Acupuncture:
Acupuncture as a Treatment for Opioid Use Disorder
Opioid use disorder (OUD) is a chronic, relapsing condition characterized by compulsive opioid use despite harmful consequences, contributing significantly to global morbidity and mortality. Standard treatments for OUD include opioid substitution therapy (OST) with medications like methadone and buprenorphine, medication-assisted treatment [MAT]), psychosocial interventions (e.g., cognitive-behavioral therapy [CBT], contingency management), and, less commonly, detoxification programs.
Unlike OST, acupuncture avoids pharmacological dependence, making it appealing for patients with comorbidities or individuals wary of MAT.
See:
- Traditional Chinese Medicine (TCM)
- TCM – Chinese Herbal Medicine (introduction)
- TCM – Acupuncture Introduction
See also:
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
Definitions and Terms Related to Pain
Acupuncture as a Treatment for Opioid Use Disorder (OUD)
Introduction
The United Nations Office on Drugs and Crime (2022) estimated that 300 million people used illicit drugs in 2021, with opioids accounting for 70% of the global disease burden from drug use disorders. In the United States, the 2020 National Survey on Drug Use and Health reported over 40 million individuals with substance use disorders (SUDs), with OUD disproportionately affecting youth and young adults. OUD is associated with increased risks of overdose, infectious diseases (e.g., HIV, hepatitis C), and socioeconomic burdens. Effective treatment remains a public health priority, yet conventional approaches face challenges in accessibility, efficacy, and side effects.
Standard treatments for OUD
Standard treatments for OUD include opioid substitution therapy (OST) with medications like methadone and buprenorphine, psychosocial interventions (e.g., cognitive-behavioral therapy [CBT], contingency management), and, less commonly, detoxification programs. OST, introduced in the 1960s, is the cornerstone of OUD treatment, supported by extensive evidence for reducing illicit opioid use and mortality However, OST carries risks of dependency, side effects (e.g., sedation, constipation), and limited availability, particularly for adolescents (only 25% of youth with OUD receive medication-assisted treatment [MAT]).
Psychosocial interventions, widely advocated since the 1980s, enhance treatment retention but are less effective as standalone therapies. Detoxification, while effective for acute withdrawal, has high relapse rates due to protracted opioid abstinence syndrome (POAS).
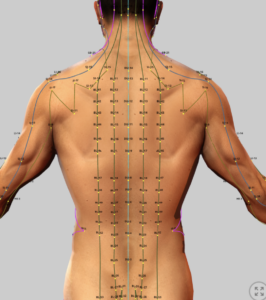
Acupuncture, a modality rooted in Traditional Chinese Medicine (TCM) for over 2,000 years, emerged in Western addiction medicine in the 1970s .Unlike OST, acupuncture avoids pharmacological dependence, making it appealing for patients with comorbidities or youth wary of MAT. Advocacy for acupuncture has grown, with the World Health Organization (WHO) recognizing its potential for addiction treatment in 1979 and the National Institutes of Health (NIH) endorsing it as an adjunct in 1997.
However, acupuncture’s evidence of effectiveness remains limited. This treatise evaluates acupuncture’s efficacy for OUD, focusing on withdrawal symptoms, psychological outcomes, and relapse prevention, compared to conventional modalities.
Efficacy of Acupuncture for OUD
A 2018 systematic review (Chen et al. (2018):) included 9 RCTs (1,063 participants) evaluating acupuncture for OUD. Note acronyms: manual acupuncture [MA], electroacupuncture [EA], auricular acupressure [AA], transcutaneous electrical acupoint stimulation [TEAS], opioid substitution therapy (OST), Random controlled trials (RCTs). Sham acupuncture is a placebo treatment used in acupuncture research to compare against actual acupuncture.It involves mimicking the appearance and sensation of acupuncture, but without actual needle insertion or stimulation of acupuncture points. This allows researchers to isolate the specific effects of acupuncture from the psychological or physiological effects of the placebo response.
Key findings include:
-
- Withdrawal Symptoms: EA and MA reduced withdrawal symptoms compared to no treatment/sham acupuncture. EA was more effective than sham EA for craving and depression . No significant benefit was found for AA or TEAS in reducing withdrawal symptoms.
- Psychological Symptoms: EA alleviated depression compared to no treatment/sham. TEAS improved insomnia and anxiety compared to no treatment/sham TEAS.
- Limitations: Small sample sizes, low study quality
- Conclusion: Acupuncture, particularly EA and TEAS, may reduce craving, depression, insomnia, and anxiety in OUD, but evidence is insufficient to confirm superiority over OST due to study limitations.
- Kitzman et al. (2023): This narrative review highlighted acupuncture’s role in addiction medicine, with a focus on auricular acupuncture (AA):
- Auricular Acupuncture (AA): Standardized auricular acupuncture (5 ear points: Shenmen, Sympathetic, Kidney, Liver, Lung) reduced cravings, anxiety, and depression in women with SUDs when added to psycho-educational programs. It also lowered methadone doses and improved treatment retention in residential settings.
- Neonatal Abstinence Syndrome (NAS): Acupuncture reduced morphine therapy duration and hospital stays in newborns with NAS. However, one study found no difference in hospital stay length with auricular acupressure.
- Mechanisms: Acupuncture modulates the limbic–paralimbic–neocortical system (fMRI evidence), reducing heroin cue-induced activation and enhancing endogenous opioid peptide release (dynorphins, enkephalins, endorphins).
- Limitations: Heterogeneous study designs, small sample sizes, and poor methodology (e.g., lack of randomization or controls) hindered definitive conclusions.
- Conclusion: Acupuncture, especially AA, is a safe adjunct for OUD, reducing withdrawal symptoms and supporting recovery, but requires integration with psychosocial interventions for optimal efficacy.
- A 2018 meta-analysis study (Ding et al) that focused on POAS, (28 RCTs, 2,463 participants) found acupuncture reduced withdrawal symptoms vs. OST and vs. no treatment), regardinf anxiety, depression, and sleep disturbances, but not cravings. Common acupoints (PC6, HT7, ST36, SP6) stimulated Substance P release, modulating opioid receptors and dopamine/serotonin pathways. High study bias with regional skew (mostly Chinese) limited generalizability.
Comparison with Other Modalities
- Opioid Substitution Therapy (OST):
- Advocacy and Timeframe: Since the 1960s, OST (methadone, buprenorphine) has been the gold standard, supported by international WHO guidelines for reducing illicit opioid use and mortality. Advocacy is strong due to robust RCTs and long-term outcomes.
- Limitations: Dependency risk, side effects (e.g., sedation, respiratory depression), and limited access for youth (only <25% of adolescents receive MAT). Relapse rates remain high post-tapering due to POAS,
- .
- Comparison: Acupuncture offers a non-pharmacological alternative, avoiding dependency but lacking OST’s robust evidence for long-term relapse prevention. Acupuncture may complement OST by reducing methadone doses.
- Psychosocial Interventions:
- Advocacy and Timeframe: CBT and contingency management, formalized in the 1980s, are widely endorsed as adjuncts to OST, improving retention but not standalone efficacy.
- Limitations: Resource-intensive, variable efficacy, and limited impact on physical withdrawal symptoms.
- Comparison: Acupuncture integrates well with psychosocial interventions, as seen in residential programs, enhancing compliance and reducing psychological symptoms .
- Detoxification:
- Advocacy and Timeframe: Used since the 1970s, detoxification is less advocated due to high relapse rates (80–90% within 1 year) driven by POAS.
- Comparison: Acupuncture outperforms no-treatment controls in POAS, offering a safer adjunct to manage protracted symptoms.
Mechanisms of Acupuncture in OUD
Acupuncture’s efficacy in OUD is linked to modulation of endogenous opioid systems and neural pathways:
- Endogenous Opioids: Acupuncture increases dynorphin, enkephalin, and endorphin release, suppressing withdrawal symptoms. Dynorphins inhibit heroin withdrawal, while endorphins reduce craving.
- Neurotransmitter Modulation: Stimulation of acupoints enhances dopamine and serotonin signaling in the nucleus accumbens and striatum, reducing psychological dependence.
- NMDA Receptor Modulation: Acupuncture inhibits NMDA receptor activity, reducing excitotoxicity and craving, aligning with mechanisms of magnesium threonate.
- fMRI Evidence: Acupuncture deactivates limbic–paralimbic–neocortical regions, reducing cue-induced craving.
Synergistic Nutraceutical Interventions
To enhance acupuncture’s effects in OUD, consider:
- Magnesium: Citrate or bisglycinate (400–600 mg/day) for its NMDA receptor antagonism, reducing craving and anxiety. Threonate (1–2 g/day) may enhance CNS penetration for refractory cases (von Luckner & Riederer, 2022).
- Zinc: Picolinate (30–50 mg/day) supports immune function and neurotransmitter balance, potentially reducing depression (Goschorska et al., 2023).
- Selenium: Selenomethionine (200 µg/day) for antioxidant effects, supporting neuroprotection in chronic OUD (Goschorska et al., 2023).
Safety and Adverse Effects
Acupuncture is generally safe, with minimal side effects (e.g., mild bruising, discomfort at needle sites). No serious adverse events were reported in the reviewed studies. Its non-pharmacological nature avoids drug–drug interactions, making it suitable for patients with comorbidities or individuals hesitant about MAT.
Discussion
Acupuncture, particularly EA, TEAS, and the NADA protocol, shows promise for OUD by reducing withdrawal symptoms, craving, anxiety, depression, and insomnia. EA and TEAS outperform sham controls in specific outcomes (e.g., craving, depression), while NADA enhances treatment retention and reduces methadone doses.
Compared to OST, acupuncture offers a safer, non-addictive adjunct but lacks the robust, long-term evidence of methadone or buprenorphine. It integrates well with psychosocial interventions, enhancing holistic care, particularly in residential settings. For POAS,, acupuncture outperforms no-treatment controls, suggesting utility in post-detoxification management.
Implications for Clinical Practice:
- Acupuncture (e.g., NADA protocol, EA at PC6/ST36, 3–5 sessions/week for 2–4 weeks) can be integrated into OUD treatment to reduce withdrawal symptoms and psychological distress, especially as an adjunct to OST or psychosocial therapy.
- Suitable for youth or patients with comorbidities due to its safety profile.
- Nutraceuticals like magnesium citrate (400–600 mg/day) and zinc picolinate (30–50 mg/day) may enhance outcomes by supporting NMDA modulation and neuroprotection.
- Potential future TCM herbs (e.g., Corydalis yanhusuo for analgesia)
Conclusion
Acupuncture, including MA, EA, TEAS, and the NADA protocol, is a promising adjunctive treatment for OUD, reducing withdrawal symptoms, craving, anxiety, depression, and insomnia, with a favorable safety profile. While EA and TEAS show specific benefits, and NADA enhances treatment retention, the evidence is constrained by low-quality studies, heterogeneity, and limited long-term data. Acupuncture complements OST and psychosocial interventions, offering a non-pharmacological option for youth, patients with comorbidities, or those in post-detoxification phases (e.g., POAS,). Integration with nutraceuticals like magnesium citrate and zinc picolinate may enhance outcomes.
References
- United Nations Office on Drugs and Crime. World Drug Report 2022. Accessed July 19, 2025. https://www.unodc.org/unodc/en/data-and-analysis/world-drug-report-2022.html
- Substance Abuse and Mental Health Services Administration. 2020 National Survey on Drug Use and Health. Accessed July 19, 2025. https://www.samhsa.gov/data/report/2020-nsduh-annual-national-report
- Chen Z, Wang Y, Wang R, Xie J, Ren Y. Efficacy of acupuncture for treating opioid use disorder in adults: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2018;2018:3724708. doi:10.1155/2018/3724708
- Kitzman JM, Bowman LC, Lin YC. Acupuncture in addiction medicine: its history, evidence, and possibilities. Med Acupunct. 2023;35(3):109-118. doi:10.1089/acu.2023.0021
- Ding L, Li C, Zhang P, et al. Acupuncture-related therapies for protracted opioid abstinence syndrome: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2018;2018:3724708. doi:10.1155/2018/3724708
- Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;2014(2):CD002207. doi:10.1002/14651858.CD002207.pub4
- Dutra L, Stathopoulou G, Basden SL, et al. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165(2):179-187. doi:10.1176/appi.ajp.2007.06111851
- Amato L, Davoli M, Minozzi S, et al. Methadone at tapered doses for the management of opioid withdrawal. Cochrane Database Syst Rev. 2013;2013(2):CD003409. doi:10.1002/14651858.CD003409.pub4
- Han JS, Zhang RL. Suppression of morphine abstinence syndrome by body electroacupuncture in rats. Acta Pharmacol Sin. 2004;25(5):533-538. PubMed:15132820
- Yang CH, Lee BH, Sohn SH. A possible mechanism underlying the therapeutic effects of acupuncture in the treatment of drug addiction. Evid Based Complement Alternat Med. 2008;5(3):257-263. doi:10.1093/ecam/nem081
- Sun Y, Xu Y, Yu J, et al. Neuroprotective effects of Achyranthes bidentata polypeptides against NMDA-induced excitotoxicity. Neurochem Int. 2012;61(8):1335-1342. doi:10.1016/j.neuint.2012.06.017
- von Luckner A, Riederer F. Magnesium in migraine prophylaxis: a systematic review and meta-analysis. Pain Physician. 2022;25(3):E321-E328. doi:10.36076/ppj.2022.25.E321
- Goschorska M, Gutowska I, Baranowska-Bosiacka I, et al. Selenium in neuroprotection: implications for chronic pain and headache management. Nutrients. 2023;15(12):2764. doi:10.3390/nu15122764
- World Health Organization. WHO Traditional Medicine Strategy: 2014–2023. Geneva: WHO; 2013. Accessed July 19, 2025. https://www.who.int/publications/i/item/9789241506090
- NIH Consensus Conference. Acupuncture. JAMA. 1998;280(17):1518-1524. doi:10.1001/jama.280.17.1518
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
.
