Acupuncture:
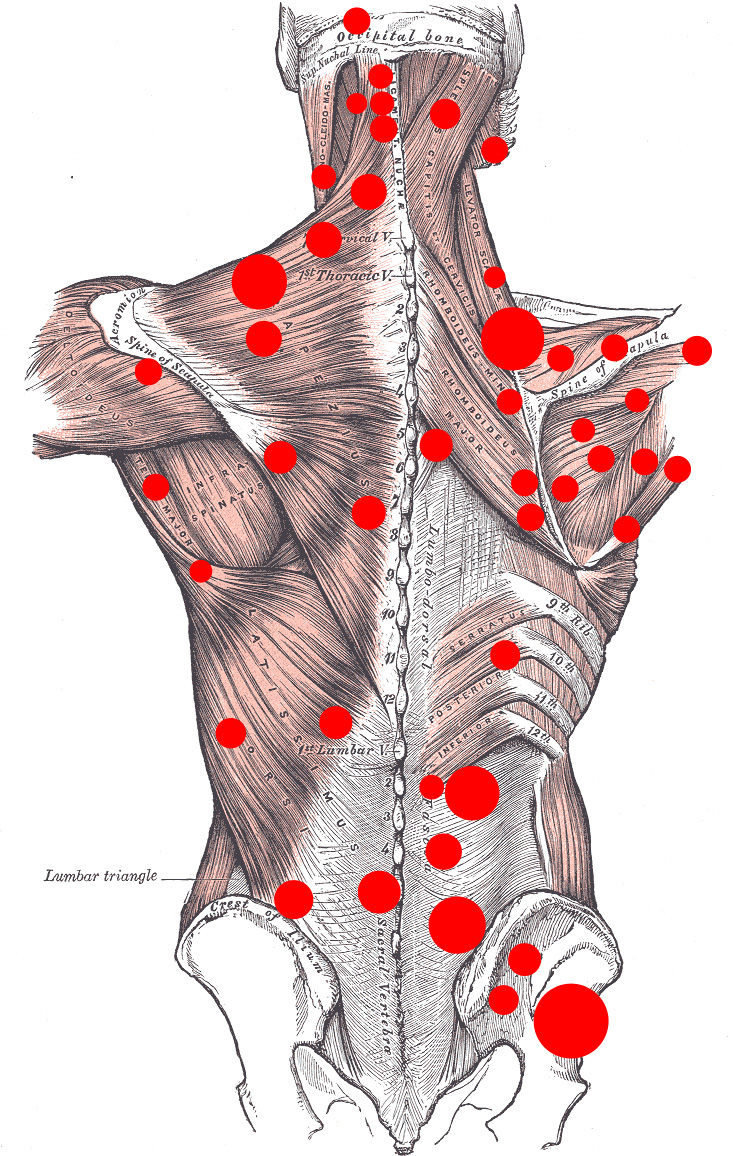
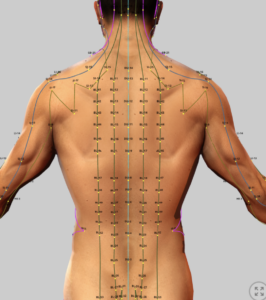
Trigger Points & Acupuncture Points
Trigger Points Acupuncture Points
Myofascial Pain:
- In Traditional Chinese Medicine (TCM) the presence of health and illness is based on the belief that there is a life energy that flows through the body through various channels called meridians. TCM focuses on balancing the body’s energy, or “Qi” (pronounced “chee”), which is believed to flow along the meridians. Any imbalance or blockage of the flow of Qi is believed to lead to illness. Acupuncture involves the insertion of thin needles into specific points along the meridians to stmulate the flow of Qi and alleviate pain and other conditions.
The treatment of myofacial pain associated with trigger points sometimes includes the insertion of acupuncture needles to provide relief of pain. This form of trigger point therapy has proven effective in the western medical community, and the question has been raised as to whether this form of trigger point therapy with acupuncture needles represents in actuality a form of acupuncture therapy despite the fact that the trigger points are identified with palpation of the muscle rather than identifying specific acupuncture points, lung specific meridians.
This section reviews studies that have evaluated this potential overlap between western trigger point therapy and Chinese acupuncture therapy.
See: Acupuncture (Introduction)
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
Definitions and Terms Related to Pain
Trigger Points & Acupuncture Points
Correlation of Myofascial Trigger Points and Acupuncture Points on Specific Meridians
This review examines studies evaluating the correlation between myofascial trigger points (MTrPs), as mapped in seminal work by Travell and Simons, Myofascial Pain and Dysfunction: The Trigger Point Manual by Janet G. Travell and David G. Simons, and acupuncture points on specific traditional Chinese medicine (TCM) meridians, focusing on the neck, shoulders, back, and extremities. It addresses the high prevalence of myofascial pain in chronic pain patients and assesses the anatomical, clinical, and physiological overlap between MTrPs and acupuncture points (classical, extra, and Ah-shi).
The evidence is drawn from key studies, with reference to the work by Travell and Simons, and includes recommendations for integrating these findings into pain management. (Of note, Janet Travell was the personal physician of John F. Kennedy who suffered greatly from multiple symptoms of chronic pain).
Myofascial Tissue
Myofascial tissue, also known as fascia, is a connective tissue that surrounds and supports muscles and other structures throughout the body. It’s a continuous network that provides structural support, protection, and allows for smooth movement. When healthy, it’s flexible and soft, but injury or inflammation can cause it to become tight and rigid, leading to pain and restricted movement.
- Myofascial tissue is a type of connective tissue that includes fascia and muscle tissue.
- Fascia is a thin, tough, and elastic tissue that wraps around muscles, bones, nerves, and organs, acting like a 3D spiderweb that connects the entire body.
- It provides support, stability, and allows for smooth movement between different structures.
- Myofascial tissue has an abundance of pain receptors throughout.
-
Support and protection:Myofascial tissue provides structural support to the body and protects internal organs.
-
Movement:It allows muscles and other tissues to slide smoothly against each other during movement, preventing friction and restriction.
-
Interconnectedness:
The fascial network connects different parts of the body, meaning that problems in one area can affect others.
-
Injury and inflammation:
Trauma or repetitive strain can cause myofascial tissue to become inflamed and tight, forming adhesions or knots.
-
Trigger points:
These tight areas within the fascia can cause pain, both at the site of the trigger point and in other areas of the body (referred pain).
-
Restricted movement:
Tight fascia can restrict muscle and joint movement, leading to pain, stiffness, and reduced range of motion.
-
Myofascial pain syndrome:
This condition is characterized by chronic pain caused by problems in the myofascial tissue.
-
What it is:
Myofascial release is a type of therapy that aims to relieve pain and improve movement by releasing tension in the myofascial tissue.
-
How it works:
Therapists use gentle, sustained pressure to release restrictions in the fascia and restore its flexibility.
-
Benefits:Myofascial release can help reduce pain, improve range of motion, and improve overall function.
Background: Travell and Simons’ Trigger Point Manual
- Reference: Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual. Vol 1 (Upper Half of Body, 1983; 2nd ed., 1999), Vol 2 (Lower Half of Body, 1992), 3rd ed. (combined, 2019). Baltimore: Williams & Wilkins.
- Content: The manuals map 255 common MTrPs across skeletal muscles, detailing their locations, referred pain patterns, and clinical effects (e.g., pain, dysfunction, autonomic symptoms). MTrPs are hypersensitive nodules in taut muscle bands, causing local or referred pain. The 3rd edition classifies pain into Muscle Belly Pain (85.4%), Origin-Insertion Pain (80.9%), and Referred Pain (59.5%), enhancing diagnostic precision.
- Relevance: Provides the standard for MTrP identification, widely used in pain management for conditions like neck pain, shoulder pain, low back pain, and extremity pain.
Evidence on Correlation Between MTrPs and Acupuncture Points
Several studies have investigated the overlap between MTrPs and acupuncture points, focusing on anatomical locations, pain indications, and referred pain patterns aligning with TCM meridians. The following summarizes key findings, with specific examples for neck, shoulders, back, and extremities.
1. Anatomical Correspondence
- Melzack et al. (1977):
- Study: Compared 56 MTrPs from early myofascial pain literature with TCM acupuncture points used for regional pain. Found 71% correspondence in spatial distribution and pain indications, suggesting MTrPs and acupuncture points may represent the same phenomenon.
- Critique: Birch (2003) argued the 71% figure is inflated, as 61% of acupuncture points studied were not recommended for pain, suggesting only 18–19% correlate with MTrPs for pain treatment. The study focused on Ah-shi points (tender spots), not classical or extra points, limiting meridian-specific conclusions.
- Relevance: Established early evidence of overlap, though not meridian-specific.
- Dorsher (2006, 2009):
- Study (2006): Analyzed 255 MTrPs from Travell and Simons’ 1st edition against 386 TCM acupuncture points. Found 92% anatomical correspondence (238/255 MTrPs within 3 cm of a classical acupuncture point, entering the same muscle). 79.5% shared local pain indications.
- Study (2009): Examined referred pain patterns of 238 MTrP-acupuncture point pairs. Found 81.5% complete/near-complete correlation between MTrP referred pain and corresponding meridian distributions, with 9.5% partial correlation and 9% minimal/no correlation. Strongest correlations in extremities (e.g., Bladder meridian for soleus MTrP), weaker in anterior neck/chest.
- Examples:
- Neck/Shoulder (Trapezius, TrP3): Refers pain to upper trapezius and GB20/GB21 (Gallbladder meridian). GB21 (Jianjing) at trapezius midpoint aligns with TrP3, used for neck/shoulder pain.
- Shoulder (Infraspinatus, TrP1): Refers pain to anterior shoulder/arm, aligning with Large Intestine meridian (LI14, Binao).
- Back (Quadratus Lumborum, TrP1): Refers pain to sacroiliac region, corresponding to Bladder meridian (BL25, Dachangshu).
- Extremity (Soleus, TrP1): Refers pain to heel, aligning with Bladder meridian (BL57, Chengshan), used for heel pain/cramps.
- Critique: Simons and Dommerholt (2007) noted that Travell’s MTrP locations are indicative, not exhaustive, and additional MTrPs exist. Dorsher’s high correspondence may overestimate overlap due to broad definitions of acupuncture points.
- Liu et al. (2016):
- Study: Reviewed anatomical overlap between MTrPs and TCM acupuncture points, including primary channel, extra, and Ah-shi points. Found significant correlation, particularly with Ah-shi points, suggesting MTrPs and acupuncture points share stimulation sites. Proposed that MTrP research could inform Ah-shi point studies.
- Relevance: Emphasized Ah-shi points’ similarity to MTrPs, supporting their use in pain management but less meridian-specific.
2. Clinical and Physiological Correspondence
- Melzack et al. (1977): Suggested shared neural mechanisms (e.g., gate control theory), where MTrP stimulation (dry needling) or acupuncture activates Aδ and C fibers, modulating pain via central nervous system inhibition.
- Dorsher (2009): Found 97% correlation for pain treatment and 93% for somatovisceral conditions between MTrPs and acupuncture points. Referred pain patterns (e.g., soleus MTrP to heel) closely followed meridian pathways (e.g., Bladder meridian), suggesting physiological overlap via peripheral and central nervous system sensitization.
- Lee et al. (2022): Highlighted that MTrPs most closely resemble Ah-shi points due to shared tenderness and patient-reported pain. Classical points (e.g., LI10, SP10) in muscles like brachioradialis or vastus medialis also overlap with MTrPs, with referred pain aligning with meridian indications (e.g., LI10 for digestive issues).
- Examples:
- Neck (Sternocleidomastoid, TrP1): Refers pain to occiput, aligning with Gallbladder meridian (GB20, Fengchi).
- Shoulder (Supraspinatus, TrP1): Refers pain to elbow, corresponding to Large Intestine meridian (LI15, Jianyu).
- Back (Erector Spinae, TrP2): Refers pain to lower back/buttock, aligning with Bladder meridian (BL23, Shenshu).
- Extremity (Brachioradialis, TrP1): Refers pain to wrist/thumb, aligning with Large Intestine meridian (LI10, Shousanli).
3. Specific Meridian Correlations
- Gallbladder Meridian (GB): Common for neck/shoulder pain (e.g., GB20, GB21 for trapezius MTrPs). GB30 (Huantiao) in gluteus medius aligns with buttock pain MTrPs.
- Bladder Meridian (BL): Frequent for back and lower extremity pain (e.g., BL57 in soleus, BL25 in quadratus lumborum). Referred pain patterns closely follow BL meridian pathways.
- Large Intestine Meridian (LI): Relevant for shoulder and upper extremity pain (e.g., LI15 in supraspinatus, LI10 in brachioradialis).
- Stomach Meridian (ST): Less consistent for trunk pain (e.g., ST21 in rectus abdominis), but strong for lower extremity pain (e.g., ST36, Zusanli, for tibialis anterior MTrPs).
- Ah-shi Points: Non-fixed tender points, highly correlated with MTrPs due to palpation-based identification. Most relevant for localized pain in your patients.
4. Treatment Implications
- Acupuncture and Dry Needling: Studies (e.g., Tough et al., 2009) show acupuncture and dry needling targeting MTrPs (often Ah-shi or classical points) reduce pain in neck/shoulder (e.g., trapezius) and back. A 2018 RCT found superficial acupuncture on trapezius MTrPs as effective as traditional acupuncture, with less post-treatment soreness.
- Pain Management: Integrating MTrP and acupuncture point knowledge allows targeted therapy. For example, needling GB21 (trapezius) or BL57 (soleus) addresses both MTrP pain and meridian indications, enhancing outcomes in chronic pain patients.
Strength of Evidence
- Quality: Moderate. Studies like Dorsher (2006, 2009) and Melzack (1977) provide robust anatomical and clinical data, but reliance on Travell’s maps and subjective referred pain limits objectivity. No gold standard (e.g., imaging) confirms MTrPs.
- Consistency: High for anatomical overlap (92–93%) and referred pain-meridian correlation (81.5–91%), especially in extremities. Weaker in anterior neck/chest due to fewer MTrPs mapped.
- Clinical Significance: Strong for pain management, as MTrP-acupuncture point overlap supports targeted needling. Ah-shi points align closely with MTrPs, enhancing practical utility in your practice.
- Gaps: Limited RCTs comparing MTrP and acupuncture point stimulation. Variability in acupuncture point definitions (e.g., classical vs. Ah-shi) and lack of meridian-specific studies hinder precision.
Clinical Recommendations
For chronic pain patients with MTrPs in the neck, shoulders, back, and extremities:
- Assessment: Use Travell and Simons’ maps to identify MTrPs (e.g., trapezius TrP3, quadratus lumborum TrP1) and cross-reference with TCM points (e.g., GB21, BL25) for targeted therapy.
- Treatment: Combine dry needling (for MTrPs) and acupuncture (for meridian-based effects) to address local and referred pain. Focus on Ah-shi points for immediate relief and classical points (e.g., GB20, LI15) for systemic benefits.
- Monitoring: Track pain reduction using VAS scores and range of motion, as in Aranha et al. (2015) for cervical MTrPs.
- Integration with Other Therapies: Combine with omega-3 supplementation (1–2.7 g/day EPA + DHA) to reduce inflammation, as per Wen Deng et al. (2023), and monitor Eliquis interactions.
Conclusion
Studies confirm a high correlation (71–93%) between MTrPs, as mapped by Travell and Simons, and TCM acupuncture points, particularly Ah-shi points, with 81.5–91% of referred pain patterns aligning with meridians like Gallbladder, Bladder, and Large Intestine. Neck (e.g., trapezius-GB21), shoulder (e.g., infraspinatus-LI15), back (e.g., quadratus lumborum-BL25), and extremity (e.g., soleus-BL57) MTrPs show strong anatomical and clinical overlap. These findings support integrating MTrP and acupuncture therapies in pain management, enhancing outcomes for your patients. Further RCTs are needed to validate meridian-specific effects and optimize treatment protocols.
Proposed mechanism of the flow of key through my facial tissues
Based on the anatomical features of myofascial tissue surrounding muscles and organs throughout the body, a theory has been proposed that the flow of Qi through myofascial tissues outside the established 12 Chinese meridians may explain the benefits of treating myofascial trigger points with acupuncture stimulation, despite the trigger point not matching exactly with an established acupuncture point on a meridian.
Key References
- Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual. Vol 1 (2nd ed., 1999), Vol 2 (1992), 3rd ed. (2019). Baltimore: Williams & Wilkins.
- Melzack R, et al. (1977). Trigger points and acupuncture points for pain: Correlations and implications. Pain, 3(1):3–23. doi: 10.1016/0304-3959(77)90032-X.
- Dorsher PT. (2006). Trigger points and acupuncture points: Anatomic and clinical correlations. Medical Acupuncture, 17(3):21–25.
- Dorsher PT. (2009). Myofascial referred-pain data provide physiologic evidence of acupuncture meridians. The Journal of Pain, 10(7):723–731. doi: 10.1016/j.jpain.2008.12.010.
- Liu L, et al. (2016). Traditional Chinese Medicine acupuncture and myofascial trigger needling: The same stimulation points? Complementary Therapies in Medicine, 26:28–32. doi: 10.1016/j.ctim.2016.02.013.
- Lee S, et al. (2022). Similarities between Ashi acupoints and myofascial trigger points: Exploring the relationship between body surface treatment points. Frontiers in Neuroscience, 16:947884. doi: 10.3389/fnins.2022.947884.
- Tough EA, et al. (2009). Acupuncture and dry needling in the management of myofascial trigger point pain: A systematic review and meta-analysis. European Spine Journal, 18(1):3–18. doi: 10.1007/s00586-008-0787-8.
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
.