Acupuncture:
Depression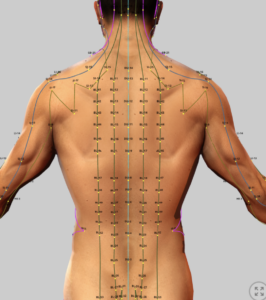
Patients often inquire about what supplement brands and products are recommended Accurate Clinic. In an effort to field these questions, four well known supplement brands are presented here for comparison. This is not meant to be an exhaustive review, but rather a simple resource for those looking for guidance only.
See:
- Traditional Chinese Medicine (TCM)
- TCM – Chinese Herbal Medicine (introduction)
- TCM – Acupuncture Introduction
- Acupuncture – Anxiety
- Acupuncture – Depression
- Acupuncture – Insomnia
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
Definitions and Terms Related to Pain
Acupuncture –Depression
Acupuncture as a Treatment for Depression: A Comprehensive Review with a Focus on Chronic Pain-Related Depression
Introduction
Depression, affecting over 280 million people globally, is a leading cause of disability, characterized by persistent sadness, anhedonia, and impaired daily functioning. In the United States, its lifetime prevalence is approximately 20%,. Depression frequently coexists with chronic pain, with 18–85% of chronic pain patients experiencing depressive symptoms. This comorbidity, often termed chronic pain-related depression (CPRD), exacerbates pain perception, reduces treatment efficacy, and impairs quality of life, creating a bidirectional relationship where pain worsens depression and vice versa.
Conventional treatments, including antidepressants (e.g., selective serotonin reuptake inhibitors [SSRIs], serotonin-norepinephrine reuptake inhibitors [SNRIs]) and psychotherapy (e.g., cognitive-behavioral therapy [CBT]), are effective for many but have non-response rates up to 30%, side effects (e.g., weight gain, sexual dysfunction), and limited accessibility, particularly for complex cases involving chronic pain.
Acupuncture, a cornerstone of Traditional Chinese Medicine (TCM) for over 2,000 years, has emerged as a promising adjunctive therapy for depression since its introduction to Western medicine in the 1970s. The National Institutes of Health’s 1997 consensus statement endorsed its use for various conditions, including depression. Acupuncture modalities—manual acupuncture (MA), electroacupuncture (EA), laser acupuncture (LA), and auricular acupuncture (AA)—stimulate specific acupoints to modulate neuroendocrine pathways, offering a safe, non-pharmacological option with minimal side effects.
This treatise evaluates acupuncture’s efficacy and safety for depression, with a specific focus on CPRD, compares it to standard and alternative treatments, and explores synergistic approaches with CAM nutraceuticals, emphasizing its role in integrative pain management. The following information synthesizes evidence from systematic reviews, meta-analyses, and randomized controlled trials (RCTs) on acupuncture for depression, with a focus on CPRD.
However, evidence is limited by high risk of bias (e.g., inadequate blinding), regional skew (mostly Chinese studies), and inadequate reporting of adverse events. Long-term follow-up data are sparse, necessitating further research to confirm sustained benefits.
Key sources include:
- Armour et al. (2019), a systematic review and meta-analysis of 29 RCTs (2,268 participants) evaluating acupuncture for major depressive disorder (MDD).
- Cheng et al. (2022), a systematic review of 83 meta-analyses assessing interventions for depressive symptoms in chronic pain.
- You et al. (2021), a systematic review and meta-analysis of 8 RCTs (636 participants) on acupuncture for CPRD.
- Chen et al. (2022), a systematic review and network meta-analysis of 22 RCTs (2,391 participants) on acupuncture for depression.
- Additional studies from the literature to contextualize acupuncture’s role, mechanisms, and synergy with nutraceuticals.
Acupuncture for Depression
General Depression
Acupuncture demonstrates clinical benefits in reducing depression severity across various modalities. A comprehensive review of 29 RCTs found acupuncture effective compared to usual care, sham acupuncture, and as an adjunct to antidepressants. Manual acupuncture outperformed sham interventions, suggesting effects beyond placebo, while acupuncture combined with SSRIs or SNRIs showed greater benefits than antidepressants alone.
Electroacupuncture combined with antidepressants achieved superior outcomes compared to controls or antidepressants alone, followed by manual acupuncture plus antidepressants and manual acupuncture alone.
Acupuncture’s benefits are attributed to its modulation of serotonin, noradrenaline, and adenylate cyclase pathways, similar to antidepressants, but with fewer side effects.
Chronic Pain-Related Depression (CPRD)
For CPRD, acupuncture shows promise as a safe and effective therapy, particularly when combined with antidepressants. A meta-analysis of 8 RCTs found that acupuncture alone was comparable to oral antidepressants in reducing depression severity and pain intensity, but with fewer side effects.
Acupuncture combined with antidepressants was more effective than antidepressants alone for both depression and pain outcomes, suggesting a synergistic effect. Common pain conditions included fibromyalgia, axial pain (e.g., low back pain), and arthritis
Acupuncture’s mechanisms in CPRD involve modulation of shared neural circuits (e.g., cortex, hippocampus) and neurotransmitters (e.g., 5-HT1A/1B receptors), reducing both pain and depressive symptoms.
A broader review of interventions for depressive symptoms in chronic pain found limited evidence for acupuncture due to under-synthesis compared to psychological or pharmacological interventions. While fluoxetine and web-based psychotherapy showed moderate effects for fibromyalgia-related depression, acupuncture’s effects were less robustly documented, highlighting a research gap. Acupuncture’s safety profile, with only mild adverse events (e.g., headaches, dizziness), supports its use in CPRD, particularly for patients intolerant to antidepressants or seeking non-pharmacological options.
Alternative Treatments for Depression
Several alternative treatments are effective for depression:
- Psychological Interventions: CBT, acceptance and commitment therapy (ACT), and interpersonal therapy are widely used, with CBT showing robust effects in reducing depression severity, particularly in fibromyalgia and mixed chronic pain. Web-based psychotherapy is effective for fibromyalgia-related depression, offering accessibility advantages, especially post-COVID-19.
- Pharmacological Interventions: Fluoxetine (Prozac) and other SSRIs/SNRIs (Cymbalta) are first-line treatments, with moderate effects in fibromyalgia-related depression. However, side effects (e.g., nausea, sedation, sexual dysfunction) and non-response rates limit their utility, particularly in CPRD, where pain may reduce antidepressant effectiveness.
- Mind-Body Interventions: Exercise (e.g., for arthritis) and music therapy (for general chronic pain) show benefits for depressive symptoms,. Yoga and mindfulness-based stress reduction also demonstrate effectiveness in reducing depression in chronic pain populations.
- Other CAM Therapies: Herbal medicines (e.g., Hypericum perforatum [St. John’s wort]) and meditation are used for depression, with variable levels of evidence. St. John’s wort shows efficacy comparable to SSRIs for mild-to-moderate depression but requires caution due to drug interactions.
Comparison of Acupuncture with Standard Treatments
Standard treatments for depression include pharmacotherapy and psychotherapy:
- Antidepressants: SSRIs (e.g., fluoxetine, sertraline) and SNRIs (e.g., duloxetine) are first-line, reducing depression severity in 50–70% of patients. In CPRD, fluoxetine is effective for fibromyalgia, but side effects and reduced efficacy in severe pain limit its use. Acupuncture alone is comparable to antidepressants for CPRD, with fewer adverse events, while acupuncture combined with antidepressants outperforms antidepressants alone, suggesting a complementary role.
- Psychotherapy: CBT and interpersonal therapy are effective, with CBT showing sustained benefits up to two years post-treatment. In CPRD, web-based CBT is effective for fibromyalgia, but access to qualified therapists is limited. Acupuncture integrates well with psychotherapy, enhancing outcomes in residential settings, as seen in addiction medicine with the NADA protocol.
- Comparison: Acupuncture offers a safer profile than antidepressants, avoiding risks like dependence or nervous system damage. Unlike psychotherapy, acupuncture addresses both physical (pain) and psychological (depression) symptoms simultaneously, making it particularly suitable for CPRD. However, acupuncture’s evidence base is less robust than CBT or SSRIs due to methodological limitations and fewer long-term studies.
Synergistic Approaches with CAM Nutraceuticals
Acupuncture’s efficacy for depression, particularly CPRD, can be enhanced through synergistic integration with standard treatments and CAM nutraceuticals:
- With Antidepressants: Combining acupuncture (especially EA or MA) with SSRIs/SNRIs enhances depression and pain outcomes in CPRD, as seen in studies where acupuncture plus antidepressants outperformed antidepressants alone. This synergy likely stems from acupuncture’s modulation of serotonin and noradrenaline pathways, complementing pharmacological effects.
- With Psychotherapy: Acupuncture integrates well with CBT or ACT, particularly in chronic pain settings, by reducing physical symptoms that exacerbate depression, thus improving engagement in therapy. The NADA protocol, used in addiction settings, suggests potential for similar integration in depression treatment programs.
- CAM Nutraceuticals:
- Magnesium: Citrate or bisglycinate (400–600 mg/day) modulates NMDA receptors, reducing excitotoxicity and depressive symptoms. Magnesium threonate (1–2 g/day) may enhance CNS penetration, supporting acupuncture’s neuroendocrine effects in CPRD.
- Zinc: Picolinate (30–50 mg/day) supports neurotransmitter balance and immune function, potentially reducing depression severity in chronic pain patients.
- Selenium: Selenomethionine (200 µg/day) provides antioxidant neuroprotection, complementing acupuncture’s anti-inflammatory effects.
- Omega-3 Fatty Acids: EPA/DHA (1–2 g/day) reduce inflammation and support mood stabilization, enhancing acupuncture’s effects on TNF and NF-kappa B pathways.
- Vitamin D: Cholecalciferol (2,000–4,000 IU/day) addresses deficiencies common in chronic pain and depression, supporting mood and pain outcomes.
- TCM Herbal Medicines: Hypericum perforatum (300–900 mg/day) may enhance acupuncture’s antidepressant effects but requires caution due to interactions with SSRIs. Future exploration of Corydalis yanhusuo could address both pain and depression in CPRD, aligning with Accurate Clinic’s integrative approach.
Discussion
Acupuncture demonstrates clinical benefits for depression, particularly CPRD, by reducing depression severity and pain intensity with a favorable safety profile. Electroacupuncture combined with antidepressants is the most effective, followed by manual acupuncture plus antidepressants and manual acupuncture alone. For CPRD, acupuncture is comparable to antidepressants with fewer adverse events and is more effective when combined with pharmacotherapy. Common acupoints (e.g., GV20, EX-HN3, PC6, ST36) modulate shared neural circuits (e.g., hippocampus, thalamus) and neurotransmitters (e.g., serotonin, noradrenaline), addressing both pain and depression.
Compared to standard treatments, acupuncture offers a non-pharmacological alternative with fewer side effects, making it suitable for patients intolerant to antidepressants or with limited access to psychotherapy. Its ability to address both pain and depression simultaneously is a key advantage in CPRD. Synergistic approaches with antidepressants, psychotherapy, and nutraceuticals (e.g., magnesium, zinc) enhance outcomes, aligning with Accurate Clinic’s integrative model. Future research should focus on high-quality, multicenter RCTs with standardized protocols, long-term follow-up, and comparative effectiveness studies to define acupuncture’s role in depression treatment algorithms.
Conclusion
Acupuncture, particularly EA and MA, is a safe and effective treatment for depression, with specific benefits for CPRD when used alone or combined with antidepressants. It reduces depression severity and pain intensity, offering a non-pharmacological option with minimal adverse events (e.g., mild headaches, dizziness). While comparable to antidepressants for CPRD and synergistic with pharmacotherapy and psychotherapy, acupuncture’s evidence base is constrained by low-quality studies, heterogeneity, and regional bias. Integration with CAM nutraceuticals (e.g., magnesium citrate, zinc picolinate) enhances its efficacy, supporting its role in integrative pain management. High-quality RCTs are needed to standardize protocols, assess long-term outcomes, and confirm applicability in diverse populations.
Relevance to Accurate Clinic: Acupuncture aligns with your integrative pain management program, particularly for CPRD patients. Its modulation of NMDA receptors and serotonin pathways synergizes with nutraceuticals like magnesium citrate (400–600 mg/day) and zinc picolinate (30–50 mg/day). Future incorporation of TCM herbs (e.g., Corydalis yanhusuo) could further enhance pain and depression outcomes, supporting holistic care for opioid-dependent or chronic pain patients.
References
- Interventions for Depressive Symptoms in People Living with Chronic Pain- A Systematic Review of Meta-Analyses – 2022
- Acupuncture for Chronic Pain-Related Depression- A Systematic Review and Meta-Analysis – 2021
- Efficacy and safety of acupuncture for depression- A systematic review and meta‐analysis – 2022
- Acupuncture for Depression- A Systematic Review and Meta-Analysis – 2019
- Armour M, Smith CA, Wang LQ, et al. Acupuncture for depression: a systematic review and meta-analysis. J Clin Med. 2019;8(8):1140. doi:10.3390/jcm8081140
- Cheng DK, Lai KSP, Pico-Espinosa OJ, et al. Interventions for depressive symptoms in people living with chronic pain: a systematic review of meta-analyses. Pain Med. 2022;23(5):934-954. doi:10.1093/pm/pnab248
- You J, Li H, Xie D, Chen R, Chen M. Acupuncture for chronic pain-related depression: a systematic review and meta-analysis. Pain Res Manag. 2021;2021:6617075. doi:10.1155/2021/6617075
- Chen B, Wang CC, Lee KH, Xia JC, Luo Z. Efficacy and safety of acupuncture for depression: a systematic review and meta-analysis. Res Nurs Health. 2023;46(1):48-67. doi:10.1002/nur.22284
- Smith CA, Armour M, Lee MS, Wang LQ, Hay PJ. Acupuncture for depression. Cochrane Database Syst Rev. 2018;3(3):CD004046. doi:10.1002/14651858.CD004046.pub4
- Malhi GS, Mann JJ. Depression. Lancet. 2018;392(10161):2299-2312. doi:10.1016/S0140-6736(18)31948-2
- Bauer M, Pfennig A, Severus E, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part 1: update 2013 on the acute and continuation treatment of unipolar depressive disorders. World J Biol Psychiatry. 2013;14(5):334-385. doi:10.3109/15622975.2013.804195
- Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-1222. doi:10.1016/S0140-6736(20)30925-9
- Hansen AH, Kristoffersen AE. The use of CAM providers and psychiatric outpatient services in people with anxiety/depression: a cross-sectional survey. BMC Complement Altern Med. 2016;16:461. doi:10.1186/s12906-016-1446-9
- von Luckner A, Riederer F. Magnesium in migraine prophylaxis: a systematic review and meta-analysis. Pain Physician. 2022;25(3):E321-E328. doi:10.36076/ppj.2022.25.E321
- Goschorska M, Gutowska I, Baranowska-Bosiacka I, et al. Selenium in neuroprotection: implications for chronic pain and headache management. Nutrients. 2023;15(12):2764. doi:10.3390/nu15122764
- Pizzorno JE, Murray MT, Joiner-Bey H. The Clinician’s Handbook of Natural Medicine. 3rd ed. Churchill Livingstone; 2016.
- World Health Organization. Depression. Accessed July 20, 2025. https://www.who.int/news-room/fact-sheets/detail/depression
- Australian Bureau of Statistics. National Health Survey: First Results, 2017-18. Accessed July 20, 2025. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/2017-18
- Santomauro DF, Mantilla Herrera AM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700-1712. doi:10.1016/S0140-6736(21)02143-7
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
.
