“Vitality shows in not only the ability to persist but the ability to start over.”
– Scott Fitzgerald
Low Back Pain (LBP) – Overview
Low back pain (LBP) is highly prevalent: about 80-90% of the population gets low back pain at some point in time and about 25% report having back pain in the past week. According to the Centers for Disease Control and Prevention (CDC), the prevalence of low back pain in adults 18 years of age and older is 28.4% and may range as high as 32.1% in adults ≥ 75 years (CDC, 2012).
There are entire books written about low back pain. Because it is such an exhaustive subject, the goal of this section of the website is to provide a basic understanding of the most common causes, how to distinguish between different causes, the role of diagnostic testing and an overview of treatment options.
The emphasis here is to provide an adequate understanding of back pain to help guide decision-making regarding treatment options for those with chronic LBP. Since many treatment options for pain are covered in detail on other pages of this site, the reader may be directed to links to these pages to avoid duplication.
See Also:
- Low Back Pain (LBP) – Overview
- LBP – Arachnoiditis
- LBP – Superior Cluneal Nerve Entrapment
- LBP – Disc Pain
- LBP – Facet Pain
- LBP – Failed Back Surgery Syndrome
- LBP – Myofascial Pain
- LBP – Sacroiliac (SI) Joint Pain
- LBP – Sciatica
- LBP – Spinal Stenosis
Treatment Procedures:
- Epidural Injections
- Facet Joint Injections and Nerve Procedures
- Heat & Cold Therapy
- Inversion Therapy
- Massage Therapy
- Physical Therapy
- Trigger Point Therapy
LBP – Surgery:
.
Low Back Pain (LBP)
As an important preface to the discussion of low back pain, it should be pointed out that there may be no singular history that can be provided by the patient, no findings on physical examination and no imaging tests including x-rays, MRIs and CT scans, or procedures that can reliably and accurately define the cause of an individual’s back pain. While each of these provide clues, it is the careful assessment of all the variables that can impact pain to illuminate a source or sources that will successfully lead to an accurate diagnosis of the cause, and often causes, of back pain.
There are multiple arguments in favor of, or against, the diagnostic accuracy of controlled local anesthetic blocks, but controlled local anesthetic blocks continue to be the best available tool to identify intervertebral discs, facet, or sacroiliac joint(s) as the source of low back pain. Unfortunately, these procedures are invasive, expensive, painful and often difficult to interpret, and therefore they may not be suitable for routine clinical use as a primary diagnostic modality. This leaves clinical assessment as the only process in many cases.
It is also important to understand that a finding on an imaging study such as an MRI that may appear grossly abnormal may nevertheless not be a source of pain. Clinical correlation is essential to determine the importance of abnormalities on imaging studies. Too often patients and clinicians chase these “abnormal” findings with treatments and procedures that are destined to fail from the beginning. A thorough assessment of pain is usually required to direct a successful treatment plan.
Sources of Chronic Low Back Pain (LBP)
Chronic low back pain is usually multifactorial. The major anatomic sources include the lumbar intervertebral discs, the facet joints, the sacro-iliac (SI) joints, and the soft tissues: muscles, ligaments and fascia (fibrous tissue surrounding muscles. The intervertebral disc is estimated to be the most common source of chronic LBP, estimated by one authority to represent up to 42%, with the facet joints the next most common source accounting for up to 31% and the SI joint up to 18%. Other authorities consider the soft tissues to be the most common source of LBP as they accompany all the other conditions most of the time.
Age correlates with the source of chronic LBP. Specifically, lumbar intervertebral disc cases were found to be significantly younger (average age 43.7 years) than cases of facet joint pain cases (59.8 years ) and SI pain cases (62.3 years).
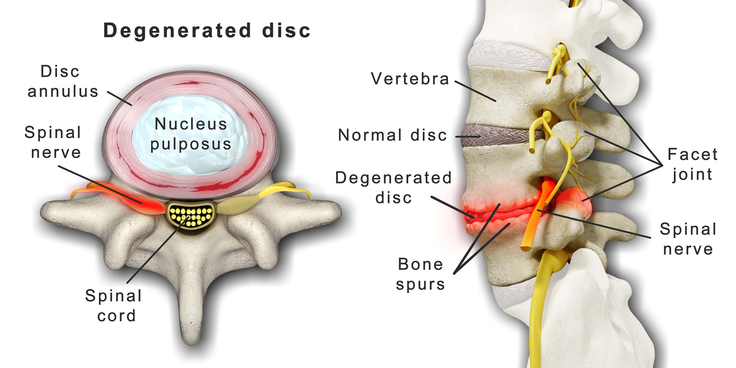
The spine consists of bony elements, the vertebrae, that are separated from one another by intervertebral discs that function as shock absorbers to prevent damage from bone-against-bone trauma related to movement of the spine. Along both sides of the spine are facet joints that provide for movement of the spine, including forward “flexion,” backward “extension,” leaning laterally and twisting. Connecting the vertebrae are ligaments, tendons and muscles, along with the fascia, the fibrous tissure surrounding all musculoskeletal components. There are nerve receptors in each of these components capable of sourcing pain, both locally and in referral patterns, causing a spread of pain to other areas.
To successfully identify pain sources, it is important to understand the character and patterns of pain that generally accompany each anatomic source of pain, including their referral patterns. This is not an exact science, as there are overlaps in pain characteristics and referral patterns as well as individual variations in anatomy and pain perceptions from one patient to the next. The treatment of pain therefore may require a trial and error approach until a successful outcome can be achieved.
Treatment of Chronic Low Back Pain (LBP)
Successful management of chronic LBP often requires an “integrative” approach, that is a treatment regimen that incorporates a multi-disciplinary collection of treatment options that include education, exercise, trigger point therapy, massage, spinal manipulation, acupuncture, diet and nutritional supplements, medications and mind-body disciplines such as yoga and tai chi. These topics are covered elsewhere on this website. However, for specifics regarding the diagnosis and management of the different anatomic sources of chronic LBP see:
- LBP – Disc Pain
- LBP – Facet Pain
- LBP – Myofascial Pain
- LBP – Sacro-Iliac (SI) Pain
- LBP – Spinal Stenosis
Procedures:
A Different Paradigm for the Assessment and Management of LBP
The correct identification of an anatomical source of pain is of critical importance to guide surgical or procedural techniques for the successful management of pain. However, in clinical practice the exact sources of pain is often elusive and poorly defined even with careful assessment. Patients often experience this when a physician makes a diagnosis followed by a surgical or interventional procedure that is unsuccessful in reducing pain. Then a second, or the same, physician follows with a different diagnosis as to the source of pain and a different recommended treatment. This does not necessarily reflect incompetence but rather the imprecision of the diagnostic process based on a great deal of overlapping manifestions of different anatomic sources of pain as well as individual variation.
Because it has been clearly demonstrated that accuracy of determining an anatomic source of LBP is often lacking, it can be argued that the management of LBP may require a “mechanistic” approach rather than an “anatomic” approach. In other words, as physicians understanding of the mechanisms of pain has grown, it is possible to identify the likely mechanism of a pain even if the specific anatomic source may be uncertain.
Three mechanism-based classifications of pain have been identified:
- Nociceptive
- Peripheral Neuropathic
- Central Sensitization
It has been established that pain states are characterized by a dominance of ‘nociceptive’, ‘peripheral neuropathic’ and ‘central’ mechanisms that may be distinguishable from one another clinically, based on the pattern recognition of clusters of symptoms and signs particular to each category. Consequently, management of pain can be guided by understanding the mechanism of the pain even when the source is not clearly identified. It has been established that certain medications, nutriceutical supplements and other treatment interventions have effectiveness based on these mechanisms of pain.
For example, true “sciatica” is nerve pain generated by irritation or compression of one or more lumbar nerve roots. It is likely experienced as “burning” or “electric” with a referral pattern that can be severe and follows a narow band of distribution. By identifying this pain as “peripheral neuropathic” pain and engaging medical management directed specifically at this nerve pain, successful pain control may be achieved without necessitating expensive imaging or procedures.
See: Neurobiology of Pain
Resources
www.SpineUniverse.com
References
LBP – Overviews
LBP – Failed Back Surgery Syndrome (FBSS)
LBP – Mechanisms of Pain
- The Discriminative Validity of “Nociceptive,” ” Peripheral Neuropathic,” and “Central Sensitization” as Mechanisms-based Classifications of Musculoskeletal Pain – 2011
- Clinical indicators of ‘nociceptive’, ‘peripheral neuropathic’ and ‘central’ mechanisms of musculoskeletal pain. A Delphi survey of expert clinicians – 2010
.
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.