“Ambition is the path to success. Persistence is the vehicle you arrive in.”
– Bill Bradley
Prescription Medications:
Rotating from Other Opioids to Buprenorphine, for Pain
It is recommended to first read the following sections to become familiarized with some of the terms and concepts related here:
- Handout – Microdosing Rotation to Buprenorphine
- Opioid Induced Hyperalgesia (OIH)
- Buprenorphine for Pain
- Opioids
- Cold Pressor Test )CPT)
Also see:
- Buprenorphine Treatment – Emergency and Surgery Pain Management
- Buprenorphine in Pregnancy & Breast Feeding
- Naloxone (Opioid Blocker)
See also: Buprenorphine for Opioid Substance Use Disorder (SUD)
Definitions and Terms Related to Pain
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
.
Opioids – Buprenorphine for Pain
Buprenorphine for Pain – A Brief Overview
Buprenorphine is an opioid medication commonly used for treating pain and, because of it’s special characteristics, it is also offers significant potential advantages for pain management over other opioids. While buprenorphine is also commonly used for treating opiate addiction, many people have the mistaken belief that it is used only for addiction which is not the case at all.
Buprenorphine is effective for both neuropathic (burning and electric/tingling) pain and nociceptive (dull and aching) pain. Some of the strongest clinical evidence of buprenorphine’s effectiveness for pain is for chronic low back pain and peripheral neuropathies.
Buprenorphine also appears to have the advantage of being less likely to develop tolerance to it’s pain benefits compared to many other opioids. Because buprenorphine is different, even those patients with high tolerance that require high doses of opioids such as oxycodone to control their pain usually respond well to buprenorphine for pain control.
Buprenorphine has an extensive set of favorable unique properties that include:
(1) High potency: more potent than morphine, hydrocodone and oxycodone;
(2) Long half-life and slow dissociation from the mu-receptor, providing advantages over other opioids;
(3) Safety advantages over other opioids, including a “ceiling response” to respiratory depressive effects, a benefit that makes buprenorphine potentially the safest opioid with respect to unintentional overdose;
(4) Buprenorphine binds tightly to the mu-receptor (the opioid receptor where all commonly prescribed opioids act to reduce pain);
(5) Buprenorpine offers greater analgesic benefits than some of the other commonly prescribed opioids for certain types of pain including neuropathic pain, deep bone pain and certain cancer-related pains. This may, at least in part, be due to agonist action at the ORL-1 receptor;
(6) Buprenorphine reduces depression, probably by blocking the kappa-receptor (another opioid receptor), a property that makes buprenorphine also effective as a mood elevator;
(7) Buprenorphine displays a limited degree of analgesic tolerance that likely stabilizes over time and is often effective for patients who have developed analgesic tolerance to other opioids. This reduced tolerance is thought to, at least in part, be due to it’s agonist action at the ORL-1 receptor. This same agonist action at the ORL-1 reeceptor may also be responsible for buprenorphine’s reduced reward effects and likelihood for abuse;
(8) Buprenorphine does not reduce testosterone levels in men or women as can occur with other opioids;
(9) Buprenorphine does not appear to reduce the immune response, a finding of still undetermined significance that appears to occur with some other opioids;
(10) Buprenorphine can be used more safely with those with pancreatitis;
(11) Buprenorphine has less affect on the sphincter of Oddi than many other opioids;
(12) Withdrawal symptoms with buprenorphine are less severe than many other opioids;
(13) Buprenorphine is one of the safest opioids for use in renal failure and dialysis and doses do not have to be altered in mild to moderate liver impairment (Child–Pugh class A and B);
(14) Buprenorphine is better tolerated in the elderly than many other opioids;
(15) Buprenorphine may be given with other opioids and may improve safety in their combination by reducing the reward and craving effects of the other opioids
(16) Buprenorphine appears to reduce the process of central sensitization. Central sensitization often develops with chronic pain, causing magnification of pain perception and reduced tolerance of unpleasant sensory stimulation. When taken concurrently with other traditional opioids, buprenorphine may provide a protective effect against the development of central sensitization.
(17) Unlike many other opioids, buprenorphine has not been associated with triggering serotonin syndrome, a condition resulting from excessive levels of serotonin in the nervous system characterized by a flu-like syndrome that is usually mild but can be fatal in severe cases.
For more in-depth information regarding these properties of buprenorphine, please see: Buprenorphine for Pain
Buprenorphine with other opioids
Buprenorphine has a special characteristic compared with other opioids: it has a very strong binding affinity to the receptors in the nervous system that provide pain control. This means that it may displace other opioids in a patient’s system and this displacement may trigger withdrawal symptoms dependent on a person’s level of physical dependence to their opioids. For this reason it is important that you discuss with your physician how to make the transition from another opioid to buprenorphine before doing so. This strong binding characteristic of buprenorphine also means that when a patient is taking buprenorphine for pain, the addition of other opioids may be less likely to provide significant additional pain benefit. Again, there are a number of variables that come into play here including the dose of buprenorpine one is taking and which additional opioid. However, at lower doses such as those associated with Belbuca (a buccal strip) and Butrans patches, it has been clearly demonstrated that the addition of other commonly prescribed opioids will add analgesic benefit without impairment by the buprenorphine.
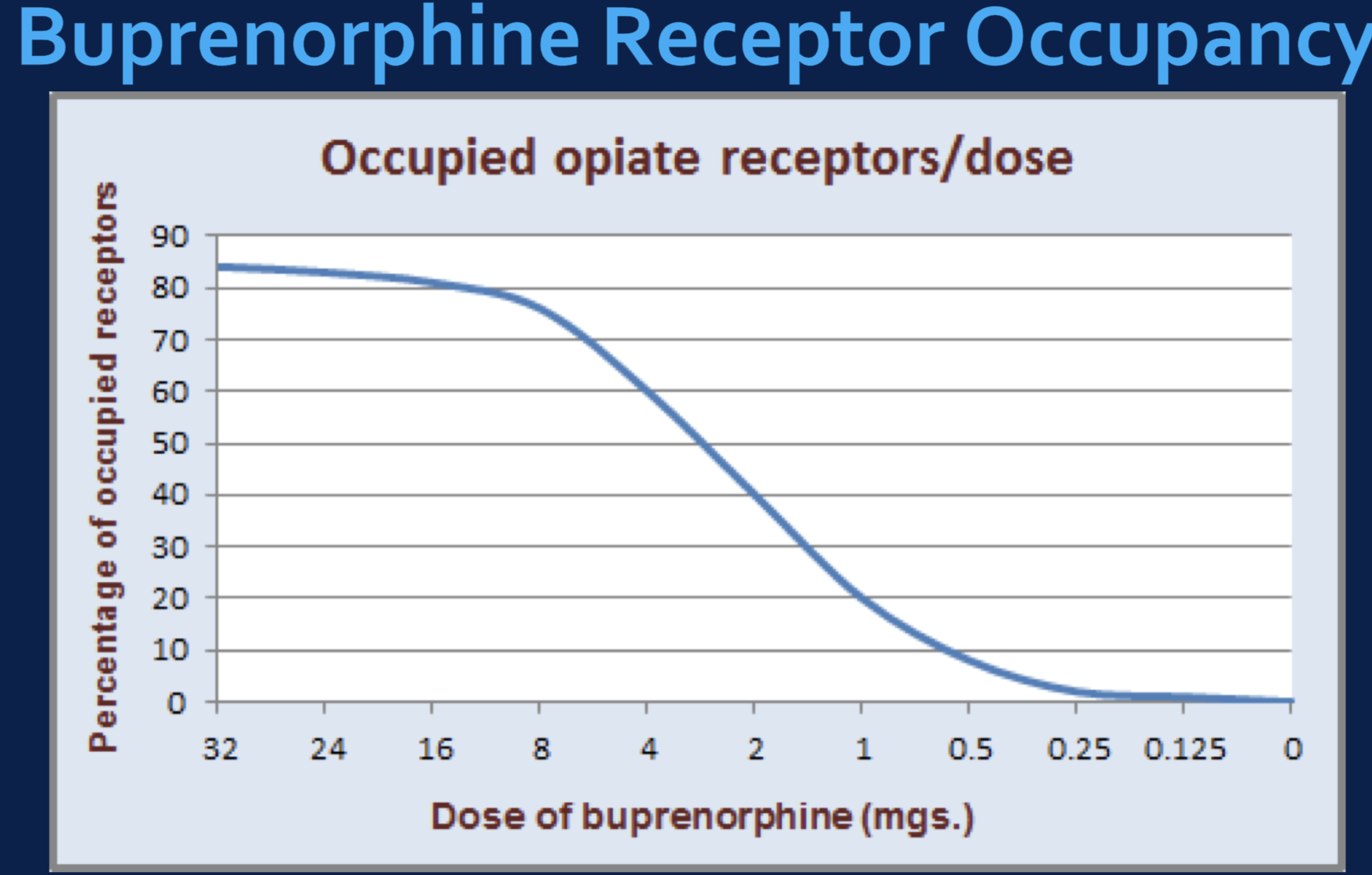
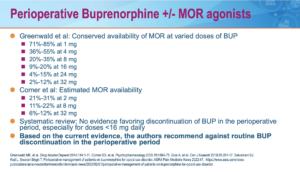
The primary factor determining the potential analgesic benefit of a second opioid added to buprenorphine is the relative degree to which buprenorphine occupies an individual’s mu-opioid receptors. For example, if buprenorphine which binds tightly to the mu-opioid receptors occupies 80-90% of these receptors, the addition of a second opioid is going to have a very limited effect unless that opioid has an even greater binding affinity to the receptors than buprenorphine. This is why high dose buprenorphine (16mg/day) blocks the effects of most opioids because at this dose 80% or more receptors are bound.
In contrast, with dosing with Belbuca even at 900 mcg twice a day, less than 40% of the mu-opioid receptors are occupied, leaving greater than 60% of the receptors available to a second opioid, even one with a weaker binding affinity. See below:
This does not mean, however, that one cannot overdose by adding other opioids while taking buprenorphine. In fact, one can. So it is advised to not take any other opioids while taking buprenorphine for pain unless guided by a physician with special knowledge regarding buprenorphine management. Such circumstances may arise with emergency conditions that are accompanied by severe pain that is not adequately controlled with buprenorphine. If this happens, one must notify the emergency physician that they are taking buprenorphine to facilitate appropriate choices to effectively manage the pain.
See also: Naloxone
Converting to Buprenorphine from other opioids
As noted above, there are many advantages to the use of buprenorphine for pain. While some physicians prefer buprenorphine as the initial choice of opioid for treating chronic pain, in most cases, patients are started on traditional, full agonist opioids for their chronic pain. Due to the advantages of buprenorphine, the physician may recommend that a patient rotate to buprenorphine from other opioids. The following is a brief overview:
Why:
- Patients on long-term opioids, especially at high doses, may develop opioid-induced hyperalgesia (OIH), a condition in which the opioids themselves increase the severity of pain and ultimately prevent good pain control despite use of high doses. Buprenorphine reduces both OIH and central sensitization that also increases pain..
- Pain control is generally maintained or improved after rotation to buprenorphine – most studies report decreased pain severity (up to 27% in one study) and improved function after rotation.
- Buprenorphine may provide better pain control in some chronic pain conditions, including neuropathic pain and fibromyalgia. It is also safer than traditional opioids, especially for those with sleep apnea and those taking benzodiazepines. It is also less likely to develop tolerance over time or contribute to pain sensitization.
- Rotation to buprenorphine with microdosing protocols are effective and well-tolerated >95% of the time.
- It is not uncommon for patients who have transitioned to buprenorphine indicate they feel generally better with more clarity and less sluggishness after their transition.
- Adverse events are uncommon.
- Due to the politics of current pain management, access to high dose medications is becoming more difficult so rotation to buprenorphine offers better access and will likely be less expensive.
Who:
- Anyone taking any dose of opioids, who is interested in doing so.
- Especially recommended for those patients who feel their current opioid regimen does not provide them with adequate pain control.
- Especially recommended for those patients taking morphine, oxycodone, and fentanyl
- Especially recommended for those patients taking 100-300 morphine-equivalent (ME) doses, but also those patients taking >300 ME.
- Especially recommended for anyone who feels they may be having difficulty controlling their doses or may be running out early.
- Especially recommended for patients concurrently taking benzodiazepines (Xanax, Klonopin and Valium) who are unable to taper off of them.
In one study, pain reduction was highest for patients using morphine, oxycodone, and fentanyl before buprenorphine rotation. Using a pain scale of 0-10, there was a 3.7 point decrease in pain for those taking morphine, a 2.5 point decrease in pain for those taking oxycodone, and a 2.2 point decrease for those taking fentanyl. The smallest pain reduction of 1.1 was seen in those taking oxymorphone.
Patients taking between 100-199 mg morphine equivalent (ME) per day experienced the greatest reduction (2.7 points) in pain scores. followed by those taking 200 and 299 mg ME who exhibited a decrease of over 2 points on average. Patients taking > 400 mg ME reported the smallest reduction in pain scores, on average a 1.1 point decrease.
Methods of rotation from full opioids to buprenorphine
Rotating to buprenorphine from full agonist opioids may be done with two methods, the “Microdosing” method in which the rotation onto buprenorphine is gradual and overlapping with the full agonist opioid and the earlier traditional “Stop and Start” method, which involves discontinuing, and/or decreasing the opioid dose then discontinuing the opioid and starting the buprenorphine.
Microdosing” Method
The microdosing rotation method involves introducing very low-dose buprenorphine to the patient’s usual opioid regimen without initially, reducing the usual opioid dose. Gradually the buprenorphine dose is increased until a point at which the opioid may then be discontinued without precipitating withdrawal or triggering inadequate pain control. This microdosing method is relatively new and no definitive protocols have been established, but current protocols used at the VA and other pain management programs have provided encouraging data showing this protocol to be well tolerated and successful greater than 95% of the time.
“Stop and Start” Method
The “Stop and Start” method involves discontinuing, and or decreasing the opioid dose then discontinuing the opioid and starting the buprenorphine. This method often precipitates withdrawal symptoms and inadequately controlled pain, and as such as not well tolerated by some people, particularly those on high dose opioids.
The “Stop and Start” method historically has mostly often been engaged as a safety intervention when patients prescribed opioids for pain demonstrate safety concerns with their use of opioids and are therefore relatively abruptly discontinued from their opioids. The microdosing regimen however, is not limited to safety concerns, but is often recommended as a means of improving pain control and reducing side effects in situations unrelated to specific safety concerns.
When one chooses to convert other opioids to buprenorphine using a “Stop and Start” protocol, there are two scenarios, (1) conversion from a morphine equivalent of 90 or less and (2) conversion from a morphine equivalent of greater than 90.
Conversion from 90 ME or less:
-
- Discontinue the current opioid after taking the last bedtime dose
- Consider adding an adrenergic alpha agonist, such as clonidine or lofexidine to reduce potential risk of opioid withdrawal symptoms
- In the morning, initiate either Belbuca (buccal strip) at 150 – 300 µg strip every 12 hours or initiate Butrans (transdermal patch) at 10 – 20 µg/hour patch for weekly dosing
Conversion from >90 ME:
-
- Discontinue the current opioid after taking the last bedtime dose
- Consider adding an adrenergic alpha agonist, such as clonidine or lofexidine to reduce potential risk of opioid withdrawal symptoms
- In the morning, initiate either Belbuca (buccal strip) at 300 – 450 µg strip every 12 hours or initiate Butrans (transdermal patch) at 20 µg/hour patch for weekly dosing
What is the most important information I should know about taking Buprenorphine?
- Buprenorphine can cause death from overdose, especially if you take them with alcohol or sedatives such as Xanax, Valium or Klonopin. Use Buprenorphine exactly the way your doctor tells you to with medicines used to treat depression or anxiety.
- Use Buprenorphine only for the condition for which it was prescribed.
- Buprenorphine can cause drug dependence. This means that you can get withdrawal symptoms if you stop using it too quickly. Buprenorphine is not for occasional (“as needed”) use.
- Getting off buprenorphine can be accomplished without serious difficulty. The reason it sometimes has the reputation of being difficult to taper off is that the tapering is not done correctly. Buprenorphine is a potent opioid that should be tapered slowly; you should not simply stop taking it abruptly when you get down to a 1 or 2mg/day dose. Use of alternative buprenorphine formulations and tapering regimens can be engaged to make the final taper smooth and well tolerated. There is growing research to suggest that the use of gabapentin (Neurontin) may ease opioid withdrawal symptoms (See: Gabapentin). Additionally, the use of Synaptamine during the tapering process may make the tapering better tolerated.
- Prevent theft and misuse. Buprenorphine is a narcotic painkiller that can be a target for people who abuse prescription medicines or street drugs. Keep your buprenorphine locked in a safe place, to protect them from theft. Never give them to anyone else. Selling or giving away this medicine is against the law.
- In an emergency, have family members tell emergency room staff that you are being treated with buprenorphine, especially if being treated for a severely painful condition. Buprenorphine binds very tightly to the opioid receptors (see: Neurobiology of Opioids) that provide pain relief, more than most other opioids including hydrocodone, oxycodone and morphine. This means that in the event of an emergency that demands pain medicines for pain not controlled by currently prescribed buprenorphine, the emergency physician should use the best opioid for pain or the buprenophine may impair the effectiveness of the second opioid. There are multiple variables that will contribute to how effective a second opioid will be for the patient currently taking buprenorphine. This ineffectiveness may be
misinterpreted as drug-seeking by a physician not well informed regarding treating pain in patients who take buprenorphine. Perhaps the best two opioids for emergency use for managing pain in this emergency circumstance, either orally or intravenously, are hydromorphone (Dilaudid) or fentanyl. These two opioids have greater affinity for the opioid receptor than buprenorphine and should be effective for pain. That being said, caution is advised to avoid unintentional overmedication/overdose and careful monitoring should be employed. Whenever possible, always contact Dr. Ehlenberger (24/7) should you need to go to the emergency room for any condition, but especially for a painful condition.
Who Should Not Take Buprenorphine?
Do not take buprenorphine if:
- your doctor did not prescribe buprenorphine for you.
- you are allergic to buprenorphine, or any of the inactive ingredients in the medicines. See the end of this leaflet for a complete list of ingredients.
Your doctor should know about all your medical conditions before deciding if buprenorphine is right for you or what dose is best. Tell your doctor about all of your medical problems, especially the ones listed below:
- trouble breathing or lung problems
- head injury or brain problem
- liver or kidney problems
- gallbladder problems
- adrenal gland problems, such as Addison’s disease
- low thyroid (hypothyroidism
- enlarged prostate gland (men)
- problems urinating
- a curve in your spine that affects your breathing
- severe mental problems or hallucinations (seeing or hearing things that are not really there
- alcoholism
Tell your doctor:
- if you are pregnant or plan to become pregnant. Buprenorphine may not be right for you. It is not known whether buprenorphine could harm your baby.
- if you are breast feeding, buprenorphine will pass through your milk and may harm your baby.
- Tell your doctor about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. They may cause serious side effects when taken with buprenorphine. Sometimes, the doses of certain medicines and buprenorphine need to be reduced if used together.
- Do not take any other medicine, herbal, or over-the-counter medicine while using buprenorphine unless your doctor has told you it is okay.
How should I take Buprenorphine?
- Follow your doctor’s directions exactly. Your doctor may change your dose after seeing how the medicine affects you. Do not change your dose unless your doctor tells you to change it. Do not take buprenorphine more often than prescribed.
- Put the tablets or film under your tongue or against the cheek as directed and let them melt. This will take 2 to 10 minutes. Do not chew or swallow the tablets. The medicine will not work this way and you may get withdrawal symptoms.
- If your doctor tells you to take more than 1 tablet/film, you will be told to:
- take all tablet/films at the same time together under your tongue, or
- take 2 tablet/films, put them under your tongue. After they melt, put the next tablet/film under your tongue right away
- hold the tablet/film under your tongue until they melt completely. The medicine will not work if swallowed and you may get withdrawal symptoms.
- Do not change the way you are told to take your medicine or you may get too little or too much medicine.
- Do not inject (“shoot-up”) buprenorphine. Shooting-up is dangerous and you may get bad withdrawal symptoms.
- Buprenorphine can cause withdrawal symptoms if you take them too soon after using opiate drugs like morphine, oxycodone, hydrocodone or methadone.
- If you miss a dose of buprenorphine, take it as soon as possible. If it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not take 2 doses at once unless your doctor tells you to.
- Before discontinuing buprenorphine, ask your doctor how to avoid withdrawal symptoms.
- If you take too much buprenorphine or overdose, call your local emergency room or poison control center ASAP.
- If you discontinue taking buprenorphine, flush the unused tablets or strip down the toilet.
What Should I Avoid While Taking Buprenorphine?
- Do not drive, operate heavy machinery, or perform other dangerous activities until you know how this medicine affects you.
- Do not drink alcohol or take tranquilizers or sedatives (medicines that help you sleep) while using buprenorphine. You can die when you use these products with buprenorphine..
- Do not take other medicines without talking to your doctor. Other medicines include prescription and non-prescription medicines, vitamins, and herbal supplements. Be especially careful about medicines that may make you sleepy.
Potential Drug Interactions
There may also be a potential for a buprenorphine interaction with other drugs and compounds that induce or inhibit the cytochrome P-450 3A4 system, the enzyme system in the liver that metabolizes buprenorphine. There are many agents in this category and they include erythromycin, zileuton, and grapefruit juice and starfruit (inhibitors of metabolism), as well as carbamazepine, phenobarbital, phenytoin, and rifampin (inducers that enhance metabolism). In a study of the effects of the selective serotonin reuptake inhibitors (SSRIs) fluoxetine (Prozac) and fluvoxamine (Luvox), were both shown to inhibit buprenorphine metabolism, suggesting they may increase blood levels of buprenorphine if started on someone already taking buprenorphine.
What are the Possible Side Effects of Buprenorphine?
Some of the common side effects of buprenorphine are headache, drowsiness, problems sleeping, nausea, s
weating, stomach pain, and constipation.These are not all the possible side effects of buprenorphine, just some of the most common.
Call your doctor or get medical help right away if:
- You feel faint, dizzy, confused, or have any other unusual symptoms.
- Your breathing gets much slower than is normal for you. These can be signs of an overdose or serious problem.
- Buprenorphine can cause your blood pressure to drop, causing dizziness if you get up too fast from sitting or lying down.
- Buprenorphine can cause allergic reactions that can make it hard for you to breathe. Other symptoms of a bad allergic reaction include hives, swelling of your face, asthma (wheezing) or shock (loss of blood pressure and consciousness).
Call a doctor or get emergency help right away if you get any of these symptoms.
Buprenorphine may cause liver problems. Call your doctor right away if:
- Your skin or the white part of your eyes turns yellow (jaundice).
- Your urine turns dark.
- Your bowel movements (stools) turn light in color.
- You don’t feel like eating much food for several days or longer.
- You feel sick to your stomach (nausea).
- You have lower stomach pain.
Your doctor will do blood tests while you are taking buprenorphine to make sure your liver is okay.
Other considerations:
- You may get withdrawal symptoms when you start treatment with buprenorphine. To avoid this, be sure other opiates are out of your system before starting buprenorphine.
- Like with all opiates, you can develop dependence from taking buprenorphine, so you may get withdrawal symptoms when you stop taking buprenorphine. There is also a chance that you may abuse or get addicted to buprenorphine.
Genetic Testing
At Accurate Clinic we highly recommend genetic testing for our opioid patients. Through testing our patient’s DNA with a simple oral swab of saliva from the cheek, an individual’s ability to metabolize opioids and other medications by the liver can be evaluated. This information provides important insights as to how a patient may respond to various medications, including buprenorphine, and where side effects or drug interactions may be predicted, allowing for substantial safety benefits in prescribing.
Neurobiology of Buprenorphine – for those interested in understanding more…
As noted above, buprenorphine has characteristics that make it particularly effective in managing certain types of pain. This is because buprenorphine has different mechanisms of action that conventional opioids
See: Neurobiology of Opioids)
References:
Buprenorphine –Patient Information
- Buprenorphine Transdermal Patch: MedlinePlus Drug Information
- Buprenorphine – for Pain, Informed Consent
Buprenorphine – Overviews
- Buprenorphine – Considerations for Pain Management
- Sublingual Buprenorphine:Naloxone for Chronic Pain in At-Risk Patients – Development and Pilot Test of a Clinical Protocol
- Is Levorphanol a Better Option than Methadone – 2015
- Transdermal buprenorphine in clinical practice: a multicenter, noninterventional postmarketing study in the Czech Republic. – PubMed – NCBI
- clinical-update-on-the-pharmacology-efficacy-and-safety-of-transdermal-buprenorphine-pubmed-ncbi
- opioids-and-the-management-of-chronic-severe-pain-in-the-elderly-consensus-statement-of-an-international-expert-panel-with-focus-on-the-six-clinic-pubmed-ncbi
- buprenorphine-an-attractive-opioid-with-underutilized-potential-in-treatment-of-chronic-pain-2015
- twelve-reasons-for-considering-buprenorphine-as-a-frontline-analgesic-in-the-management-of-pain-pubmed-ncbi
- the-clinical-analgesic-efficacy-of-buprenorphine-pubmed-ncbi
- current-knowledge-of-buprenorphine-and-its-unique-pharmacological-profile-pubmed-ncbi
- equipotent-doses-of-transdermal-fentanyl-and-transdermal-buprenorphine-in-patients-with-cancer-and-noncancer-pain-results-of-a-retrospective-cohor-pubmed-ncbi
- transdermal-buprenorphine-in-cancer-pain-and-palliative-care-pubmed-ncbi
- safety-and-effectiveness-of-intravenous-morphine-for-episodic-breakthrough-pain-in-patients-receiving-transdermal-buprenorphine-pubmed-ncbi
- evaluation-of-the-tolerability-of-switching-patients-on-chronic-full-l-opioid-agonist-therapy-to-buccal-buprenorphine-2016
- buprenorphine-naloxone-therapy-in-pain-management-2014
- efficacy-and-tolerability-of-buccal-buprenorphine-in-opioid-experienced-patients-with-moderate-to-severe-chronic-low-back-pain-2016
- management-of-moderate-to-severe-chronic-low-back-pain-with-buprenorphine-buccal-film-using-novel-bioerodible-mucoadhesive-technology-2016
- the_clinical_analgesic_efficacy_of_buprenorphine
- effect-of-transdermal-opioids-in-experimentally-induced-superficial-deep-and-hyperalgesic-pain-2011
- a-clinical-trial-comparing-tapering-doses-of-buprenorphine-with-steady-doses-for-chronic-pain-and-co-existent-opioid-addiction-2010
Buprenorphine – Constipation
- Opioid-induced constipation_ rationale for the role of norbuprenorphine in buprenorphine-treated individuals – 2016
- Comparison of Pharmacological Activities of Buprenorphine and Norbuprenorphine – Norbuprenorphine Is a Potent Opioid Agonist – 2001
Buprenorphine – Drug Interactions
Buprenorphine – Opioid Tolerance, Hyperalgesia and NMDA Antagonism
- Buprenorphine – a review of its role in neuropathic pain
- Buprenorphine for neuropathic pain–targeting hyperalgesia. – PubMed – NCBI
- Transdermal buprenorphine controls central neuropathic pain. – PubMed – NCBI
- Pharmacologic Treatments for Neuropathic Pain
- Low-dose buprenorphine infusion to prevent postoperative hyperalgesia in patients undergoing major lung surgery and remifentanil infusion a double-blind, randomized, active-controlled trial – 2017
- Effects of opioid rotation to buprenorphine_naloxone on pain, pain thresholds, pain tolerance, and quality of life in patients with chronic pain and opioid use disorder – PubMed
- Conversion of chronic pain patients from full-opioid agonists to sublingual buprenorphine – PubMed – 2012
- Hyperalgesia in opioid-managed chronic pain and opioid-dependent patients – 2009
- Attitudes Towards and Management of Opioid-induced Hyperalgesia_ A Survey of Chronic Pain Practitioners – PubMed – 2029
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.