“Our soul desires to be understanding, our ego is only concerned with being understood. When you are being understanding you are connected to your soul.”
– Michaiel Bovenes
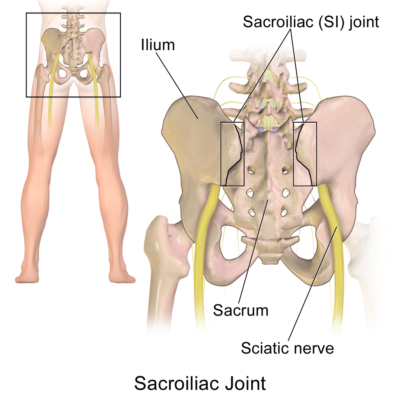
Low Back Pain: SacroIliac (SI) Joints
The sacroiliac (SI) joints are quite common sources of low back pain (LBP), yet often overlooked. SI joint pain is usually unilateral and is a cause of the pain in up to 10% to 30% of patients with chronic LBP below the 5th lumbar vertebra.
See Also:
- Low Back Pain (LBP) – Overview
- LBP – Arachnoiditis
- LBP – Superior Cluneal Nerve Entrapment
- LBP – Disc Pain
- LBP – Facet Pain
- LBP – Failed Back Surgery Syndrome
- LBP – Myofascial Pain
- LBP – Sacroiliac (SI) Joint Pain
- LBP – Sciatica
- LBP – Spinal Stenosis
Treatment Procedures:
- Epidural Injections
- Facet Joint Injections and Nerve Procedures
- Heat & Cold Therapy
- Inversion Therapy
- Massage Therapy
- Physical Therapy
- Trigger Point Therapy
LBP – Surgery:
.
Sacroiliac (SI) Joint Pain
At the base of the spine is the sacrum, the bone that connects the spine to the pelvis. The sacroiliac joint (SIJ) is the joint connecting the spine to the pelvis with strong ligaments where it supports the weight of the upper body in the standing position. There are SIJs in both the right and left side of the lower back. The SIJ has many nerves and is often a source of low back pain and referred pain in the lower extremity. Low back pain originating from the SIJ can result from traumatic injury or surgery, degeneration (wear and tear), arthritis (sacroiliitis) or pregnancy. The SIJ is the most common cause of LBP in pregnancy. SIJ can also result from inflammatory conditions such as spondyloarthropathy (ankylosing spondylitis; rheumatoid spondylitis).
SIJ pain most often occurs in the buttocks and lower back, and may radiate down through the buttocks and the leg. Sacroiliac pain, similar to facet pain of the lumbar spine, becomes more common as people age, with the average age of 62 years at onset in the absence of trauma. There tends to be a trend for a higher likelihood of low back pain to come from the SI joints vs facets when there is no associated thigh pain, but the reverse is true when there is associated thigh pain. In other words, facetogenic pain is more likely to refer to the thigh than SI joint pain.
Predisposing factors for SIJ pain include true and apparent leg length discrepancy, older age, inflammatory arthritis, previous spine surgery and pregnancy. SI joint pain may develop as a result of trauma, particularly when there is a direct force against the SI joint (i.e. fall onto buttocks) or a shearing force as may occur when rear-ended in a motor vehicle accident.
The SI joint as a pain generator is sometimes associated with failed back surgery in patients who have undergone lumbar fusions for discogenic pain. The literature suggests this may represent a misdiagnosis that is more common than previously reported.
Other sources of risk for SI joint pain include inflammatory arthritis conditions such as ankylosing spondylitis (AS), a rare but debilitating condition associated with spine and SI stiffness and onset early in age. Crohns and Ulcerative Colitis can also be associated with inflammatory sacroiliitis and represent increased risk for SI pain.
Diagnosis of Sacroiliac Joint Pain
Unfortunately, no single history, physical exam, or radiological feature can definitively establish a diagnosis of sacroiliac joint pain. The successful diagnosis and treatment of sacroiliac joint pain is compromised by wide variability and a lack of definitive evidence in the scientific literature. A working diagnosis, nevertheless, can be established with a thorough evaluation that combines history, physical exam and imaging. While a definitive diagnosis can arguably be established with a diagnostic block of the SI joint with an anesthetic injection, this procedure is painful and expensive.
One source of pain in the area of the SIJ that may be misdiagnosed as SIJ pain is entrapment of the middle cluneal nerve. A similar pattern of tenderness may exist but treatment is clearly different.
See: LBP – Cluneal Nerve Entrapment
Signs and Symptoms of Sacroiliac Joint Pain
SI joint pain is usually unilateral and virtually all patients have pain distal to the posterior iliac crest and lateral to the midline spine. Pain from the SI joint tends to be located over the joint and patients will tend to point directly over the SI joint when asked to show where the pain is centered. It is not uncommon for SI joint pain to disrupt sleep.
SI joint pain is worsened with prolonged sitting so the patient may tend to avoid sitting on the affected side and may frequently shift side-to-side while seated for extended periods. SI joint pain is worsened during transition from sitting to standing and the pain may also increase with single leg weight bearing. There may be instability of the leg on the affected side so that the leg may “give out” sometimes.
Referral Patterns of SI Pain
SI joint pain radiates distally. and is rarely, if ever, experienced above the L5 level. Therefore, unlike facet pain, pain located exclusively below the 5th lumbar vertebrae increases the likelihood of the sacroiliac joint being the source. SI joint pain is frequently referred to the groin, thigh, calf, and occasionally even the foot—patterns that might otherwise suggest radiculopathy or even hip joint pathology.
Physical Examination
A discrepancy in leg length is sometimes found which may be a risk factor for SI joint pain. Most often there is tenderness directly over the SI joints. Individuals whose point of maximum discomfort falls within an area that extends 10 cm (4-5 inches) below and 3 cm lateral to the posterior superior iliac spine are more likely to have sacroiliac joint pain (view posterior superior iliac spine).
Although not specific, a diagnosis of SI joint pain is most likely when there is tenderness directly over the SI joints and positive findings on three provocative tests are also present. Provocative tests are specific maneuvers involving the SI joint that a clinician performs in order to reproduce the pain complaint. Although provocation maneuvers have been evaluated by multiple investigators, an evaluation of these studies suggests there is only limited evidence that they are helpful in determining the likelihood of sacroiliac joint pain in patients with pain located primarily below the 5th lumbar vertebrae.
Another author identified pain triggered by changing position from sitting to standing coupled with a lack of centralization on repeated physical exams to strongly correlate with positive findings with anesthetic blocks.
Imaging studies
Plain radiographs, MRIs, CT scans and bone scans are not definitive and appear to be of no significant value in chronic sacroiliac joint pain without inflammatory arthritis. However, if findings of inflammatory arthritis are confirmed, a potential source of pain is identified.
Diagnostic Procedures
The confirmation of the SI joint pain as the source of chronic LBP is most accurately determined by obtaining relief of the target pain after fluoroscopically guided local anesthetic SI joint injection, performed twice (i.e if one injection is determined to be positive, a second confirmation injection is performed).
Treatment of SI Joint Pain
Treatment for SIJ pain depends upon the signs and symptoms, as well as the underlying cause for the pain. Medications, such as NSAIDs, opioids, muscle relaxants or tumor necrosis factor (TNF) inhibitors, such as etanercept (Enbrel), adalimumab (Humira), or infliximab (Remicade), may be prescribed. Interventional procedures used to treat SIJ pain include corticosteroid injections to reduce inflammation and pain, radiofrequency denervation and electrical stimulation. However, there is limited evidence regarding any of these non-surgical treatments for long term effectiveness. If these measures fail to provide significant and lasting symptom relief, surgical options may be considered.including SI joint fusion.
Treatment Based on Mechanisms of SI Joint Pain
It is believed that the basis of SI joint pain stems from degenerative and inflammatory processes suggesting the dominant mechanism of pain to be nociceptive. This is also consistent with the common descriptions of SI joint pain to be dull and achy in character. For this reason, medical management of SI joint pain should likely focus primarily on medications directed at nociceptive pain including non-steroidal anti-inflammatory drugs (NSAIDs) and when required, opioids.
Due to a possible inflammatory role in SI joint pain, other therapeutic measures directed at osteoarthritis would also likely be helpful.
See: Osteoarthritis
There is some research that suggests a component of neuropathic pain in the pain of arthritis. If a patient appears to have symptoms suggestive of neuropathic pain including sharp, stabbing, burning or electric-like pain, a trial of neuromodulators should be considered.
See: Neuropathic Pain
Physical Therapy
The benefit of physical therapy has been well established for SI joint pain but must be individually assessed and directed. Therapy sessions with a physical therapist involving range-of-motion stretching and strengthening exercises may be used to maintain joint flexibility and strengthen the muscles.
See: Physical Therapy
Treatment Procedures
SI joint Injections (Intra-Articular Steroid (IAS) Injections)
The SI joints can be selectively injected with a mixture of a local anesthetic and an anti-inflammatory steroid (like cortisone) in the same manner commonly employed for painful, arthritic shoulders and knees. In order to confirm correct placement of the injectable medication into the SI joint space, fluoroscopic or computed tomography (CT) guidance is used. An injection into the soft tissue around the SIJ may be used if ligamentous or muscular attachments are suspected to be the source of pain. The goal of the therapeutic injection is to reduce inflammation and/or pain and provide long-term pain relief. The duration of relief after IA steroid injection varies greatly. Long-term relief is generally defined as 6 weeks or longer, but positive responders generally have a much longer duration of response; serial injections may be required in order to maintain therapeutic effectiveness. While some patients achieve long-lasting relief after one to three injections, others may require several injections each year.
While evidence supports that SIJ injection is an effective method of determining the source of pain, the evidence is considerably limited. There are few controlled or prospective clinical studies to support SIJ injection for therapeutic purposes. Despite the limited quality of the clinical studies supporting SIJ injection for the treatment of SIJ pain, the procedure is recommended by the American Society of Anesthesiologists (ASA) and the American Society of Regional Anesthesia and Pain Management (ASRAPM) Practice Guidelines.
Radiofrequency Neurotomy (RFN) of the SI Joint
For patients who’s pain does not respond to conservative treatments, SI joint RFN, a procedure where the nerves carrying pain signals from the SI joint are burned, has been shown to be useful in some people. Sacral lateral branch radiofrequency neurotomy is more effective than placebo treatment but the duration of effect is limited. Whereas 80% of patients achieved at least 50% relief of their pain at 1 month in one study, this proportion had dropped to 60% at 6 months and 10% at 12 months.
Surgical Fusion of the SI Joints
In a 2015 systemic review study evaluating effectiveness of surgery, open surgery or minimally-invasive surgery (MIS), it was found that “rates of excellent satisfaction, determined by pain reduction, function, and quality of life, ranged from 18% to 100% with a average of 54% in open surgical cases. For MIS patients, excellent outcome, judged by patients’ stated satisfaction with the surgery, ranged from 56% to 100% (average 84%). The re-operation rate after open surgery ranged from 0% to 65% (average 15%). Re-operation rate after MIS ranged from 0% to 17% (average 6%). Major complication rates ranged from 5% to 20%.”
Nevertheless, authors of the 2015 review concluded that “Surgical intervention for SIJ pain is beneficial in a subset of patients. However, with the difficulty in accurate diagnosis and evidence for the efficacy of SIJ fusion itself lacking, serious consideration of the cause of pain and alternative treatments should be given before performing the operation.”
In yet another review of MIS published also in 2015 concluded “Published studies of MIS SI joint fusion using a lateral transarticular approach confirm its minimally invasive characteristics with minimal blood loss and short operating room times, and show consistent, rapid, sustained and clinically important improvements in patient reported SI joint pain, disability and quality of life scores.”
References
LBP: SI Pain – Overviews
- Ignoring the sacroiliac joint in chronic low back pain is costly – 2016
- Sacroiliac joint pain: a comprehensive review of epidemiology, diag… – PubMed – NCBI – 2013
- Sacroiliitis- A Review on Anatomy, Diagnosis, and Treatment – 2023.pdf
- Sacroiliitis – StatPearls – 2023.pdf
LBP: SI Pain – Diagnostic Evaluations
- Evaluation of Sacroiliac Joint Interventions – 2009 A Systematic Appraisal of the Literature. – 2009
- A Prospective Study of Centralization of Lumbar and Referred Pain – A Predictor of Symptomatic Discs and Anular Competence – 1997
LBP: SI Pain – Mechanisms of Pain
- The Discriminative Validity of “Nociceptive,” ” Peripheral Neuropathic,” and “Central Sensitization” as Mechanisms-based Classifications of Musculoskeletal Pain – 2011
- Clinical indicators of ‘nociceptive’, ‘peripheral neuropathic’ and ‘central’ mechanisms of musculoskeletal pain. A Delphi survey of expert clinicians – 2010
LBP: SI Pain –Referral Patterns
LBP: SI Pain – Treatment
- Surgical and clinical efficacy of sacroiliac joint fusion – a systematic review of the literature. 2015 – PubMed – NCBI
- A systematic review of minimally invasive sacroiliac joint fusion utilizing a lateral transarticular technique – 2015
.
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.
