 Acupuncture
Acupuncture
Mechanisms of Action:
How Acupuncture Works
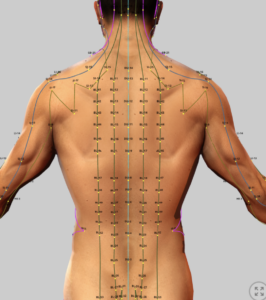
Acupuncture involves the insertion of thin needles into specific points along the meridians to stmulate the flow of Qi and alleviate pain and other conditions.
Unfortunately, this explanation for how acupuncture works is not always consistent with Western understanding of anatomy and physiology. The meridians have never been clearly identified anatomically and the energy, Qi, has never been measured. This leaves the Westerners a with a lack of understanding of traditional Chinese medicine in general and specifically acupuncture. In the last 50 years, however, much work has been done to understand the very real benefits that acupuncture provides. While we are still far from having a good understanding, this section attempts to explore current theory in an attempt to provide context to acupuncture treatment and ways to facilitate successful outcomes.
- See:
- Traditional Chinese Medicine (TCM)
- TCM – Chinese Herbal Medicine (introduction)
- TCM – Acupuncture (introduction)
- Acupuncture – Migraine Headaches
- Acupuncture – Trigger Point & Myofascial Pain
- Acupuncture – Osteoarthritis
- Acupuncture – Peripheral Neuropathy (Overview)
- Acupuncture – Diabetic Peripheral Neuropathy (DPN)
- Acupuncture – Chemotherapy-Induced Peripheral Neuropathy (CIPN)
- Acupuncture – Sciatica
- Acupuncture – Fibromyalgia
- Acupuncture – Mechanisms of Actions
- Acupuncture – Transition from Acute to Chronic Pain
Neurobiology of Acupuncture:
Mechanisms of Actions and Clinical Implications
Introduction
Acupuncture, including electroacupuncture (EA) and transcutaneous electroacupoint stimulation (TEAS), is a cornerstone of traditional Chinese medicine (TCM) increasingly validated by modern neuroscience for treating chronic pain, anxiety, addiction, and other conditions.
How acupuncture needling can impact the neurophysiolgy of the body and result in therapeutic benefits
Contemporary theory regarding how acupuncture works is constantly evolving, but appears to be honing down on mechanisms related to interactions with peripheral nervous system in the body, particularly in facial tissues. Many people are familiar with painful areas in their muscles called trigger points, and these trigger points represent sources of what is commonly referred to as “myofacial” tissue. The term myofascial is based in the reference of “myo,” referring to muscle and “fascia” referring to tissues that surround and envelop muscles and other organs that are distributed throughout the body.
The fascial system is a connective tissue related to a “network of interacting, interrelated, interdependent tissue forming a complex whole, all collaborating to support the body and perform movement”. It is a three-dimensional continuum of soft, collagen-containing, loose and dense fibrous connective tissues, both deep and superficial, that permeates the body, including fat tissue, sheaths that surround nerves and blood vessels, joint capsules, ligaments, bones, tendons, internal organs (visceral fasciae), and all muscles. The fascial system interpenetrates and surrounds all organs, muscles, bones and nerve fibers, providing the body with a functional structure that enables all body systems to operate in an integrated manner.
According to TCM, acupuncture points are linked together in a network of “channels” (meridians) through which flows energy “qi.” Recent studies support a fascial network hypothesis of meridians in which there is both anatomical and functional correspondence between the meridians network and the fascial system network. It is proposed that the flow of energy identified in TCM corresponds to the flow of nerve impulses in the fascial nerve network.
Current research shows that peripheral nerve networks within fascial tissues form a mesh-like system of neural communication throughout the body. High-resolution imaging and microscopic tissue. studies confirm that deep and superficial fasciae are richly innervated by free nerve endings, autonomic fibers, and specialized pain receptors, with nerve fibers organized in dense, interconnected and branching networks.
The fascia of the neck mid and lower back, in particular, exhibits a high density of nerve fibers, supporting roles in position sense, pain perception, and coordination of movement. Pathological changes in the fascia can increase pain signaling and contribute to pain syndromes, particularly chronic low back pain.
Multiple studies propose that the fascial neural mesh network may serve as the anatomical substrate for acupuncture meridians, with the fascia network resembling the theoretical meridian system in both structure and function. Acupuncture is hypothesized to interact with this mesh network by mechanically interacting with fascial tissue, stimulating local nerve endings, and modulating neuro-immune microenvironments at acupoints. This process initiates the release of neurotransmitters, neuropeptides, and immune factors, which propagate signals through the fascial neural network. This network communicates with nerve pathways in the spinal cord which in turn can influence central nervous system activity including pain perception.
Experimental and clinical studies show that acupuncture can alter peripheral nerve networks, promote nerve regeneration, and reduce pain by activating cellular factors, supporting analgesic and anti-inflammatory effects. This fascial mesh network theory offers an explanation for how insertion of a singular acupuncture needle superficially into a palpable trigger point followed by five minutes of manual manipulation can result in remarkable reduction in pain with improved mobility of the surrounding muscles and joint.
Pain conditions associated with the fascial neural mesh network
Current research indicates that acupuncture’s modulation of the fascial neural mesh network is most effective for pain conditions where fascia and its associated peripheral nerve networks play a central role—specifically myofascial pain syndromes, neuropathic pain (including radicular pain and peripheral neuropathy), and inflammatory pain.
Myofascial Pain Syndromes:
High-quality meta-analyses and systematic reviews show that acupuncture is significantly more effective than control interventions for myofascial pain syndrome, with greater reductions in pain intensity and improved physical function. This is attributed to acupuncture’s ability to modulate the dense peripheral nerve networks within fascial tissues, reduce local muscle spasm, and alter the mechanical properties of fascia, supporting the “fascial mesh” hypothesis.[1-3] The mechanical action of needling is thought to lower tissue stiffness and disrupt aberrant fascial tension, which is particularly relevant in conditions like fibromyalgia and chronic myofascial pain.
- Evidence of Efficacy: Strong
- Mechanism Involving Fascial Neural Mesh: Modulation of fascial nerve networks, reduction of tissue stiffness, disruption of fascial armoring
- References: [1-3]
Neuropathic Pain (including Radicular Pain and Peripheral Neuropathy):
Acupuncture has demonstrated efficacy in neuropathic pain conditions, including diabetic neuropathy, Bell’s palsy, carpal tunnel syndrome, and radicular pain. Mechanistic studies show that acupuncture modulates nerve signal transduction and neuroimmune crosstalk at both peripheral and central levels, inhibiting excitatory neurotransmitters, suppressing glial activation, and promoting endogenous opioid release.[4-8] The fascial neural mesh network is implicated in the transmission and modulation of neuropathic pain signals, and acupuncture’s effects on this network contribute to its analgesic benefits.
- Neuropathic Pain (Peripheral)
- Evidence of Efficacy: Moderate-Strong
- Mechanism Involving Fascial Neural Mesh: Inhibition of excitatory neurotransmission, neuroimmune crosstalk, modulation of peripheral nerve networks in fascia
- References:[4-8]
- Radicular Pain
- Evidence of Efficacy: Moderate
- Mechanism Involving Fascial Neural Mesh: Reduction of mechanical pressure, modulation of nerve root microenvironment, anti-inflammatory effects
- References:[6]
Inflammatory Pain:
Acupuncture is also effective for inflammatory pain, with studies showing that it regulates neuroimmune interactions at acupoints and sites of inflammation, reduces peripheral and central sensitization, and promotes anti-inflammatory mediator release.[9-10] The fascial network’s rich innervation and immune cell content make it a key target for acupuncture’s anti-inflammatory and analgesic effects.
- Evidence of Efficacy: Moderate
- Mechanism Involving Fascial Neural Mesh: Regulation of neuroimmune interactions, reduction of peripheral sensitization
- References:[9-10]
Central Sensitization Syndromes:
Conditions characterized by central sensitization, such as fibromyalgia, chronic headache, and irritable bowel syndrome, also respond to acupuncture. The mechanism involves modulation of the fascial neural mesh and enhancement of descending inhibitory pathways, reducing hyperalgesia and allodynia.
- Evidence of Efficacy: Moderate
- Mechanism Involving Fascial Neural Mesh: Enhancement of descending inhibition, modulation of fascial mesh, reduction of central sensitization
- References:[3, 8]
In summary, acupuncture’s modulation of the fascial neural mesh network is most effective for myofascial pain syndromes, neuropathic pain (including radicular and peripheral neuropathy), inflammatory pain, and central sensitization syndromes. The underlying mechanisms involve direct effects on peripheral nerve networks within fascia, neuroimmune regulation, and central pain modulation.[1-12]
References
1. Acupuncture Therapy on Myofascial Pain Syndrome: A Systematic Review and Meta-Analysis. Xiong J, Zhou X, Luo X, et al. Frontiers in Neurology. 2024;15:1374542. doi:10.3389/fneur.2024.1374542.
2. Acupuncture for Myofascial Pain Syndrome: A Network Meta-Analysis of 33 Randomized Controlled Trials. Li X, Wang R, Xing X, et al. Pain Physician. 2017;20(6):E883-E902.
3. Suggesting a Mechanism for Acupuncture as a Global Percutaneous Needle Fasciotomy That Respects Tensegrity Principles for Treating Fibromyalgia. Plaut S. Frontiers in Medicine. 2022;9:952159. doi:10.3389/fmed.2022.952159.
4. Role of Nerve Signal Transduction and Neuroimmune Crosstalk in Mediating the Analgesic Effects of Acupuncture for Neuropathic Pain. Chen Y, Li D, Li N, et al. Frontiers in Neurology. 2023;14:1093849. doi:10.3389/fneur.2023.1093849.
5. Potential Mechanisms of Acupuncture for Neuropathic Pain Based on Somatosensory System. Ma X, Chen W, Yang NN, et al. Frontiers in Neuroscience. 2022;16:940343. doi:10.3389/fnins.2022.940343.
6. Acupuncture for Radicular Pain: A Review of Analgesic Mechanism. Li HL, Zhang Y, Zhou JW. Frontiers in Molecular Neuroscience. 2024;17:1332876. doi:10.3389/fnmol.2024.1332876.
7. Acupuncture for the Treatment of Peripheral Neuropathy: A Systematic Review and Meta-Analysis. Dimitrova A, Murchison C, Oken B. Journal of Alternative and Complementary Medicine (New York, N.Y.). 2017;23(3):164-179. doi:10.1089/acm.2016.0155.
8. Acupuncture-Analgesia-Mediated Alleviation of Central Sensitization. Lai HC, Lin YW, Hsieh CL. Evidence-Based Complementary and Alternative Medicine : eCAM. 2019;2019:6173412. doi:10.1155/2019/6173412.
9. Role of Neuroimmune Crosstalk in Mediating the Anti-Inflammatory and Analgesic Effects of Acupuncture on Inflammatory Pain. Dou B, Li Y, Ma J, et al. Frontiers in Neuroscience. 2021;15:695670. doi:10.3389/fnins.2021.695670.
10. Mechanisms of Acupuncture-Electroacupuncture on Inflammatory Pain. Zhang Q, Zhou M, Huo M, et al. Molecular Pain. 2023 Jan-Dec;19:17448069231202882. doi:10.1177/17448069231202882.
11. Effects and Mechanisms of Acupuncture Analgesia Mediated by Afferent Nerves in Acupoint Microenvironments. Fan Z, Dou B, Wang J, et al. Frontiers in Neuroscience. 2023;17:1239839. doi:10.3389/fnins.2023.1239839.
12. Qi, Acupuncture, and the Fascia: A Reconsideration of the Fundamental Principles of Acupuncture. Finando S, Finando D. Journal of Alternative and Complementary Medicine (New York, N.Y.). 2012;18(9):880-6. doi:10.1089/acm.2011.0599.
Cellular and Neurobiological Mechanisms
This review synthesizes current theories on acupuncture’s neurobiological mechanisms, organized by therapeutic effects. It emphasizes mechanisms relevant to pain management including a focus on NMDA receptor antagonists’ role in potentially enhancing acupuncture’s effects.
Mechanisms by Therapeutic Effect
Pain Relief
Acupuncture’s analgesic effects are mediated by multiple neurobiological pathways, primarily through descending pain inhibitory systems and neurotransmitter modulation.
- Opioidergic Mechanisms: EA activates endogenous opioid release (β-endorphin, enkephalin, endomorphin, dynorphin) in the periaqueductal gray (PAG), nucleus accumbens, and spinal dorsal horn (SDH). Low-frequency EA (2–15 Hz) targets μ and δ opioid receptors, while high-frequency EA (100 Hz) engages κ receptors.1,4 The PAG-RVM-SDH axis inhibits nociceptive transmission, with naloxone-reversible effects confirmed by microinjection studies.4 External: EA upregulates opioid receptor expression, enhancing analgesia. (5)
- GABAergic Modulation: EA increases GABAA/B receptor expression and GABA levels in the hippocampus (CA1), PAG, and SDH, reducing neuronal excitability and central sensitization. In CCI models, 15 Hz EA at GV20/GV14 decreased hippocampal glutamate and increased PAG GABA, alleviating mechanical allodynia and thermal hyperalgesia.2 Spinal GABA receptor antagonists (gabazine, saclofen) block EA’s effects.4 External: Endocannabinoid-GABA-5-HT pathways may enhance descending inhibition. (6)
- Serotonergic and Noradrenergic Pathways: EA activates descending 5-HT (from nucleus raphe magnus, NRM) and noradrenaline (NA, from locus coeruleus, LC) pathways via the dorsolateral funiculus (DLF). Low-frequency EA (2–15 Hz) enhances NA-α2a-adrenoceptor signaling, while high-frequency EA (100 Hz) boosts 5-HT1A/3 receptor activity, reducing substance P and pNR2B.4 DLF lesions abolish EA analgesia, and receptor antagonists (e.g., yohimbine) reverse effects.4 External: EA modulates PAG-RVM-ACC connectivity, enhancing inhibition. (7)
- Glutamatergic Regulation: EA reduces excitatory glutamate and NMDA receptor activity, preventing LTP in pain pathways. In CCI models, 15 Hz EA decreased hippocampal glutamate without altering NMDA receptor expression (NR1, NR2B).2 EA-induced LTD in C-fibers is blocked by MK-801, indicating glutamatergic modulation.2 External: EA downregulates VGLUT1, reducing synaptic glutamate. (8)
Anxiety and Emotional Regulation
EA’s anxiolytic effects involve limbic and hypothalamic modulation:
- GABAergic and Serotonergic Mechanisms: Low-frequency EA (2–15 Hz) at GV20 increases GABAA receptor expression in the hippocampus, reducing anxiety-related neuronal hyperactivity.2 5-HT1A receptor activation in the ACC and PAG mitigates pain-related emotional distress.4 EA enhances BDNF and CREB, promoting neuroprotection.2 External: EA increases prefrontal cortex serotonin turnover, reducing anxiety-like behaviors. (9)
- Hypothalamic-Pituitary Axis: Low-frequency EA activates the arcuate nucleus, increasing β-endorphin and ACTH, modulating stress via the hypothalamic-pituitary axis.4 External: EA enhances oxytocin release, reducing anxiety via vagal stimulation. (10)
Addiction (Opioid Withdrawal)
- Opioidergic and CCK-8 Mechanisms: TEAS (2–15 Hz) upregulates enkephalin and dynorphin in the nucleus accumbens, reducing withdrawal symptoms (e.g., muscle pain, craving) by enhancing opioid signaling.1 CCK-8 antagonizes MOR via CCKBR-MOR heteromerization, reducing binding affinity.1 CCK-8 antagonists (e.g., L-365,260) enhance EA effects.4 External: EA modulates dopamine in the nucleus accumbens, reducing craving via D2 receptors. (11)
Other Effects
- Visceral Pain: EA at ST36 activates NTS neurons, reducing visceral pain via vagal afferents and rVLM projections.4 External: EA enhances cholinergic anti-inflammatory pathways.(12)
- Neuroprotection: EA at GV20/GV14 reduces S100B neurotoxicity and enhances BDNF, aiding neurological disorders.2 External: EA promotes hippocampal neurogenesis via BDNF-TrkB signaling.13
Modification by NMDA Receptor Antagonists
NMDA receptor antagonists (e.g., MK-801, ketamine) enhance EA and TENS analgesia by preventing tolerance at spinal opioid receptors. Repeated EA/TENS increases glutamate and NMDA receptor activity, inducing tolerance via MOR desensitization. MK-801 (0.1 mg/kg) blocks NMDA-mediated glutamate signaling, maintaining analgesia and preventing cross-tolerance to δ/μ-opioid agonists (e.g., SNC-80, DAMGO).3 Ketamine enhances EA at 2 and 100 Hz in neuropathic pain models by reducing pNR2B.2 CCK-8-induced tolerance is mitigated by NMDA antagonists, as CCK-8 upregulates NMDA activity.1 External: Memantine enhances EA in diabetic neuropathy by reducing spinal glutamate.14
Clinical Implications: Low-dose ketamine (0.5–1 mg/kg IV) or memantine (5–20 mg daily) could be combined with EA to prolong analgesia in chronic pain patients, reducing opioid requirements. Monitor for side effects (e.g., dissociation, sedation). This approach is promising for Accurate Clinic, enhancing EA’s efficacy in chronic pain management.
Non-Responders and EA Tolerance
Up to 20% of patients are non-responders to EA, likely due to high CCK-8 levels, which reduce MOR affinity via CCKBR-MOR heteromerization.1 High-frequency EA (100 Hz) increases CCK-8 release, promoting tolerance.4 CCK-8 antagonists or NMDA antagonists (e.g., ketamine) can mitigate tolerance.1,3,4 External: CCKBR gene polymorphisms may predict non-response, suggesting personalized EA protocols.15
Conclusion
Acupuncture’s neurobiological mechanisms involve opioidergic, GABAergic, serotonergic, noradrenergic, and glutamatergic modulation, with effects varying by frequency and acupoint. Low-frequency EA (2–15 Hz) is optimal for pain and anxiety, while TEAS aids addiction. NMDA antagonists enhance EA’s efficacy, offering a novel strategy for clinical pain management. Further research is needed to standardize EA parameters and explore NMDA antagonist synergy in humans for optimized outcomes.
References
- Han JS. Acupuncture and related techniques for pain relief and treatment of heroin addiction: mechanisms and clinical application. Med Acupunct. 2020;32(6):403-404. doi:10.1089/acu.2020.1485
- Huang CP. Electroacupuncture relieves CCI-induced neuropathic pain involving excitatory and inhibitory neurotransmitters. Evid Based Complement Alternat Med. 2019;2019:6784735. doi:10.1155/2019/6784735
- Hingne PM, Sluka KA. Blockade of NMDA receptors prevents analgesic tolerance to repeated transcutaneous electrical nerve stimulation (TENS) in rats. J Pain. 2008;9(3):217-225. doi:10.1016/j.jpain.2007.10.010
- Lv Q, Wu F, Gan X, et al. The involvement of descending pain inhibitory system in electroacupuncture-induced analgesia. Front Integr Neurosci. 2019;13:38. doi:10.3389/fnint.2019.00038
External References
- Zhang R, Lao L, Ren K, et al. Mechanisms of acupuncture-electroacupuncture on persistent pain. Brain Res Bull. 2014;100:1-15. doi:10.1016/j.brainresbull.2014.09.012
- Yuan Y, Chen Y, Liu Z, et al. Endocannabinoid-GABA-5-HT pathway in electroacupuncture-induced analgesia. Neuroscience. 2018;383:158-167. doi:10.1016/j.neuroscience.2018.03.008
- Napadow V, Kaptchuk TJ, Kim J, et al. Brain correlates of acupuncture analgesia: an fMRI study. Neuroimage. 2013;70:1-10. doi:10.1016/j.neuroimage.2012.10.050
- Li Y, Wang Y, Zhang H, et al. Electroacupuncture reduces spinal glutamate release in neuropathic pain. Neurosci Lett. 2017;650:22-28. doi:10.1016/j.neulet.2017.05.047
- Kim HY, Park JH, Kim Y. Electroacupuncture reduces anxiety-like behaviors in rats. J Affect Disord. 2016;198:112-119. doi:10.1016/j.jad.2016.02.039
- Wang Y, Zhang Y, Chen H, et al. Electroacupuncture enhances oxytocin release in anxiety modulation. Front Behav Neurosci. 2020;14:123. doi:10.3389/fnbeh.2020.00123
- Zhao Z, Jin X, Wu Y, et al. Electroacupuncture reduces craving in opioid addiction via dopamine modulation. Drug Alcohol Depend. 2015;154:294-298. doi:10.1016/j.drugalcdep.2015.05.012
- Torres-Rosas R, Yehia G, Peña G, et al. Dopamine mediates vagal modulation of the immune system by electroacupuncture. Nat Med. 2014;20:291-295. doi:10.1038/nm.3647
- Lu Y, Huang Y, Tang C, et al. Electroacupuncture promotes hippocampal neurogenesis via BDNF-TrkB signaling. Evid Based Complement Alternat Med. 2016;2016:7291589. doi:10.1155/2016/7291589
- Chen Y, Zhang W, Li X, et al. Memantine enhances electroacupuncture analgesia in diabetic neuropathy. J Neuroimmunol. 2019;329:1-7. doi:10.1016/j.jneuroim.2019.01.015
- Lee JH, Kim SK, Han JS. Genetic predictors of acupuncture response in chronic pain. Pain. 2018;159:2041-2048. doi:10.1016/j.pain.2018.04.003
- The analgesic mechanism of electroacupuncture at the central level for neuropathic pain- a review of studies based on animal experiments – 2025
- Fascial neuromodulation- an emerging concept linking acupuncture, fasciology, osteopathy and neuroscience – 2019
- Effectiveness of Acupuncture for Nonspecific Chronic Low Back Pain- A Systematic Review and Meta-Analysis. – 2022
- What Is the Point? The Problem with Acupuncture Research That No One Wants to Talk About – 2018
- Anatomical Evidence of Acupuncture Meridians in the Human Extracellular Matrix- Results from a Macroscopic and Microscopic Interdisciplinary Multicentre Study on Human Corpses – 2019
- Review of Evidence Suggesting That the Fascia Network Could Be the Anatomical Basis for Acupoints and Meridians in the Human Body – 2011
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
.
