“Every nerve that can thrill with pleasure, can also agonize with pain.”
– Horace Mann
Prescription Medications:
Ketamine
Ketamine is a medication originally FDA approved as an anesthetic but has been found to be a potentially effective agent in the treatment of chronic pain, especially neuropathic pain, opoid tolerance and hyperalgesia, central sensitization and depression. It is increasingly being used both topically and orally as a new option for treating neuropathic pain.
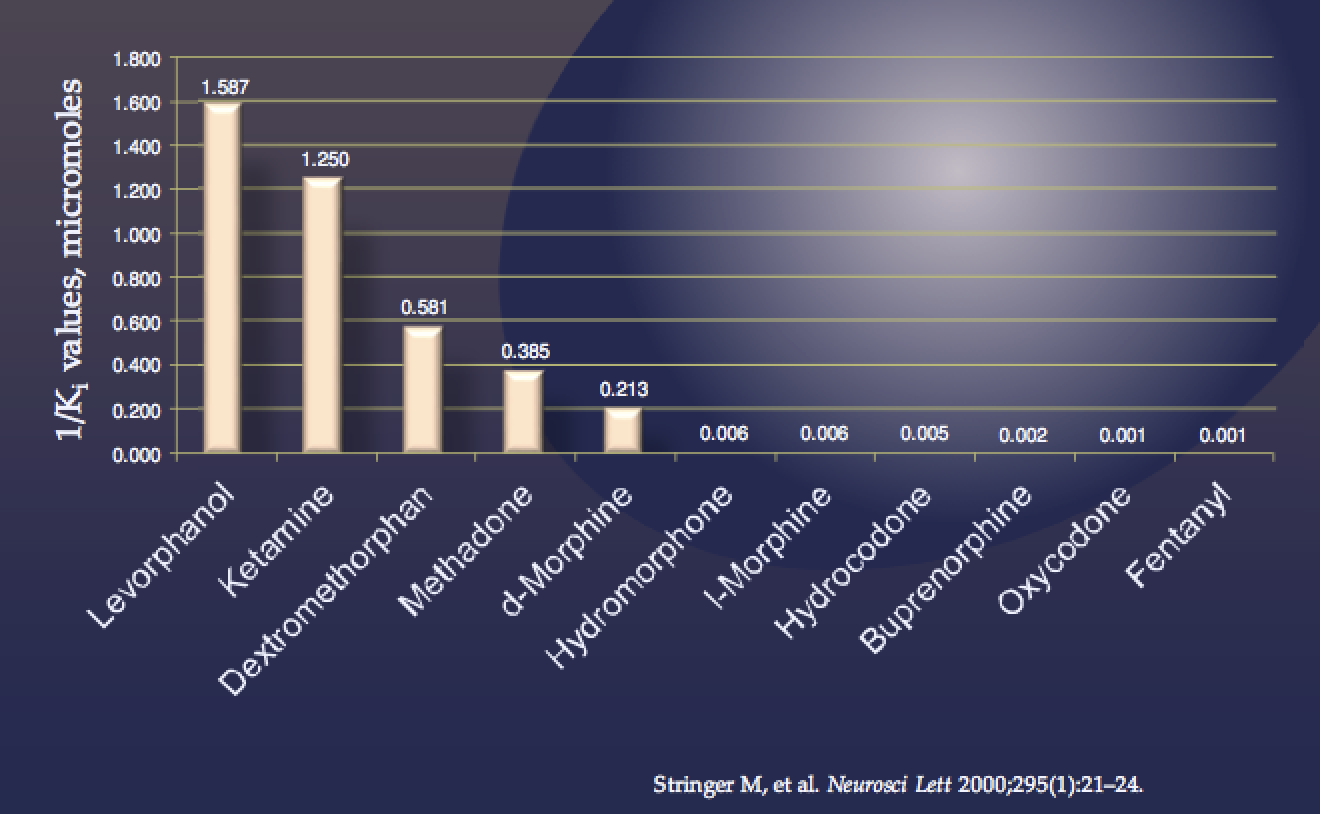
Ketamine is classified as an NMDA receptor antagonist, although its pharmacological profile is complex and it interact with numerous receptors including weak interactions with opioid and serotonin receptors.
It is recommended to first read the following sections to become familiarized with some of the terms and concepts related here:
- Education – Pain
- Neuropathic Pain
- Neurobiology of Pain
- Neurobiology of Opioids
- Central Sensitization
- Opioid Induced Hyperalgesia
Definitions and Terms Related to Pain
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
.
Ketamine
Ketamine is a phencyclidine derivative that was developed in the 1960s as an anaesthetic agent. The most important pharmacological properties of ketamine are due to it being a noncompetitive N-methyl-D-aspartate (NMDA) receptor antag- onist, and its analgesic action at subanaesthetic dose is believed to be primarily due to NMDA receptor antagonism in the brain and spinal cord
Ketamine in the Treatment of Pain
When used in chronic pain management, ketamine can be given via intravenous, subcutaneous, intramuscular, epidural, intra-articular, oral, topical, intra-nasal and sublingual routes. However, oral use is associated with much fewer side effects and topical use with minimal if any side effects. Intravenous use of ketamine appears to offer potential use for pain but it will not be addressed here.
Topical Ketamine
Depending on the source of pain, there may be an argument for the use of topical ketamine. Topical ketamine is not commercially available but can be a topical cream can be compounded at a cost of about $1/gm, representing a cost of use at about $3-4/day with use 3-4x/day. Topical ketamine is particularly effective in peripheral neuropathy, especially when associated with diabetes.
Oral Ketamine
Although the use of oral ketamine as an analgesic is now generally accepted, the amount of evidence remains weak. Little formal research has been performed on the effectiveness and safety of ketamine in chronic pain management, especially concerning long-term oral use. However, recent research shows that oral ketamine at low, slowly increasing doses may be effective in neuropathic pain. Ketamine is reported to reduce pain in patients with neuropathic pain of various origins, including postherpetic neuralgia, complex regional pain syndrome (CRPS), cancer pain, orofacial pain and phantom limb pain. Studies in fibromyalgia are lacking although it might be expected to be effective with fibromyalgia due to its mechanism of action blocking NMDA receptors.
Ketamine Intravenous Infusion Therapy
There has been growing evidence for the benefit of ketamine when given as an intravenous (IV) infusion. IV ketamine infusions have provided remarkable benefits for severe depression and chronic pain, particularly neuropathic pain. After only a few hours of IV ketamine infusions at doses usually beginning at 0.5-1mg/kg, patients with severe neuropathic pain syndromes including chronic regional pain syndrome (CRPS, previously termed Reflex Sympathetic Dystrophy (RSD), fibromyalgia and Ehler Danlos Syndrome experience dramatic relief of their pain that persists weeks to months.
The infusions are well tolerated and safe. Unfortunately, ketamine is not FDA-approved for these indications so these treatments are therefore not covered by insurance. Ketamine infusions offer very promising treatment for those with severe, unrelenting pain. Dr. Ehlenberger is investigating the possibility of offering them to his patients at Accurate Clinic.
Based on informtion based on KetamineClinicsDirectory.com (accessed 27.03.18):
Ketamine infusion for pain usually costs between $700 to $2000 per treatment due to the fact that more ketamine drug is used per infusion and the infusions last longer. Some ketamine doctors might offer a single ketamine infusion to treat pain, while most perform a series of anywhere from 2 to 8 infusions for pain. The majority of ketamine providers seem to request an upfront payment for a complete set of IV ketamine infusions. Depending on the cost per infusion, a patient can expect to pay anywhere from $1400 to over $12,000 for a full series of IV ketamine treatments for pain.
After the initial treatments, patients usually require maintenance IV ketamine therapy. Maintenance ketamine treatments usually cost between $400 to $800 per treatment. Maintenance ketamine is used to keep depression and/or pain symptoms under control. Usually, maintenance treatment is required once per month. Some providers may advise infusions twice a month, while others provide ketamine maintenance less frequently or on an as-needed basis.”
For more information, see the medical publications listed below.
Adverse Effects
One problem with the use of oral ketamine is the potential for side effects that can be frequent, although starting with low doses can be helpful in their avoidance. Studies may have drop-out rates as high as 50% due to side effects.
Ketamine is a derivative of phencyclidine, also known as PCP or angel dust, which is a drug that has been illicitly used for its mind-altering effects. Though rare, ketamine may also cause hallucinations and distorted perceptions of sounds. The most frequently observed side effects involve the central nervous system, such as sedation, dizziness, sensory illusions and blurred vision, with hallucinations, nightmares and dissociative feeling considered the most disturbing. Patients also mention gastrointestinal adverse effects, such as nausea, vomiting, loss of appetite and abdominal pain. Disturbing side effects usually disappear when dosage is reduced without the need for discontinuing treatment.
Reports have been published regarding a potentially serious adverse reaction to the use of ketamine, Ketmine Induced Cystitis (KIC). Most reports identify KIC in people who abuse ketamine as a recreational drug, it has been reported even in pediatric cases prescribed ketamine therapeutically. Studies estimate that 20%–30% of ketamine abusers develop lower urinary tract symptoms including pain and increased frequency of urination as well as lower abdominal pain. A relationship between symptom severity and frequency/ dosage of abuse has been established, and is usually determined by the chronicity of the abuse. KIC presents in a similar pattern as does Interstitial Cystitis but KIC often involves the kidneys as well as the bladder. Management of KIC includes immediate discontinuation of ketamine use.
Dosage
When starting ketamine orally, a single dose of 0.5 mg/kg (35mg for a 150 lb individual) ketamine is initiated to evaluate the effect on pain relief and determine the duration of its effect. Doses can be increased in steps of 0.25 mg/kg according to its effectiveness and side effects, respectively. Typical oral doses range between 45 to 1000mg/day with the obvious caveat that higher doses are likely to be associated with more likelihood of side effects. The duration of effect after a single dose (if there is any effect) ranges from a few hours to 24 hours or more but the average dosing frequency is 3–4 times daily. Because oral formulations of ketamine are not commercially available, the liquid injectable formulation is given as an oral solution, usually mixed with fruit juice due to its bitter taste.
The information on adverse effects after long-term use, or development of tolerance to oral ketamine, in chronic pain patients is limited. Ketamine has been used in some patients for more than 1 year without observed tolerance or adverse effects associated with long-term use.
Drug Interactions
Ketamine is metabolized in the liver by the CYP-450 enzymes (CYP3A4 & 5), making ketamine subject to being affected by other medications that may increase or decrease it’s metabolism by their impact on CYP3A4 & 5. It also suggests the possiblity that genetic variants in an individual’s CYP3A4 &5 enzyme profile may impact their response to ketamine. Ketamine’s major metabolite, norketamine, is also an active drug, though 5x weaker than ketamine. The elimination half-life is 2–3 hours for ketamine and approximately 4 hours for norketamine. Norketamine is thought to contribute to the analgesic effect and the duration of effect after taking ketamine orally.
Ketamine in the Treatment of Tolerance, Hyperalgesia and Central Sensitization
In the study of ketamine in chronic pain and its mechanisms of action primarily as an NMDA antagonist, it is evident that there is a great deal of overlap in the mechanisms by which ketamine reduces nerve pain and how it reduces tolerance, hyperalgesia and central sensitization. The experience of reduced pain is influenced by all of these variables so that the experience likely represents a reduction in tolerance, hyperaglesia and central sensitization as well. At this time it is not really possible to seperate individual effects.
See:
- Opioid Tolerance
- Opioid Withdrawal
- Opioid-Induced Hyperalgesia (OIH)
- Withdrawal-Induced Hyperalgesia (WIH)
Summary
Ketamine as an analgesic has been proven to be effective in some patients with severe pain who have failed to respond to routine pharmacotherapy. It is not a medication to be used routinely in chronic pain patients but should be considered for selected individuals as a potentially viable option.
Ketamine in the Treatment of Depression
There is growing research to support the benefit of ketamine in treating depression. Research has focused on intravenous use of ketamine which has resulted in surprising effectiveness in some people. After a single intravenous infusion, patients have experienced significant reduction in their depression symptoms for as long a one week. Ketamine appears to directly target core depressive symptoms such as sad mood, suicidality, helplessness and worthlessness, rather than inducing a nonspecific mood-elevating effect. The mechanism by which ketamine is effective in depression is not yet understood, although ketamine has been shown to interact with serotonin receptors and influence levels of serotonin, norepinephrine and dopamine.
Ketamine as a Drug of Abuse
It should not go without mentioning that ketamine is also a known drug of abuse. Known as “Special-K” and other nicknames, recreational users seek the “dissociative” effects of ketamine, including the hallucinations, depersonalization and feelings of being “high.” Recreational doses are typically higher than analgesic doses, often greater than 1000mg (1gm). These higher doses may be accompanied by cognitive impairment including disruption of memory which are considered reversable when use of ketamine is discontinued. No definitive dependence/withdrawal syndromes have been identified with chronic use of ketamine.
Ketamine – Mechanism of Action
Resources:
References:
Ketamine – Overviews
- Pharmacological aspects and potential new clinical applications of ketamine: reevaluation of an old drug. – PubMed – NCBI
- The role of ketamine in pain management. – PubMed – NCBI
- Ketamine: Current applications in anesthesia, pain, and critical care – 2014
- The role of ketamine in the treatment of chronic cancer pain – 2015
- Ketamine – 50 Years of Modulating the Mind – 2016
- Ketamine use in current clinical practice – 2016
- Ketamine for pain – 2017
- Ketamine for pain management – 2018
- Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Acute Pain Management – 2018
- Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Chronic Pain – 2018
- Ketamine and Ketamine Metabolite Pharmacology – Insights into Therapeutic Mechanisms – 2018
- Ketamine: A Review of Clinical Pharmacokinetics and Pharmacodynamics in Anesthesia and Pain Therapy. – PubMed – NCBI – 2018
Ketamine –Infusions
Ketamine – Oral
- Use of oral ketamine in chronic pain management – a review. – 2009
- Sublingual Ketamine in chronic pain: Service evaluation by examining over 200 patient years of data | Jaitly | Journal of Observational Pain Medicine – 2013
- Efficacy and safety of oral ketamine for the relief of intractable chronic pain: A retrospective 5-year study of 51 patients. – PubMed – NCBI – 2015
- (417) Oral ketamine for chronic pain: a 32-subject placebo-controlled trial in patients on chronic opioids – The Journal of Pain – 2016
- Promising Data With Ketamine in Chronic and Phantom Limb Pain – 2016
- [NMDA-receptor antagonist in pain therapy]. – PubMed – NCBI CYP2B6*6 allele and age substantially reduce steady-state ketamine clearance in chronic pain patients – impact on adverse effects – 2015
- Experience of the use of Ketamine to manage opioid withdrawal in an addicted woman – a case report – 2016
- Ketamine – 50 Years of Modulating the Mind – 2016
- New use for an old drug – oral ketamine for treatment-resistant depression – 2018
- Oral ketamine analgesia in chronic pain and problematic rise in blood pressure – 2014
- Oral ketamine for phantom limb pain: An option for challenging cases – 2015
- Oral Ketamine in Treatment-Resistant Depression – 2017
Ketamine – Topical
- Topical and Peripheral Ketamine as an Analgesic – 2014
- A Comprehensive Algorithm for Management of Neuropathic Pain – 2019
Ketamine – Chronic Regional Pain Syndrome (CRPS)
- Ketamine Infusion for CRPS – 2008
- Ketamine as Adjunctive Anesthesia in Refractory Complex Regional Pain Syndrome Patients – A Case Series – 2012
- A Systematic Review of Ketamine for Complex Regional Pain Syndrome – 2015
- Ketamine Infusions for Refractory Complex Regional Pain Syndrome – A Review – 2016
- The Role of Ketamine in Treatment of Complex Regional Pain Syndrome – A review of current evidence – 2016
Ketamine – Ehler Danlos Syndrome
Ketamine – Fibromyalgia
- Modulation of NMDA Receptor Activity in Fibromyalgia – 2017
- Ketamine reduces muscle pain, temporal summation, and referred pain in fibromyalgia patients. – PubMed – NCBI — 2000
Ketamine – Neuropathic Pain
- Promising Data With Ketamine in Chronic and Phantom Limb Pain – 2016
- Sublingual Ketamine in chronic pain: Service evaluation by examining over 200 patient years of data | Jaitly | Journal of Observational Pain Medicine – 2013
- Use of oral ketamine in chronic pain management – a review. – 2009
- Ketamine infusion as Adjuvant Analgesic to Opioids – 2004
- Trends in Opioid Analgesic – 2015
- The role of ketamine in pain management. – PubMed – NCBI
- Topical and Peripheral Ketamine as an Analgesic – 2014
- Ketamine – an old drug revitalized in pain medicine – 2017
- Effect of ketamine combined with magnesium sulfate in neuropathic pain patients (KETAPAIN) – study protocol for a randomized controlled trial – 2017
- Ketamine for pain management – 2018
- Ketamine for pain – 2017
- (417) Oral ketamine for chronic pain: a 32-subject placebo-controlled trial in patients on chronic opioids – The Journal of Pain – 2016
Ketamine – Post-Operative Pain
- Role of Ketamine in Acute Postoperative Pain Management – A Narrative Review – 2015
- Perioperative ketamine for acute postoperative pain. – PubMed – NCBI
- Butorphanol and Ketamine Combined in Infusion Solutions for Patient-Controlled Analgesia Administration – A Long-Term Stability Study – 2015
- Preventing chronic postoperative pain – 2016
- Poorly controlled postoperative pain: prevalence, consequences, and prevention – 2017
- Chronic postoperative pain: recent findings in understanding and management – 2017
- Perioperative intravenous ketamine for acute postoperative pain in adults. – PubMed – NCBI – 2018
Ketamine – Depression
- Ketamine for Treatment-Resistant Unipolar Depression – 2012
- Ketamine and other N-methyl-D-aspartate receptor antagonists in the treatment of depression – 2015
- New use for an old drug – oral ketamine for treatment-resistant depression – 2018
Ketamine – Opioid Withdrawal
Ketamine – Opioid Tolerance
Ketamine – Opioid-Induced Hyperalgesia
- The role of ketamine in preventing fentanyl-induced hyperalgesia and subsequent acute morphine tolerance. – PubMed – NCBI
- The median effective dose of ketamine and gabapentin in opioid-induced hyperalgesia in rats: an isobolographic analysis of their interaction. – PubMed – NCBI
- Promising Data With Ketamine in Chronic and Phantom Limb Pain – 2016
- Sublingual Ketamine in chronic pain : Service evaluation by examining over 200 patient years of data | Jaitly | Journal of Observational Pain Medicine – 2013
- Use of oral ketamine in chronic pain management – a review. – 2009
- Ketamine for Treatment-Resistant Unipolar Depression – 2012
Ketamine, Complications: Ketamine Induced Cystitis
- Interstitial cystitis symptoms associated with ketamine abuse – The first Japanese case – 2011
- What Is Ketamine Cystitis
- Ketamine-induced vesicopathy: a literature review. – PubMed – NCBIThe clinical presentation and diagnosis of ketamine-associated urinary tract dysfunction in Singapore – 2015
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.