produces maximum plasma concentrations of 1.1−4.1 ng/ml within 2−8 hours. This compares with oral administration of 10−15 mg doses resulting in THC concentrations that peak within 1−8 hours and range between 2.1 to 16.9 ng/ml.
Transcutaneous Cannabanoids: THC vs CBD
Topical administration is another route of cannabinoid dosing that avoids first-pass metabolism and improves THC bioavailability. Cannabinoids are highly hydrophobic, making transport across the aqueous layer of the skin the rate-limiting step in the diffusion process. Permeability of CBD has been found to be 10-fold higher than for THC. Additional research is planned with combinations of cannabinoids to increase drug absorption and hopefully reduce negative side effects seen with inhalation and oral dosing.
Metabolic Interactions with Other Drugs
The major cannabinoids, THC and CBD are both metabolized in the liver by the CYP450 enzymes 2C9 and 3A4. Drugs that inhibit these enzymes may enhance or prolong the effects of THC and CBD. Whether people with genetic variants of these enzymes may experience altered effects from cannabinoids is not fully known.
Genetic Polymorphisms of CYP2C9
One study published in 2009 evaluated the impact of the CYP2C9 polymorphisms on the pharmacokinetics of orally administered Δ9-tetrahydrocannabinol (THC). In patients with CYP2C9*3/*3 homozygotes (poor metabolizers), the median area under the curve of THC was threefold higher and that of the metabolite 11-nor-9-carboxy-9-tetrahydrocannabinol was 70% lower. CYP2C9*3 carriers also showed a trend toward increased sedation following administration of THC. Therefore, the CYP2C9*3 variant may influence both the therapeutic and adverse effects of THC.
The results of this study suggest that some individuals, likely <10% of the population, may be more sensitive to THC based on their CYP2C9 genetics but also that patients exposed to strong CYP2C9 inhibitors may also experience heightened impact with THC exposure.
Metabolic Effects of Medications on Cannabinoids
CYP3A4 Inhibitors Effect on Cannabinoids
Treatment with CYP3A4 inhibitors such as ketoconazole can produce an increase in Cmax and AUC of THC (1.2- and 1.8- fold, respectively). The increase in Cmax and AUC of the primary active metabolite of THC, 11-OH-THC, can be 3 and 3.6-fold, respectively, and of that of CBD (2- and 2-fold, respectively). Therefore, if concomitant drug treatment with CYP3A4 inhibitors (e.g. itraconazole, ritonavir, clarithromycin) is started or stopped during treatment with cannabinoids, a dose adjustment may be required.
CYP3A4 Inducers Effect on Cannabinoids
Treatment with CYP3A4inducers such as rifampicin can reduce the Cmax and AUC of THC (by 40% and 20%, respectively), 11-OH-THC (by 85% and 87%, respectively), and CBD (by 50% and 60%, respectively). Therefore, concomitant treatment with strong enzyme inducers (e.g. rifampicin, carbamazepine, phenytoin, phenobarbital, St John’s Wort) should be avoided whenever possible. Again, if concomitant drug treatment with CYP3A4 inducers (e.g. rifampicin, carbamazepine, phenytoin, phenobarbital, St John’s Wort) are started or stopped during treatment with cannabinoids, a dose adjustment may be required within two weeks of starting or stopping the inducer.
Metabolic Effects of Cannabinoids on other Medications
CYP2D6
CBD has been identified as a potent inhibitor of CYP2D6 which may have significant impact on the metabolism of medications that are broken down by CYP2D6, including hydrocodone (Norc0, Vicodin, Zohydro, Hysingla) and other opioids including tramadol and codeine. As such, use of CBD with tramadol or codeine, which are pro-drugs that require metabolism by CYP2D6 to form their active analgesic metabolite to work, may significantly reduce the analgesic effectiveness of these opioids. While CYP2D6 metabolizes hydrocodone to hydromorphone, it is not believed that inhibition of CYP2D6 significantly affects the analgesic benefit of hydrocodone. Other common medications that may be affected include antidepressants.
CBD is also a potent inhibitor of CYP3A enzymes, especially CYP3A5. While CYP3A4 is the dominant CYP3A isoform in the metabolism of most drugs, some drugs such as diltiazem (Cardizem), are more efficiently metabolized by CYP3A5 than by CYP3A4. Also, CYP3A5 is a major isoform of CYP3A found in extrahepatic tissues that plays an important role in the metabolism of endogenous and exogenous compounds in these tissues. Thus, the inhibition of CYP3A5 by CBD may cause interactions with other medications and may also disturb normal metabolism of endogenous compounds.
Since cannabinoids are readily distributed in various tissues due to a high lipophilicity, tissue concentrations of CBD may be even higher than the blood concentration, suggesting that the inhibition of CYP3A by CBD might occur during and/or after marijuana smoking.
Resources:
National Academy of Sciences
This website appears to be good resource for exploring medical marijuana.
References:
Medical Marijuana – Driving
- Establishing legal limits for driving under the influence of marijuana – 2014
- Medical Marijuana and Driving – a Review – 2014
Medical Marijuana – Opioids
- Impact of co-administration of oxycodone and smoked cannabis on analgesia and abuse liability. – PubMed – NCBI
- Cannabinoid–Opioid Interaction in Chronic Pain
- Synergistic interactions between cannabinoid and opioid analgesics. – PubMed – NCBI
- FDA approves CBD drug – Epidiolex – The Washington Post
Medical Marijuana – Opioid Drug Interactions
- The Effect of CYP2D6 Drug-Drug Interactions on Hydrocodone Effectiveness – 2014
- Cannabidiol, a Major Phytocannabinoid, As a Potent Atypical Inhibitor for CYP2D6 – 2011
- Potent inhibition of human cytochrome P450 3A isoforms by cannabidiol. – Role of phenolic hydroxyl groups in the resorcinol moiety – 2011
- Interindividual variation in the pharmacokinetics of Delta9-tetrahydrocannabinol as related to genetic polymorphisms in CYP2C9. – PubMed – NCBI
- A Marijuana-Drug Interaction Primer – Precipitants, Pharmacology, and Pharmacokinetics – 2019
Medical Marijuana – Pharmacokinetics
- Pharmacokinetics of cannabinoids – PubMed – 2005
- Human Cannabinoid Pharmacokinetics – 2007
- A tale of two cannabinoids: the therapeutic rationale for combining tetrahydrocannabinol and cannabidiol. – PubMed – NCBI
- Cannabis and cannabis extracts – greater than the sum of their parts? – 2001
- Cannabinoids and Cytochrome P450 Interactions. – PubMed – NCBI
- Adverse effects of medical cannabinoids – a systematic review – 2008
- Cannabimimetic effects modulated by cholinergic compounds. – PubMed – NCBI
- Antagonism of marihuana effects by indomethacin in humans. – PubMed – NCBI
- Pharmacokinetics and pharmacodynamics of cannabinoids. – PubMed – NCBI
- Clinical Pharmacodynamics of Cannabinoids – 2004
- Quality Control of Traditional Cannabis Tinctures – Pattern, Markers, and Stability – 2016
- Exogenous cannabinoids as substrates, inhibitors, and inducers of human drug metabolizing enzymes: a systematic review. – PubMed – NCBI
- Pharmacology of Cannabinoids
- The Cannabis sativa Versus Cannabis indica Debate – An Interview with Ethan Russo, MD – 2016
- Human Metabolites of Cannabidiol – A Review on Their Formation, Biological Activity, and Relevance in Therapy 2016
- A Comprehensive Review on Pharmacotherapeutics of Herbal Bioenhancers – 2012
- The effects of black pepper on the intestinal absorption and hepatic metabolism of drugs. – PubMed – NCBI – 2011
- Piperine-pro-nanolipospheres as a novel oral delivery system of cannabinoids: Pharmacokinetic evaluation in healthy volunteers in comparison to buc… – PubMed – NCBI – 2017
- A Systematic Review on the Pharmacokinetics of Cannabidiol in Humans
- Clinical_Pharmacokinetics_of_Cannabinoids
- Δ9-Tetrahydrocannabinol (THC), 11-Hydroxy-THC, and 11-Nor-9-carboxy-THC Plasma Pharmacokinetics during and after Continuous High-Dose Oral THC – 2009
- MARINOL® (Dronabinol) product info – 2017
- Human Pharmacokinetic Parameters of Orally Administered Δ 9-Tetrahydrocannabinol Capsules Are Altered by Fed Versus Fasted Conditions and Sex Differences – PubMed
- Pharmacokinetics and pharmacodynamics of cannabinoids. – 2018
- A Marijuana-Drug Interaction Primer – Precipitants, Pharmacology, and Pharmacokinetics – 2019
Medical Marijuana – Pharmacogenetics
Medical Marijuana – Cannabidiol (CBD) Pharmacokinetics
- Human Cannabinoid Pharmacokinetics – 2007
- A tale of two cannabinoids: the therapeutic rationale for combining tetrahydrocannabinol and cannabidiol. – PubMed – NCBI
- Human Metabolites of Cannabidiol – A Review on Their Formation, Biological Activity, and Relevance in Therapy 2016
- A Comprehensive Review on Pharmacotherapeutics of Herbal Bioenhancers – 2012
- The effects of black pepper on the intestinal absorption and hepatic metabolism of drugs. – PubMed – NCBI – 2011
- Piperine-pro-nanolipospheres as a novel oral delivery system of cannabinoids: Pharmacokinetic evaluation in healthy volunteers in comparison to buc… – PubMed – NCBI – 2017
- A Systematic Review on the Pharmacokinetics of Cannabidiol in Humans
Medical Marijuana – ∆9-tetrahydrocannabinol (THC) Pharmacokinetics
- 11-Nor-9-carboxy-∆9-tetrahydrocannabinol – a ubiquitous yet underresearched cannabinoid. A review of the literature
- A Marijuana-Drug Interaction Primer – Precipitants, Pharmacology, and Pharmacokinetics – 2019
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.