“Who, except the gods, can live time through forever without any pain?”
Aeschylus (BC 525-BC 456) Greek dramatist.
Prescription Medications:
Neurobiology of Opioids
The following information is provided for those interested in learning more about how opioids work and how certain opioids differ from one another. Understanding these differences allows for more informed selections of specific opioids to individualize someone’s pain management. The content of this page is expected to evolve as research progresses and more information becomes available. Check back from time to time…
It is recommended to first read the following sections to become familiarized with some of the terms and concepts related here:
- Neurobiology of Pain
- Neuropathic Pain
- Opioids
- Opioid Tolerance
- Opioid Induced Hyperalgesia (OIH)
- Opioid Withdrawal
- Withdrawal Induced Hyperalgesia (WIH)
Individual opioids:
- Buprenorphine (for Pain)
- Levorphanol
- Methadone (for Pain)
- Tapentadol (Nucynta)
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
.
Neurobiology of Opioids
Receptors and Neurotransmitters
Receptors are cellular structures, usually a complex protein molecule found on the surface of a cell, that interacts or binds with a chemical which then triggers a response. These chemicals may be neurotransmitters (in the nervous system), hormones or drugs. A chemical or drug that triggers a reaction with a receptor is referred to as an “agonist,” while one that blocks the activity of a receptor is referred to as an “antagonist.” In the world of pain, there are a handful of receptors that play prominent roles, most notably the opioid receptors which interact with both endogenous opioids (manufactured by the body) and exogenous opioids (drugs and medications).
Besides the opioid receptors, another receptor that plays a significant roles in pain is the NMDA receptor. The list of receptors important in pain is not limited to only these few receptors but these are the receptors that, when understood, can provide insights towards better choices of opioids. Thus, understanding the nature of a person’s pain and understanding the difference in how medications work allows for tailoring an individualized pain management plan to optimize pain control.
What makes one opioid different from another is how effectively it binds with the opioid receptors and how it may interact with other receptors such as the NMDA receptors. Some opioids also increase activity of certain neurotransmitters which can result in reduced pain.
Opioid Receptors
Opioid pain medications affect the nervous system by interacting with receptors on nerve cells, most importantly the opioid receptors. It is important to appreciate the fact that opioids interact with receptors with different degrees of affinity as well as different degrees of potency. Thus some opioids are stronger than others because of how they interact with opioid receptors. There are 3 types of opioid receptor: mu, kappa and delta. How a particular opioid interacts with each of these receptors determines its benefits and its side effects.
Mu-Opioid Receptors
The mu-opioid receptors are the most prominent in providing pain control (analgesia) and the receptors where most opioids have their greatest impact including both the endogenous “endorphin” opioids as well as prescription opioid medications. Mu-opioid receptors are responsible for analgesic benefits of opioids but also nausea, sedation, euphoria, pinpoint pupis, respiratory depression and constipation. Triggering the mu-receptor is also rewarding, creating a desire to repeat the activity that stimulated the mu-opioid receptor.
While all prescription opioids typically used to treat pain are agonists for the mu-opioid receptors, the prescription opioids that are significant agonists only with the mu-opioid receptor are:
codeine
hydrocodone
oxycodone
morphine
methadone
Kappa-Opioid Receptors
The kappa-opioid receptors also play a role in providing analgesia, although their role is less understood. Stimulating the kappa-opioid receptors provides analgesia but also results in the potential for dysphoria (feeling bad, the opposite of euphoria), distorted perceptions and pinpoint pupils. The kappa-opioid receptors, unlike the mu-opioid receptors, are aversive or non-reinforcing. When opioids also trigger the kappa-opioid receptors in addition to the mu-opioid receptors, they can sometimes offer greater pain benefit. This is especially true when introduced as a new opioid following the development of tolerance to an opioid with only mu-opioid activity (see “cross-tolerance” below).
Prescription opioids that are significant kappa-opioid agonists include:
- oxymorphone (weak)
- fentanyl (weak?)
- hydromorphone (strong?)
- levorphanol (strong)
Prescription opioids that are significant kappa-opioid antagonists include:
- Buprenorphine
Delta-Opioid Receptors
The delta-opioid receptors are the least understood and little information is available as to their specific role in analgesia at this time. In addition to providing analgesia, they may also offer some degree of antidepressant benefit.
Prescription opioids that are significant delta-opioid agonists (?) are:
- levorphanol
- buprenorphine
- fentanyl (weak?)
ORL Receptors
The ORL-1 receptors are related to opioid receptors and are relatively new in our understanding and little information is available as to their specific role in analgesia. There is some evidence that activation of ORL-1 receptors has effects in neuropathic pain.
More information soon…
Prescription opioids that are significant ORL-1-opioid agonists (?) are:
- buprenorphine
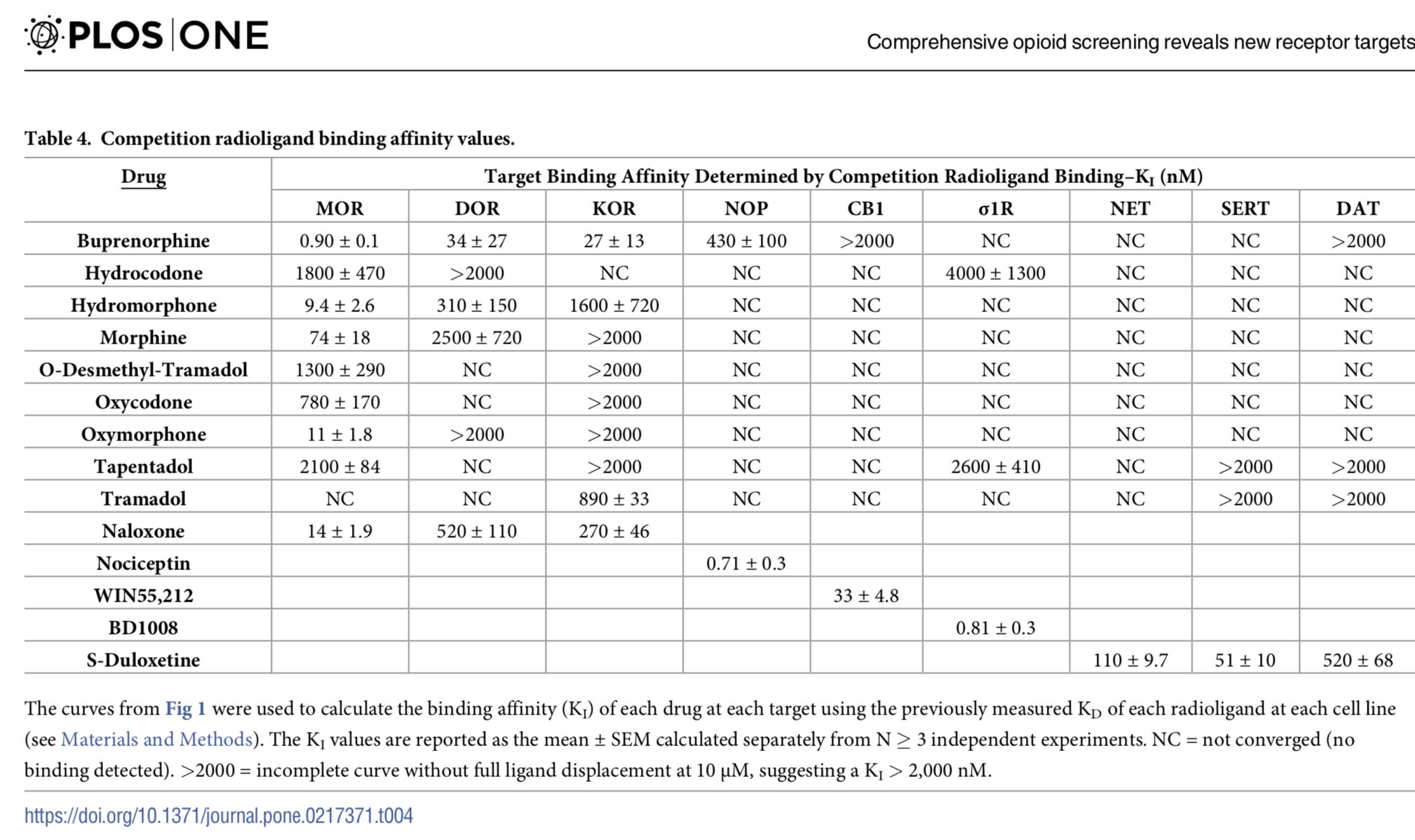
Affinity to Opioid Receptors
Different opioids have different affinities to opioid receptors, meaning that the strength of binding to opioid receptors is stronger in some opioids than others. Each opioid’s affinity varies for each opioid receptor and this affinity is significant in certain circumstances. For example, because buprenorphine is an opioid with strong affinity for the mu-opioid receptor, it will block the action of another opioid with less affinity when taken at the same time. This quality makes it an effective deterrent when used for treating opioid addiction because it will block the euphoria potentially offered by a second opioid, but it also will block the additive pain relieving qualities of a supplemental opioid taken together with buprenorphine. This is why “break through” opioids are ineffective when a patient takes buprenorphine for pain. This circumstance represents a challenge when treating a patient on buprenorphine for pain that is not relieved by their buprenorphine. To learn how to address this problem, one must treat with another opioid with greater affinity for the mu-opioid receptor than buprenorphine (see: “Buprenorphine for Pain”).
NMDA Receptors
The N-methyl-D-aspartate (NMDA) receptor is another receptor found in nerve cells. It is activated when neurotransmitters such as glutamate bind to it. It remains uncertain how NMDA and opioid receptors interact but blocking the NMDA receptor appears to reduce the development of opioid tolerance and opioid induced hyperalgesia (see OIH). Some medications that have activity inhibiting NDMDA receptors benefit neuropathic (nerve) pain, especially peripheral neuropathy as well as fibromyalgia.
The clinical application of blocking NMDA activity remains elusive with the literature lacking clear, definitive answers. However, what is known is that some opioids have NMDA blocking (antagonist) activity and these opioids offer advantages when treating neuropathic pain. The opioid that currently appears to provide the most benefit for nerve pain related to blocking NMDA is levorphanol, although methadone and buprenorphine are also thought to be weak NMDA antagonists.
In addition to opioids with NMDA antagonist activity, other medications are known NMDA antagonists including ketamine (see Ketamine) and dextromethorphan. Ketamine is a very effective nerve pain medication when used topically. Ketamine can also be very effective when used intravenously but side effects limit its use in this way. Dextromethorphan (Delsym, Robitussin DM), an OTC cough suppressant, is another NMDA antagonist (weak, but equipotent to the NMDA activity of methadone) which may offer some clinical applications in the treatment of opioid withdrawal and in the prevention of opioid tolerance and opioid induced hyperalgesia. (Additional information regarding dextromethorphan will be forthcoming on this web site in the near future).
Neurotransmitters (serotonin and norepinephrine)
In the processing of pain, the communication of pain signals from nerves involves the stimulation of receptors on the surface of nerves by chemicals called neurotransmitters. Neurotransmitters are released from one nerve which then attach to the receptors on a second nerve which triggers a response. After stimulating this second nerve, the neurotransmitters may be recycled by being reabsorbed (reuptake) by the first nerve or they can be metabolized (broken down) by enzymes such as COMT or MAO (more about these enzymes later). The space between two interacting nerves where all of this happens is called a “synapse.” As noted in the “neurobiology of pain” page, the descending pathways from the brain to the spinal cord which inhibit pain involve the neurotransmitters serotonin and norepinephrine. Increasing the levels of these two neurotransmitters is the basis for the benefit of the SNRI medications, duloxetine (Cymbalta), milnaciprin (Savella) and venlafaxine (Effexor) in the treatment of fibromyalgia and neuropathic pain. These SNRIs (Serotonin and Norepinephrine Reuptake Inhibitors) act on these pain-inhibiting descending pathways by blocking the reuptake of these neurotransmitters, keeping them in the synapse longer, thereby increasing their activity and pain benefit .
In addition to the SNRIs, there is good evidence some opioids also have SNRI activity, thus improving neuropathic pain via an additional mechanism separate from opioid or NMDA receptor activity. Opioids with SNRI activity may also possibly provide some mood improvement by reducing anxiety and depression (see: buprenorphine and PTSD).
The opioids known to have SNRI activity include:
tramadol (Ultram)
- tapentadol (Nucynta)
- levorphanol
- methadone
- buprenorphine (Butrans, Belbuca, Suboxone, Zubsolv, Bunavail)
References:
Opioids – Individual
Opioids – Buprenorphine (Butrans, Belbuca, Suboxone, Subutex, Zubsolv, Bunavail)
Opioids – Fentanyl (Duragesic)
Opioids – Hydrocodone (Norco, Vicodin)
Opioids – Hydromorphone (Dilaudid, Exalgo)
Opioids – Levorphanol
Opioids – Methadone
Opioids – Oxycodone (Percocet, Oxycontin)
Opioids – Morphine (MSIR, MSER, MSContin)
Opioids – Tapentadol (Nucynta)
Opioids – Tramadol (Ultram, Ultracet)
Opioids – Neuropathic (Nerve) Pain
Opioids Overdose: Tolerance
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.