“ Drunkeness brings pallor and sagging cheeks, sore eyes, and trembling hands that spill a full cup, of which the immediate punishment is a haunted sleep and unrestful nights…”
– Pliny the Elder: Gaius Plinius Secundus
Naturalis Historia 79 AD
Alcohol, Pain & Opioids
The use of alcohol by patients with chronic pain requires special understanding, even for those individuals who don’t take opioids for their pain. For those who do take opioids for chronic pain, it is even more important that they understand these specific concerns and precautions if they are to drink alcohol.
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
.
Alcohol – Guidelines for Use
Alcohol consumption can be roughly divided into two categories: low risk and hazardous. Low risk consumption is at a level unlikely to cause any problems. Hazardous consumptiom has degrees of severity but starts with the point at which one’s alcohol blood level would create impairment. This impairment could be mental, one of judgement or decision-making, or it could be physical, with impaired coordination, reaction time or balance. The cross-over from low risk to hazardous is generally associated with a blood level of about 0.8 ng/ml (80mg/dL), the usual marker of driving impairment.
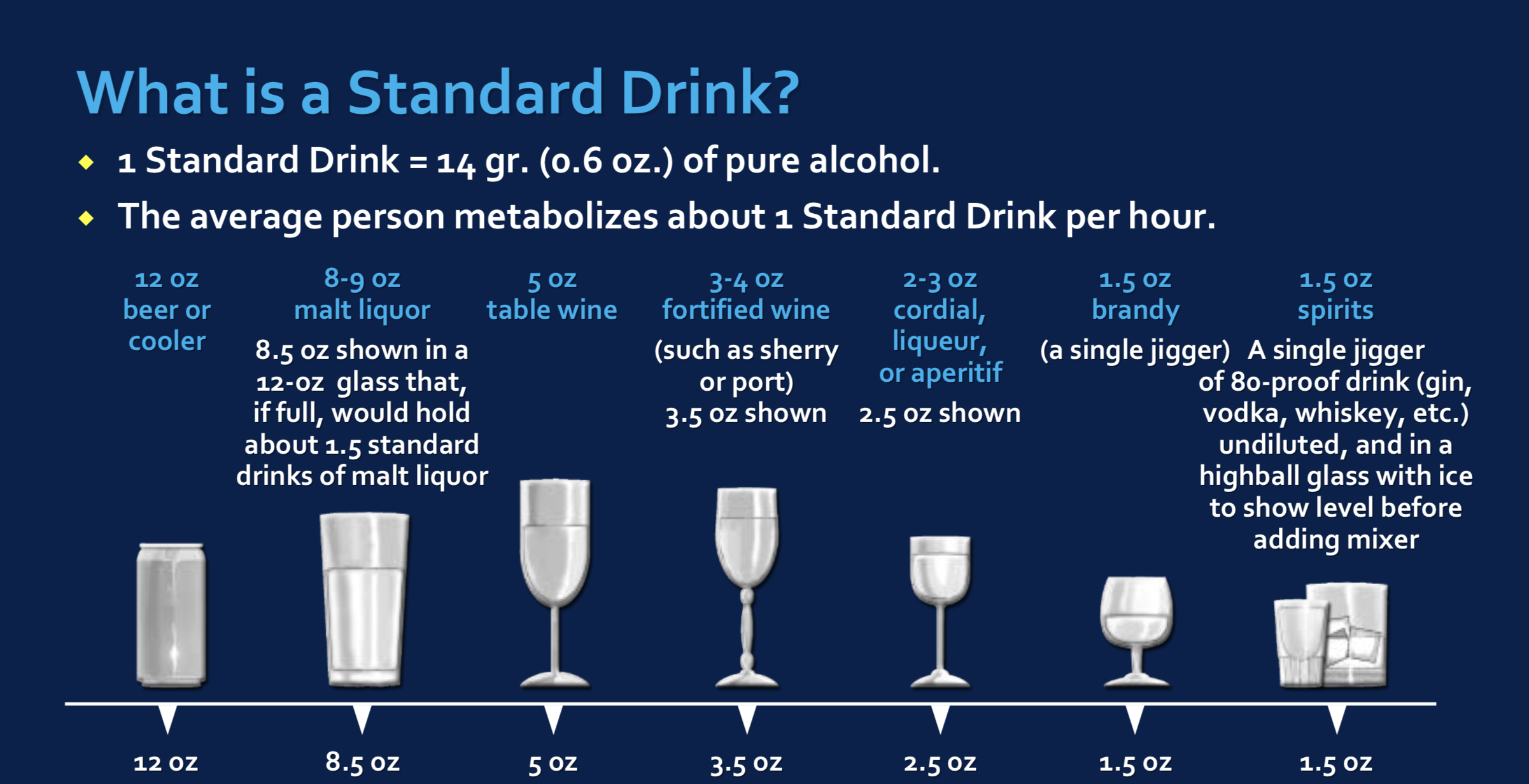
Different guidelines have been proposed to direct safe alcohol consumption but for simplicity, the following recommendations are advised, based on the concept of a “standard drink,” one that contains 14 gms of alcohol (see below). In the absence of compromising medical conditions or use of medications that could contribute to further impairment:
Men: Up to 3 standard drinks/day; no more than 5 drinking days/week; no more than 14 drinks/week
Women: Up to 2 standard drinks/day; no more than 5 drinking days/week; no more than 7 drinks/week
But, for those taking medications such as opioid pain medications or benzodiazepines like Xanax or Klonopin that might contribute impairment, further precautions must be engaged. Ideally, total abstinence from alcohol is advised for those taking multiple potentially compromising medications.
However, for those taking opioid medications who choose to drink, the following guidelines are advised:
- Be open, discuss your use of alcohol with your physician.
- Abstain from alcohol for 6 hours after taking a short-acting opioid such as a Norco or Percocet.
- Abstain from alcohol for 12 hours after taking a long-acting opioid such as 12-hr extended release morphine.
- Abstain from alcohol if you take long-acting opioids designed for 24-hour duration use
- Abstain from alcohol if you use Fentanyl patches
- Do not ever drink alcohol with an extended-release opioid, this may cause the immediate release of the opioid and the potential for overdose.
- For each standard drink consumed, wait 2 hours before resuming your opioid medication.
- Men: Limit alcohol consumption to 1-2 standard drinks per occasion per day.
- Women: Limit alcohol consumption to 1 standard drink per occasion per day.
- Do not drink alcohol in the evening or at night if you are at risk for sleep apnea, regardless if you treat with CPAP.
- Do not resume pain medications if you continue to feel any “buzz” or other impairment from alcohol.
- Do not drink alcohol if you are taking Soma or benzodiazepines (Xanax, Klonopin, Valium, Restoril etc).
Binge Drinking
A “binge” is defined as:
Men: 5 drinks in 2 hours
Women: 4 drinks in 2 hours
Alcohol – Men vs. Women: Why the Difference?
Guidelines directed at alcohol consumption consistently advise reduced intake for women compared with men but there is no evidence that women become more impaired than men with the same blood levels. However, there are several factors that contribute to women having higher blood levels with less alcohol intake compared to men. When ingested, alcohol is distributed throughout the water-based compartments of the body, primarily including blood and muscle tissues, not bone or fat. Because women in general are smaller with less muscle mass than men, the alcohol is distributed to a smaller water-based body volume so concentrations are higher. In addition, women have less alcohol dehydrogenase enzyme in their liver, the enzyme that breaks down alcohol, so it takes women longer for their bodies to clear the alcohol consumed.
The Rule of 20’s:
MEN:
Each drink adds 20 mg/dL to blood alcohol level.
WOMEN:
Each drink adds 40 mg/dL to blood alcohol level.
Remember: A blood level of 80mg/dL establishes alcohol impairment and will earn a DUI
Alcohol and Pain
Historically, alcohol has been used to manage acute pain for thousands of years. It has been reported that as many as 25% of people experiencing pain self-medicate with alcohol. However, it is important to understand the conditions in which the use of alcohol in those with pain, especially chronic pain, may place those people at risk for engaging in hazardous drinking and lead to vulnerability in becoming an alcoholic. With approximately 15.1 million American adults suffering from alcohol use disorder (AUD) and 100 million suffering from chronic pain, the co-occurrence of AUD and chronic pain is common although their relationship is complex. It has been theorized that alcoholism may in some cases be viewed as a chronic pain disorder.
It is well established that people with chronic pain tend to drink more heavily than those without pain. This may be due to inadequate pain control, sleep problems, anxiety, depression or other mood disorders. While alcohol may temporarily reduce acute pain, there is evidence that chronic alcohol use increases sensitivity to painful stimulation. People with chronic pain conditions are more likely to have family members with drinking problems. Studies also suggest that people who do not have drinking problems, but have a positive family history of alcoholism, are more sensitive to painful stimulation than those having no family history of alcoholism. There appears to be a relationship, though not entirely understood, between chronic pain and alcoholism.
An important aspect of the pain-alcohol link lies in how alcohol use reinforces pain transmission and perception. It is theorized that neuroreceptor systems may play a dual role in reinforcement of alcohol use and the transmission of pain which has implications for pain-related problems to lead to compulsive alcohol seeking. As alcohol use becomes more frequent in the presence of chronic pain, the abstinence period after drinking results in a withdrawal-associated condition of hyperalgesia, in which the experience of pain becomes magnified over the usual pain. Commonly accompanying chronic pain are conditions of stress and/or anxiety and mood disorders including depression. The inter-related neurocircuitry of pain, stress and mood along with an accompanying condition of “reward deficiency” (see below) contributes to the compulsive drive to resume alcohol use which will improve the sense of well-being and reduce pain.
The basis of reward deficiency theory is that humans are reward-driven creatures and that hehavior is heavily influenced ty the reward associated with that behavior. Hunger drive is driven by the reward of feeling satiated or full after eating. Sexual drive is driven by completion of the sexual act. Emotional drives are driven by the emotional reward of expressing the emotion, be it anger or passion. When an individual experiences chronic or extremely stressful emotional or psychiatric disruptions to their psychological well-being, they become “reward deficient,” manifest by imbalance in the reward center of the brain.
The role of the Reward Deficiency Syndrome (RDS) in chronic pain and addiction, including alcoholism has led to exploration of genetic factors that impact risk for these conditions. There is a significant contribution of genetic variants impacting chronic pain and the risk for alcoholism. Genes that have been identified as playing significant overlapping roles in both chronic pain and alcoholism include COMT, OPRM1 and DRD2. Understanding an individual’s genetic risks for RDS including these genes can provide insight into treatment options that may reduce chronic pain and alcohol cravings. These treatment options include personalized nutritional supplements based on the individual’s specific genetic variants.
See:
Genetic Testing: Individual DNA Alleles
Neurobiology of Pain
Reward Deficiency Syndrome (RDS)
Reward Deficiency Syndrome (RDS) & Addiction
Reward Deficiency Syndrome (RDS) & Chronic Pain
Resources:
References:
Alcohol – Pain
- Alcohol dependence as a chronic pain disorder – 2012
- Comorbidity of alcohol use disorder and chronic pain – Genetic influences on brain reward and stress systems – 2017
Alcohol – Testing
- Levels and Types of Alcohol Biomarkers
- Using Alcohol Biomarkers to Guide Pharmacotherapy for Alcohol Use Disorder
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.