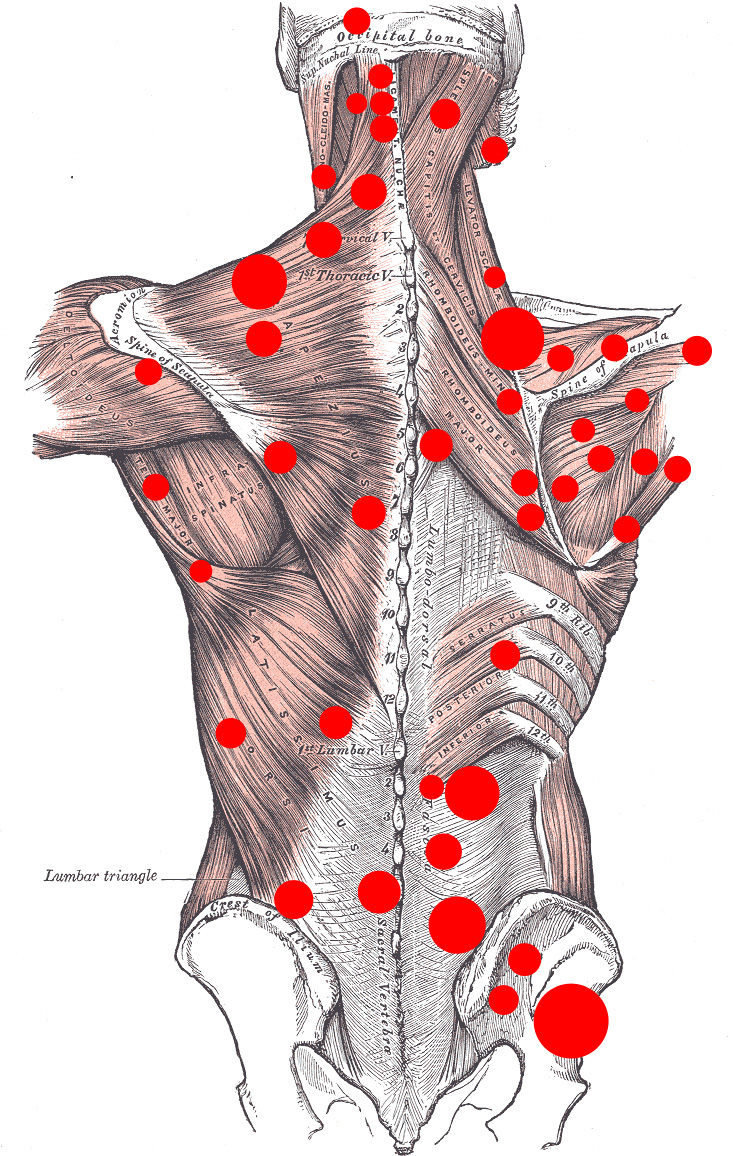
Sites of common trigger points (TrPs)
Trigger Point Therapy
for Myofascial Pain
See:
See Also:
Low Back Pain (LBP) – Overview
LBP – Sacroiliac (SI) Joint Pain
Treatment Procedures:
Facet Joint Injections and Nerve Procedures
Definitions and Terms Related to Pain
Key to Links:
Grey text – handout
Red text – another page on this website
Blue text – Journal publication
.
Myofascial Pain – Trigger Points (TrP)
What are Trigger Points?
Trigger points, also known as “myofascial trigger points (TrPs),” are hyper-irritable spots in the muscle and fascia (fibrous connective tissue) surrounding muscle (hence the term, “myofascial). They are associated with palpable nodules in taut bands of muscle fibers and are tender to touch. Trigger points are named so because when pressure is applied to a TrP or the the TrP is stretched, it triggers pain.
TrPs, when severe, can also becomes a source of continuous pain, even without active pressure or stretching. Additionally, a TrP can “refer” pain to another location, inches or more away from it’s source, in various patterns of referred pain. The patterns of referred pain have been mapped out by the physician who first identified and defined trigger points in 1942, Dr. Janet Travell who, incidentally, treated President John Kennedy for chronic myofascial pain. The exact nature of TrPs remains somewhat ill-defined, but they are best described as localized areas in muscle fibers that have become taut and inflamed, associated with release of cytokines (proteins) that are neurochemically active, stimulating localized inflammation and triggering local nerve receptors that cause pain.
Why are Trigger Points Significant?
As common sources of moderate to severe pain, TrPs are often overlooked and other conditions misdiagnosed as the source or cause of someone’s chronic musculoskeletal pain. Unfortunately, it is very common for people suffering from myofascial TrP pain to undergo invasive procedures such as epidural steroid injections, nerve blocks and ablations and even surgery (!) in what proves to be an unsuccessful means of treatment. Because it is not at all uncommon for patients with chronic neck or back pain to have multiple precipitating injuries and sources of pain including visible abnormalities on their MRIs, the key to managing their pain is to identify which potential source of pain is the actual culprit. Just because an abnormal finding exists on an MRI does not mean it is the source of pain, or at least the source of pain that is the most compromising. Not all referred pain, or “shooting pain,” is due to nerve compression.
What Causes Trigger Points?
There are a number of conditions that can lead to the creation of trigger points. A common scenario is one in which there is a localized injury such as a herniated lumbar disc that is associated with a great deal of pain with movement. As a consequence, the muscles in the lumbar area tighten up to limit motion around the injured, painful disc. Unfortunately, the continued pain related to movement results in prolonged and sustained contraction of muscle fibers that becomes pathologic for the muscle. It is thought that the sustained muscle fiber contraction leads to exhaustion of nutrients and compromise in the local blood supply, resulting in localized inflammation, changes in pH and release of the cytokines described above and other sensitizing substances.
Other mechanisms involved in the development of TrPs are direct muscle trauma or injury from overuse or over-stretching. Factors that make TrP pain worse include compression or stretching of the TrP, stress or anxiety, though these exacerbations are likely mediated by the increased muscle tone/contraction associated with stress. Cigarette smoking may be a contributing risk factor due to the constriction of blood vessels and impaired micro-circulation associated with nicotine and smoking.
The etiology of trigger point (TrP) formation in muscle and its mechanism of producing somatic symptoms is not fully understood. However, peripheral mechanisms, such as bio-chemical changes in neuromuscular junctions (where nerves interact with muscles to stimulate them) are thought to be a source of pathology. However, it believed that chronic musculoskeletal pain cases is characterized by alterations in central nervous system processes and autonomic nervous system activation that leads to prolonged stimulation and contraction of muscles leading to TrPs. Patients with TrPs may also have autonomic symptoms, such as sweating, goose bumps, changes in skin temperature, tearing and salivation. The connection between activity of the sympathetic nervous system and TrPs was confirmed in a recent 2016 study demonstrating the benefit of therapeutic dry needling of Trps ( see below).
Diagnosing Trigger Points
Trigger points are characterized by tender, palpable nodules or taut bands in muscle that when stimulated may elicit a twitch response which is a small, brief, localized muscle fiber contraction. Palpation of the trigger point reproduces the patient’s complaint of pain and may radiate pain to different areas in a distribution typical of the specific muscle harboring the trigger point. A twitch response can be felt in the muscle by running your finger perpendicular to the muscle’s directionThe identification of TrPs can be somewhat subjective and there can be some inconsistency in the interpretation of the physical exam.
There are no practical diagnostic laboratory tests or imaging studies available to establish or confirm the diagnosis of a TrP. The use of magnetic resonance elastography (MRE) imaging of the taut band of a TrP appears to identify TrPs but this technique remains limited to research. An MRE is a non-invasive medical imaging technique that measures the stiffness of soft tissues by using MRI technology.
Treating Trigger Points
The treatment of TrPs typically requires physical intervention in the form of either vigorous focal massage or instrumentation, either via “dry needling” with acupuncture needles or via the localized injection of small amounts of saline, an anesthetic such as lidocaine, botox or cortisone. For many clinicians, dry needling is the preferred method as it has been shown to be equally effective to the other techniques and is potentially less likely to lead to the local complications of using cortisone. It remains controversial as to which technique is superior.
Botox offers a promising option but research is limited at this time. “Dry needling” involves stimulation of the Trp for a few seconds without any injected material. While the process may sound intimidating and painful, in fact is the use of the very fine acupuncture needles is usually considered to be quite tolerable and significantly less painful than receiving a tatoo.
Securing Successful Treatment of TrP Therapy
A key element in the successful outcome of dry needling or TrP injections is the follow-through treatment. Because the instrumention causes a flare-up of the localized chemo-sensitive environment of the TrP, not unlike stirring up a hornet’s nest, it is important to follow-up within hours after instrumentation with hot water soaks, preferably with epsom salts (Magnesium salts). The heat stimulates dilation of blood vessels to carry in healing nutrients and lymphatic vessels to carry away the cytokines and other inflammatory proteins released by the instrumentation. It is important to be well hydrated during and after TrP treatment in order to support good blood and lymphatic flow. Continued hot epsom baths are advised twice a day for a full week after instrumentation.
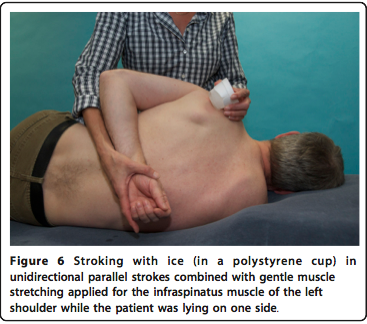
However, the passive reliance on hot soaks in not likely to be sufficient to secure an optimal outcome of TrP treatment. It is very important to stretch the affected muscle soon after instrumentation through the use of specific stretching exercises to maintain normal length of the muscle that has been in chronic, sustained contraction in order to prevent the TrP from reforming. The stretching exercises should be directed by the treating clinician and should start within hours of the instrumentation and repeated with 5 minute repetitions multiple times a day. When the muscle stretching is painful, it can be helpful to stroke the muscle with ice while stretching it to reduce pain sensation. This can be accomplished by freezing water in a styrofoam cup and using the frozen cup of water to stroke the muscle, peeling the cup lower as the ice melts.
For best results, it is recommended to also follow-up instrumentation with vigorous massage, preferably by a massage therapist experienced with TrP therapy. The massage should begin within 24 hours of instrumentation and be repeated daily (ideally) or as often as practical and affordable. The depth and intensity of the massage needs to be tailored to the needs of the patient as tolerated.
It is very common to hear of patients failing to achieve or maintain a favorable outcome from TrP therapy but in most cases, this failure is a result of poor follow-through. TrPs may take weeks, months or even years to evolve and persist – it is not likely to simply go away as a result of a momentary dry needling or injection.
Muscle Relaxers in the Treatment of Myofascial Pain
Tizanidine (Zanaflex) has been shown to be helpful in the management of myofascial pain, especially in the head, neck and shoulders.
See: Myofascial Pain
Example – Shoulder Pain
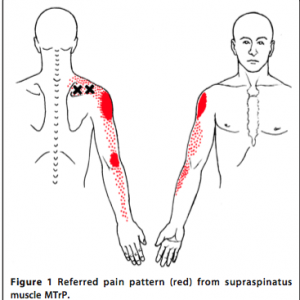
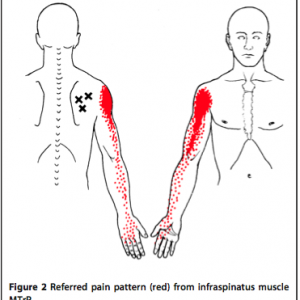
Shoulder pain is a common complaint in which TrP pain referral is mistakenly diagnosed as shoulder bursitis or arthritis or even a radicular pain referred from a compressed nerve root in the neck. The following diagrams from Travell (see below) illustrate the common distribution of pain (in red) from TrPs (black “X”).
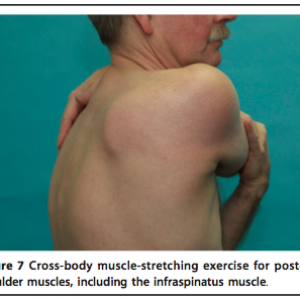
Example of stretching exercise for shoulder pain referred from a trigger point in the infraspinatous muscle, illustrated above:
References:
Myofascial Pain and TrP – Overviews
- Myofascial Pain and Dysfunction: The Trigger Point Manual (2 vol. set, 2nd Ed.). Travell, Janet; Simons David; Simons Lois (1999). USA: Lippincott Williams & Williams.
- Treatment of myofascial pain syndrome with lidocaine injection and physical therapy, alone or in combination – 2016
- Identification and quantification of myofascial taut bands with magnetic resonance elastography. – PubMed – NCBI
- New views of myofascial trigger points: etiology and diagnosis. – PubMed – NCBI
- Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. – PubMed – NCBI
- Botulinum toxin for myofascial pain syndromes in adults. – PubMed – NCBI
- Needling therapy for myofascial pain – recommended technique with multiple rapid needle insertion – 2014
- Evaluation of the Sympathetic Skin Response to the Dry Needling Treatment in Female Myofascial Pain Syndrome Patients – 2016
- Alpha-2 Adrenergic Receptor Agonists – A Review of Current Clinical Applications – 2015
- Relating Chronic Pelvic Pain and Endometriosis to Signs of Sensitization and Myofascial Pain and Dysfunction – 2017
- Effectiveness of ultrasound therapy for myofascial pain syndrome – a systematic review and meta-analysis – 2017
- Efficacy of Deep Dry Needling on Latent Myofascial Trigger Points in Older Adults With Nonspecific Shoulder Pain – A Randomized, Controlled Clinical Trial Pilot Study – 2017
- The Possible Role of Meditation in Myofascial Pain Syndrome: A New Hypothesis – 2017
- Myofascial Pain Syndrome – A Treatment Review – 2013
- Tizanidine is effective in the treatment of myofascial pain syndrome. – 2002
Myofascial Pain and TrP – Mechanisms of Pain
- The Discriminative Validity of “Nociceptive,” ” Peripheral Neuropathic,” and “Central Sensitization” as Mechanisms-based Classifications of Musculoskeletal Pain – 2011
- Clinical indicators of ‘nociceptive’, ‘peripheral neuropathic’ and ‘central’ mechanisms of musculoskeletal pain. A Delphi survey of expert clinicians – 2010
- Myofascial Trigger Points – Peripheral or Central Phenomenon? -2014
- Effectiveness of ultrasound therapy for myofascial pain syndrome – a systematic review and meta-analysis – 2017
- Randomized controlled study of the antinociceptive effect of ultrasound on trigger point sensitivity novel applications in myofascial therapy? – PubMed – 2007
Myofascial Pain and TrP – Shoulder Pain
- Treatment-of-myofascial-trigger-points-in-patients-with-chronic-shoulder-pain-a-randomized-controlled-trial-2011
- High-prevalence-of-shoulder-girdle-muscles-with-myofascial-trigger-points-in-patients-with-shoulder-pain-2011
- chronic-shoulder-pain-of-myofascial-origin-a-randomized-clinical-trial-using-ischemic-compression-therapy-pubmed-ncbi
- Effectiveness of Ultrasound Therapy on Myofascial Pain Syndrome of the Upper Trapezius – Randomized, Single-Blind, Placebo-Controlled Study – 2018
- Effect of Therapeutic Sequence of Hot Pack and Ultrasound on Physiological Response Over Trigger Point of Upper Trapezius – 2015
- Myofascial trigger points in shoulder pain – Prevalence, diagnosis and treatment. – 2011
Myofascial Pain and TrP – Tizanidine (Zanaflex)
- Myofascial Pain Syndrome – A Treatment Review – 2013
- Tizanidine is effective in the treatment of myofascial pain syndrome. – 2002
- Alpha-2 Adrenergic Receptor Agonists – A Review of Current Clinical Applications – 2015
.
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.