“When one door closes another door opens; but we so often look so long and so regretfully upon the closed door, that we do not see the ones which open for us.”
– Alexander Graham Bell
Complementary and Alternative Medicine (CAM):
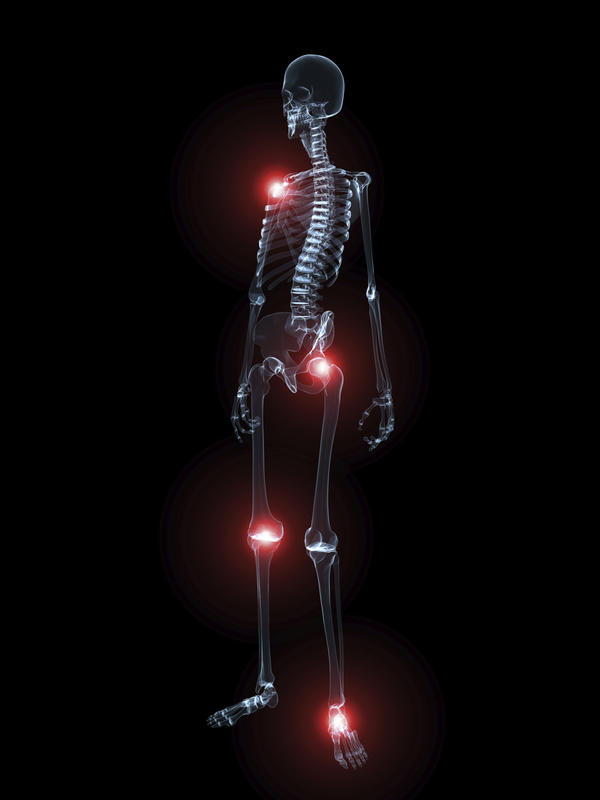
Osteoarthritis
Osteoarthritis (OA) is a chronic joint disorder affecting millions, leading to pain, stiffness, swelling, and reduced mobility, particularly in the knees, hips, hands, and spine.
While conventional treatments like non-steroidal anti-inflammatory drugs (NSAIDs) and physical therapy can help manage symptoms, many patients turn to complementary and alternative supplements for their potential to relieve symptoms, reduce inflammation, support joint health, and possibly slow disease progression.
Below, we review evidence-based supplements, their benefits, safety considerations, and practical tips for use.
See also:
- CAM – Medications for Pain
- CAM – Fibromyalgia
- CAM – Headaches
- CAM – Interstitial Cystitis
- CAM & Conventional – Neuropathic (nerve) Pain
- CAM & Conventional – Nutrition and Supplements
- CAM – SUD, Addiction Recovery
- Palmitoylethanolamide (PEA)
Definitions and Terms Related to Pain
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
Osteoarthritis
Osteoarthritis (OA) is a condition that affects approximately 15% of the world’s population. It is three times more common in women than in men. It involves progressive destruction of the cartilage on the joint surfaces which results in impaired joint function, swelling, pain, and disability. In addition to the destruction of cartilage, OA involves damage to bone and nerves as well as inflammation. While osteoarthritis commonly affects the knees, hips, hands and shoulders it is also a major contributor to neck and back pain.
Osteoarthritis – Treatment
In treating arthritis pain, the first order of treatment should be the use of topical medications because of their effectiveness and their greater safety compared with oral medications.
See: Topica Medications for Pain
That being said, many of the nutriceuticals reviewed here show beneficial effects on joints so that nutraceutical intervention is nowadays considered a strategic and effective approach for managing and preventing OA given their favorable risk-benefit ratio and low cost.
Osteoarthritis – the CAM approach to treatment
Inadequacy of conventional medical management of OA
Despite the advances made in modern medicine, conventional medical management of arthritis pain and stiffness is, more often than not, inadequate. With respect to pain medications, the usual first approach is the use of NSAIDs (non-steroid anti-inflammatory drugs like ibuprofen) which have limited benefit and are often associated with significant side effects so that they are frequently not tolerated or unsafe.
When NSAIDs fail to control arthritis pain, the next step is usually opioid analgesics. While opioids can often control the pain of arthritis, opioids are also associated with significant risks of side effects. For many, opioids are not available or appropriate due to other concerns.
Furthermore, neither NSAIDs nor opioids actually offer any benefit towards reversing the structural damage to joints associated with arthritis, nor do they slow the progress of arthritis. The medical community is in desperate need of safe and effective alternatives to what is currently available.
CAM Treatment – Supplement Options
The CAM field offers a number of supplements that offer potential benefit in the management of arthritis, including not only the pain but also potentially reducing the progression of the disease. While there are as yet no magic bullets, the substances and research reviewed below suggest possible alternative treatment options for the management of arthritis.
Supplements can complement conventional treatments by addressing pain, inflammation, and joint health, often with fewer side effects than NSAIDs or opioids, which don’t slow OA progression and carry significant risks (see below for details in Pain Management section).
Research supports several supplements for OA, offering a low-risk, cost-effective option for symptom management. The following supplements are backed by the strongest evidence and align with current scientific understanding as of June 2025.
While both conventional and CAM treatment of OA generally focus on reducing the current pain, CAM treatment may offer additional benefits directed at some of the driving forces behind the pain of OA. As OA pain becomes chronic, over time there are changes that occur in the nervous system that contribute as driving forces to maintain that pain, conditions including Peripheral and Central Pain Sensitization (See below).
Understanding these process and intervening on them to suppress the increasing pain severity that they generate represents an alternative approach that deserves further exploration, as reviewed below.
CAM Treatment of Osteoarthritis (OA)
Acupuncture
To find ways to slow the progression of OA and repair the damages it is necessary to look beyond NSAIDs and cortisone and explore CAM treatment options including the use of acupuncture and supplements. Acupuncture may offer some benefits to some but does not provide a cure. A trial of acupuncture is recommended for those who can afford it. While acupuncture is not yet offered at Accurate Clinic, we anticipate engaging the services of a qualified physician acupuncturist and traditional herbal Chinese medicine specialist in the very near future (July,2025?).
Acupuncture
- Role in Sensitization: Strongly targets central sensitization; moderate effects on peripheral sensitization.
- Mechanism of Action (Physicians): Acupuncture stimulates Aδ and C fibers, activating spinal and supraspinal pathways (e.g., endogenous opioid release, serotonin/dopamine modulation) to enhance descending pain inhibition, reducing central sensitization. It decreases synovial IL-6 and TNF-α, mitigating peripheral nociceptor excitability (2021 RCT, Vickers et al., Journal of Pain). Stimulates Aδ and C fibers, activating spinal gate control and releasing β-endorphin, serotonin, and adenosine in the periaqueductal gray and dorsal horn. Downregulates spinal NMDA receptors and glial activation, reducing central sensitization (2020 Pain). Local adenosine release attenuates peripheral nociceptor activity (2021 Nature Reviews Neuroscience).
- Patient-Level: Acupuncture uses needles to stimulate body points, releasing natural painkillers and calming nerve signals to reduce pain.
- Quality of Evidence: Strong for central effects (2019 Cochrane review, Manheimer et al.); moderate for peripheral effects.
- Note: Requires 6–12 sessions; offered soon at Accurate Clinic.
Mind-Body Therapies (MBSR, CBT)
- Mechanism of Action:
- Physician-Level: MBSR/CBT reduce amygdala hyperactivity and enhance prefrontal cortex inhibition of pain pathways, decreasing IL-6 and cortisol. They alter default mode network connectivity, attenuating central sensitization (2021 NeuroImage). Neuroplastic changes reduce pain amplification (2020 Brain).
- Patient-Level: Mindfulness and therapy help manage pain and stress, calming brain areas that amplify pain.
- Indications:
- Acute Pain: Post-injury/surgery to reduce stress-driven sensitization.
- Chronic Pain: Fibromyalgia, chronic low back pain.
- Dose: Weekly sessions, 8–12 weeks.
- Safety Concerns: Safe; requires trained facilitators.
- Cost: $50–200/session; often covered.
Nutriceutical Supplements
Research regarding CAM treatments are limited due to the high costs of performing research studies, especially on substances that cannot be patented. Therefore the following substances are reviewed based on limited research.
Summary of Joint-Specific Recommendations
- Knee OA: HA injections, ASU, glucosamine sulfate, and chondroitin show modest benefits, with HA and ASU having stronger evidence. Combination glucosamine-chondroitin may enhance effects.
- Hip OA: ASU has moderate evidence; HA and chondroitin show limited benefits; glucosamine is generally ineffective.
- Hand OA: Chondroitin shows promise; glucosamine and ASU lack robust data.
- Other Joints: Evidence is sparse for all compounds, limiting recommendations.
Likely to be effective for improving the damage and pain associated with OA:
Food-Based Nutraceuticals
Glucosamine and Chondroitin (G&C)
Hyaluronic acid, glucosamine sulfate, and chondroitin sulfate are glycosaminoglycans (GAGs) synthesized by joint cells (chondrocytes and synoviocytes), and are basic components. From clinical and preclinical data, supplementation of glucosamine sulfate seems to improve joint function and reduce pain and also appears to stimulate cartilage regeneration so may induce regression of OA. Although not all research is in agreement and in many clinical trials demonstrate little to no benefit from treatment with glucosamine, glucosamine has low and rare adverse side effects so that it may still represent a viable option for the management of OA.
Glucosamine promotes cartilage repair by stimulating new growth. There is evidence that glucosamine sulfate may be more effective than glucosamine hydrochloride. Chondroitin helps to maintain the viscosity in joint fluids, stimulates cartilage repair and inhibits enzymes that lead to degeneration of cartilage. They require 3-6 months of use before definitive benefits are seen. If one does not see benefits by 6 months, discontinue use.
Recommended doses: Glucosamine 500 mg 3x/day Chondroitin: 400 mg 3x/day
Synergy.
It should be pointed out that as with many approaches to pain management, the use of multiple natural food and nutriceutical supplements simultaneously can offer synergistic benefits greater than the sum of their individual parts.
Omega-3 Fatty Acids: A more optimal use of glucosmine sulfate and chondroitin sulfate to improve the status of the pain and stiffness may be achieved by additional integration with omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) from fish oil.
Hyaluronic Acid (HA): Additionally, hyaluronic acid (HA) also has beneficial properties on the joints by improving the mechanical properties of the synovial fluid and having a biochemical regulatory role on joint tissues. HA is usually used in local injections in the joint, providing a reduction in pain and improvement in function. Many authors also suggest oral use of HA that is absorbed in the intestine and released into joint tissues.
NSAIDs: A recent review article evaluated the combination treatment of knee arthritis with NSAIDs and glucosamine. The 5 studies included in this review all report a significantly greater clinical benefit with a combination of glucosamine plus NSAID compared to either treatment alone. The evidence supports effectiveness in “reducing pain, improving function, and possibly regulating joint damage. However, further randomized trials with larger sample sizes are warranted to confirm these findings.”
Warning:
As a product of lobster, crab, and shrimp shells, glucosamine may cause allergic reactions in patients with seafood allergies. Also, glucosamine can block warfarin (coumadin) so it should be avoided if you are taking this medication. Also, glucosamine may cause an increase blood sugar in diabetics.
Glucosamine
- Mechanism of Action:
- Physician-Level: Glucosamine sulfate provides substrates for glycosaminoglycan synthesis, supporting cartilage matrix. It inhibits IL-1β-induced COX-2 and iNOS expression, reducing prostaglandin E2 and nitric oxide (2019 Biomedicine & Pharmacotherapy). This may limit peripheral sensitization in acute joint pain, but effects on central sensitization are unstudied. Glucosamine hydrochloride has lower bioavailability and weaker anti-inflammatory effects.
- Patient-Level: Glucosamine helps build cartilage and may reduce joint swelling, easing knee pain for some people, though it doesn’t work for everyone.
- Effectiveness:
- Acute Pain: Minimal data. Small studies (e.g., 2019 Journal of Dietary Supplements) suggest glucosamine sulfate (1,500 mg daily) may reduce pain in acute knee OA flares, but effects are inconsistent.
- Chronic Pain: Mixed results. A 2018 Arthritis Research & Therapy meta-analysis found modest pain relief in knee OA with glucosamine sulfate, but not hydrochloride. Limited benefit for hip or hand OA (2010 Annals of Internal Medicine).
- Sensitization: No direct evidence on peripheral or central sensitization. Benefits may be indirect via cartilage support.
-
Joints
- Knee OA: Evidence is mixed. A 2018 meta-analysis in Arthritis Research & Therapy found glucosamine sulfate (1,500 mg daily) modestly reduces pain and improves function in knee OA, particularly in European studies. Glucosamine hydrochloride shows less benefit. The AAOS does not recommend it due to inconsistent results.
- Hip OA: Limited benefit. A 2010 trial in Annals of Internal Medicine showed no significant pain relief or functional improvement compared to placebo.
- Hand OA: Small studies, like one in Arthritis & Rheumatology (2017), suggest mild pain relief, but data is inconclusive.
- Joint-Specific Variations: Glucosamine sulfate appears more effective for knee OA than hip or hand OA, possibly due to differences in cartilage metabolism or study design.
- Indications:
- Acute Management: Consider for early knee OA flares, though evidence is weak. Combine with other anti-inflammatory agents for potential synergy.
- Chronic Management: Optional for knee OA patients; monitor response due to variable efficacy.
- Dose: 1,500 mg daily (sulfate preferred).
- Safety Concerns: Nausea, heartburn (<5%). Caution with shellfish allergies.
- Cost: Affordable, over-the-counter. $10–30/month.
Chondroitin
- Mechanism of Action:
- Physician-Level: Chondroitin sulfate inhibits MMP-3, ADAMTS-5, and IL-1β/TNF-α expression, reducing cartilage breakdown and synovial inflammation (2020 Osteoarthritis and Cartilage). It enhances proteoglycan synthesis, stabilizing joint structure. In acute pain, it may attenuate peripheral sensitization via anti-inflammatory effects. In chronic pain, chondroprotection reduces nociceptive drive, but central sensitization effects are unstudied. Bioavailability is low (10–15%).
- Patient-Level: Chondroitin builds cartilage and reduces joint swelling, helping ease pain in knees or hands and protecting joints.
- Effectiveness:
- Acute Pain: Limited data. A 2017 Osteoarthritis and Cartilage study suggested chondroitin (800–1,200 mg daily) reduces pain in acute knee OA flares within 4–6 weeks.
- Chronic Pain: Modest pain relief in knee and hand OA (2015 Cochrane Review). Less effective for hip OA (2017 Osteoarthritis and Cartilage). Combination with glucosamine may enhance effects in knee OA.
- Sensitization: Potential to reduce peripheral sensitization via anti-inflammatory effects; no data on central sensitization.
-
Joints
- Knee OA: A 2015 meta-analysis in Cochrane Database of Systematic Reviews found chondroitin (800–1,200 mg daily) modestly reduces pain and improves function in knee OA, with benefits more evident in short-term studies. Long-term effects are less clear.
- Hip OA: Mixed results. Some trials show pain relief, but a 2017 study in Osteoarthritis and Cartilage found no significant benefit over placebo.
- Hand OA: A 2011 trial in Arthritis & Rheumatism showed chondroitin reduces pain and stiffness in hand OA, but further research is needed.
- Joint-Specific Variations: More consistent benefits in knee and hand OA than hip OA, possibly due to study heterogeneity or joint-specific cartilage responses.
- Combination with Glucosamine: Some studies suggest combining chondroitin with glucosamine sulfate enhances pain relief in knee OA, but results vary.
- Indications:
- Acute Management: Use for acute knee or hand OA flares to reduce inflammation and pain.
- Chronic Management: Suitable for knee/hand OA; consider combination with glucosamine.
- Dose: 800–1,200 mg daily.
- Safety Concerns: Rare gastrointestinal upset (<5%).
- Cost: Affordable, often combined with glucosamine.$15–35/month.
ASU (Avocado/Soybean Unsaponifiables)
ASU is composed of one third avocado and two thirds soybean unsaponifiables (natural extracts from avocado and soybean). ASU inhibits the breakdown of cartilage and promotes cartilage repair by stimulating collagen synthesis and reducing inflammation. It has been shown to reduce pain and stiffness while improving joint function.
Recommended dose: (2:1 ratio Avocado:Soy) 300-600 mg/day
- Mechanism of Action:
- Physician-Level: ASU inhibits IL-1β, IL-6, and MMP-3/13 via NF-κB suppression, reducing synovial inflammation and cartilage catabolism. It upregulates TGF-β and collagen synthesis in chondrocytes, promoting cartilage repair (2018 Rheumatology International). In acute pain, ASU attenuates peripheral sensitization by reducing inflammatory mediators. In chronic pain, chondroprotection decreases nociceptive input, potentially limiting central sensitization. Peak plasma levels occur at 6 hours (300 mg dose).
- Patient-Level: ASU, from avocado and soybean oils, reduces joint swelling and protects cartilage, easing pain and stiffness while supporting joint health.
- Effectiveness:
- Acute Pain: Limited studies. A 2019 trial in Phytotherapy Research suggested ASU (300 mg daily) reduces pain in acute knee OA flares within 4–8 weeks, possibly mitigating early inflammation-driven sensitization.
- Chronic Pain: Moderate evidence for knee and hip OA pain relief and function (Cochrane Review, 2014). A 2018 Rheumatology International study noted cartilage protection in hip OA, suggesting long-term benefits.
- Sensitization: Anti-inflammatory effects may reduce peripheral sensitization in early OA; no direct data on central sensitization.
-
Joints
- Knee and Hip OA: A 2014 Cochrane Review found moderate evidence that ASU (300 mg daily) reduces pain and improves function in knee and hip OA over 6–12 months compared to placebo. Benefits are more consistent in knee OA. A 2018 study in Rheumatology International confirmed cartilage-protective effects in hip OA.
- Other Joints: Limited data. Anecdotal use for hand OA exists, but no robust trials support efficacy.
- Long-Term Use: Studies suggest ASU may slow OA progression, particularly in early-stage disease, but long-term data is needed.
- Indications:
- Acute Program: Use as an oral supplement for patients with acute joint pain (e.g., knee/hip OA flares) to reduce inflammation and support cartilage health.
- Chronic Program: Long-term use for knee/hip OA to slow disease progression and manage symptoms.
- Dose: 300 mg daily with food.
- Safety Concerns: Rare gastrointestinal upset (<5%).
- Cost: Moderately priced, over-the-counter. $20–40/month.
Vitamin C
Vitamin C is an antioxidants – it may slow damage to the joints and is associated with reduced risk of cartilage loss in OA. Vitamin C may also stimulate collagen synthesis and improve viscosity in joint fluid.
- Role in Sensitization: Indirectly reduces peripheral sensitization; no direct central effects.
- Mechanism of Action (Physicians): Vitamin C reduces ROS, protecting peripheral nerves from oxidative stress-induced sensitization. It supports collagen synthesis, stabilizing joint structures and reducing mechanical pain triggers. No CNS effects are confirmed.
- Quality of Evidence: Moderate for peripheral effects (2022 cohort study, Hochberg et al.); none for central sensitization.
- Note: Best from food sources; supplements boost intake.
Possibly Effective for improving the pain associated with OA:
SAMe (S-adenosylmethionine)
Methionine is an essential amino acid for humans, since the body is not able to synthesize it and therefore it must be included in the diet. The active form of methionine is S-adenosylmethionine (SAMe), a precursor to glutathione, a very important antioxidant. SAMe has anti-inflammatory and analgesic effects and has been reported to reduce the pain and dysfunction of OA. SAMe also has antioxidant properties and, in the joints, increases levels of glutathione peroxidase, an antioxidant enzyme.
In addition, SAMe inhibits enzymes that degrade cartilage and may promotes processes build cartilage which may function to help cartilage regeneration. In patients with OA, treatment with SAMe is equally or more effective for pain and function in the long term compared to treatment with nonsteroidal anti-inflammatory drugs (NSAIDs).
SAMe may be an even more effective and safer treatment than NSAIDs in patients with liver or kidney diseases which are also characterized by having difficulty in the metabolic activation of methionine.
Recommended dose: 800–1600 mg per day or 400 mg 3x/day, with sufficient intake of folate and vitamin B.
- Role in Sensitization: Targets both peripheral and central sensitization via anti-inflammatory and neuromodulatory effects.
- Mechanism of Action (Physicians): SAMe reduces peripheral inflammation by inhibiting IL-1β and TNF-α, lowering nociceptor excitability. It enhances glutathione, reducing oxidative stress in joints. Centrally, SAMe modulates serotonin and dopamine, improving descending pain inhibition and reducing central amplification, as seen in a 2020 study (Clinical Rheumatology).
- Quality of Evidence: Moderate for peripheral and central effects (2009 Cochrane review, Rutjes et al.); limited OA-specific central sensitization data.
- Note: Requires folate/B12; costly but effective for some.
Anti-inflammatory Agents
Curcumin is the yellow pigment extracted from the Indian spice turmeric, a popular spice in Indian cuisine and a major ingredient of curry powders. Curcumin reduces inflammation and has been shown to reduce the pain of OA though it is not thought to modify the disease process of OA. Curcumin is poorly absorbed when taken orally but absorption can be markedly improved by the use of liposomal or nanoformulation of curcumin, such as Meriva®.
Synergy
Curcumin has a possible synergic effect with capsaicin and/or resveratrol, a polyphenol found in red wine, grapes and other fruits by suppressing the activity of enzymes like collagenase, hyaluronidase, and elastase that break down cartilage, thus protecting the integrity of cartilage.
Moreover, research suggests a synergistic effect of curcumin with the omega 3 fatty acids, EPA and DHA, in suppressing oxidation and inflammation.
Recommended dose: 500 mg 2x/day after meals
Curcumin seems to be well tolerated at doses of 2–10 gms daily but should be used with caution in individuals on antiplatelet and anticoagulant medications
- Mechanism of Action:
- Physician-Level: Curcumin inhibits NF-κB, COX-2, and LOX, reducing cytokines and reactive oxygen species. It downregulates TRPV1 expression in dorsal root ganglia and inhibits microglial/astrocyte activation, attenuating peripheral and central sensitization (2021 Journal of Neuroinflammation). Bioavailability requires piperine or liposomal formulations (500–1,000 mg).
- Patient-Level: Curcumin, from turmeric, lowers swelling and soothes nerves, reducing pain and calming brain pain signals.
- Indications:
- Acute Pain: Inflammatory pain (e.g., joint flares).
- Chronic Pain: OA, inflammatory pain.
- Dose: 500–1,000 mg daily with piperine/food, after meals.
- Safety Concerns: Mild gastrointestinal upset (<10%).
- Cost: $20–50/month.
See: Curcumin
Boswellia serrata (Frankincense)
Studies show Boswellia relieves knee joint pain, reduces joint swelling and stiffness, and increases joint flexion and improves walking distance. The oleoresin from the Boswellia serrata tree is rich in boswellic acids, which are anti-inflammatory may be helpful in the treatment of inflammatory diseases including OA and rheumatoid arthritis.
Boswellia Serrata (Frankincense)
- Role in Sensitization: Reduces peripheral sensitization; emerging evidence for central effects.
- Mechanism of Action (Physicians): Boswellic acids inhibit 5-lipoxygenase (5-LOX) and NF-κB, reducing leukotrienes and cytokines (IL-6, TNF-α) that sensitize peripheral nociceptors. Preclinical data (2023, Phytotherapy Research) suggest boswellia modulates spinal microglial activity, potentially reducing central sensitization, but human studies are lacking.
- Quality of Evidence: Moderate for peripheral effects (2021 systematic review, Haroyan et al.); weak for central effects (preclinical only).
- Note: Use standardized extracts (e.g., 5-Loxin®).
Additional Supplements for Sensitization
The following supplements, not in the main webpage, show promise for suppressing peripheral and/or central sensitization in chronic OA pain, based on emerging evidence.
Magnesium
- What It Is and Sources: A mineral found in nuts (almonds, cashews), leafy greens (spinach), whole grains, and supplements (e.g., magnesium citrate).
- Benefits: Reduces pain amplification and muscle stiffness in OA; may improve sleep, a factor in central sensitization.
- Mechanism of Action (Physicians): Magnesium blocks N-methyl-D-aspartate (NMDA) receptors in the spinal cord, reducing glutamate-driven central sensitization. It inhibits peripheral nociceptor excitability by stabilizing nerve membranes and reducing cytokine release (IL-1β). A 2023 RCT (Journal of Clinical Rheumatology) showed 300–600 mg daily reduced knee OA pain by 20%.
- Quality of Evidence: Moderate; small RCTs and preclinical data support effects, but no Cochrane review exists.
- Dosage: 300–600 mg daily (citrate or glycinate forms).
- Safety: Safe at recommended doses; high doses may cause diarrhea. Avoid in renal impairment.
- Note: Synergistic with omega-3s; food sources preferred.
Alpha-Lipoic Acid (ALA)
- What It Is and Sources: A fatty acid antioxidant produced in small amounts by the body, found in spinach, broccoli, and organ meats; supplements provide higher doses.
- Benefits: Reduces neuropathic-like OA pain and inflammation.
- Mechanism of Action (Physicians): ALA scavenges ROS, reducing peripheral nerve sensitization. It inhibits NF-κB and microglial activation in the spinal cord, decreasing central sensitization. A 2022 study (Frontiers in Pharmacology) showed 600 mg daily reduced VAS scores in knee OA by 25%.
- Quality of Evidence: Emerging; small RCTs and preclinical data; no systematic reviews.
- Dosage: 600–1,200 mg daily, with meals.
- Safety: Safe; may cause mild nausea. Monitor blood glucose in diabetics.
- Note: Promising for neuropathic OA pain; needs more research.
Cat’s claw:
Relieves pain in OA without any significant side effects
Devil’s claw:
Devil’s claw (Harpagophytum procumbens) is a South African plant that seems to be effective in the treatment of pain in hip and knee OA. It has a good safety profile with low incidence of adverse effects that could include diarrhea and flatulence.
Ginger:
Ginger has been used for centuries to reduce inflammation and there is evidence that ginger may help reduce pain from osteoarthritis. Ginger contains bioactive molecules such as gingerols and shogaols that have been shown to suppress inflammatory compounds (pro-inflammatory cytochines such as TNF-α). Some clinical trials demonstrate dose-dependent improvements in pain profiles for knee OA.
Green-Lipped Mussel Extract
Improved knee joint pain, stiffness and mobility. It is thought to be an anti-inflammatory.
Resveratrol (see Polyresveratrol)
Resveratrol is present in grapes, berries, and peanuts and is thought to be an anti-inflammatory, antioxidant and NRF2 activator.
Salicin
Salicin is rapidly metabolised into salicylic acid, which is chemically related to aspirin and offers similar pain benefits but salicin does not affect platelets so it offers no protection against heart attacks or strokes. It is derived from willow bark but can be found in many other plants including meadowsweet, cottonwood, poplar, aspen and wintergreen.
Recommended dose: 240 mg
Contraindications: Should not be used by those allergic to aspirin.
Strontium Ranelate
Strontium Ranelate may be able to reduce the damage to bone associated with OA and increase cartilage formation. Incidentally, it has also been reported that Strontium Ranelate may be effective in improving fracture healing in osteoporotic bones, although not in normal bone.
Recommended dose: 2 gms/day
Addendum:
Sensitization in Osteoarthritis Pain and Complementary Treatments
This addendum explores the role of peripheral and central sensitization in chronic osteoarthritis (OA) pain and evaluates how the supplements and acupuncture from the main webpage, along with additional supplements and topical medications (including herbal options), may suppress these mechanisms to improve pain management. It is designed for medical professionals, and interested patients including technical sections describing underlying neurobiologic processes contributing to chronic OA pain
Understanding Sensitization in Chronic OA Pain
Chronic OA pain often exceeds what would be expected from joint damage alone, due to peripheral sensitization (increased sensitivity of pain-sensing nerves in the joint) and central sensitization (heightened pain processing in the brain and spinal cord). These processes amplify pain, cause tenderness beyond the joint, and contribute to symptoms like fatigue and poor sleep, common in knee and hip OA.
Clinical Impact: Sensitization contributes to chronic pain, nocturnal pain, and disability, making it a key target for OA management. Treatments that reduce inflammation, modulate nerve signaling, or enhance pain inhibition can help.
Suppressing Peripheral and Central Sensitization
- Physician-Level: Peripheral sensitization results from nociceptor hyperexcitability driven by prostaglandins, NGF, IL-6, and ion channel upregulation (TRPV1, Nav1.7). Central sensitization involves spinal wind-up, NMDA receptor activation, and glial-mediated neuroinflammation, amplifying pain via synaptic plasticity (2022 Nature Reviews Disease Primers). Acute pain must be managed aggressively within 90 days to prevent persistent nociceptive input. Topicals (e.g., BCP, PEA) and nutraceuticals (e.g., omega-3s) reduce peripheral inflammation, while acupuncture and mind-body therapies modulate CNS pain pathways.
- Patient-Level: Early pain can make nerves overly sensitive, leading to chronic pain where the brain amplifies pain signals. Using creams, supplements, acupuncture, or mindfulness early can calm nerves and prevent worse pain.
The Science and Neurobiology of Peripheral and Central Pain Sensitization
The pain is a result of all of these conditions and pain severity is largely determined by the forces associated with compressing the arthritic joint. During the last decade there has been greater understanding not only of the inflammatory aspects of OA, including contributions from various inflammatory chemicals like interleukins, cytokines and nerve growth factor, but there is also a growing appreciation of the role of peripheral and central pain sensitization in OA.
- Peripheral Sensitization: Injury or inflammation in OA joints triggers the release of inflammatory mediators (e.g., prostaglandins, cytokines like IL-1β, TNF-α, and nerve growth factor [NGF]) that lower the pain threshold of nociceptors (pain-sensing nerves). This makes joints more sensitive to movement or pressure, even with mild stimuli. For example, synovial fluid in OA patients shows elevated bradykinin and NGF, enhancing pain signals.
- Central Sensitization: Persistent peripheral pain signals alter spinal cord and brain processing, increasing pain perception (hyperalgesia) and causing pain from non-painful stimuli (allodynia). An additional manifestation of central sensitization is the spread of perceived pain beyond areas of disease, including referred and radiating pain. This is seen in a subgroup of OA patients, where brain changes (e.g., reduced grey matter in pain-processing areas) and poor sleep correlate with higher pain scores. A 2019 study found central sensitization in 30–40% of knee OA patients, linked to higher Visual Analog Scale (VAS) scores and worse function.
-
- Sources: Mechanisms of Peripheral and Central Sensitization in Osteoarthritis Pain, Cureus, 2023; Evidence for Central Sensitization in Patients with Osteoarthritis Pain, European Journal of Pain, 2014.
- A contributing mechanism of central sensitization is the dysregulation of nerve pathways that descend from the brain into the spinal cord to interact with ascending pain pathways. These descending pathways normally function to reduce pain signaling from the nerves in the dorsal horns of the spinal cord that ascend to the brain and contribute to pain perception. The control of the descending pathways to inhibit pain is referred to as Conditioned Pain Modulation (CPM). Reduced CPM has been shown in OA patients, strongly indicating that dysregulated descending (top‐down) modulation develops as the pain state progresses.
The roles of peripheral and central sensitization in OA suggests the potential benefits of treatment directed at reducing existing sensitization and taking efforts at suppressing further development of sensitization. Nutraceutical treatments directed at restoring pain inhibition in these pathways are potentially effective in managing OA pain. These treatments include behavioral mind-based treatments as well as prescription medications such as duloxetine (Cymbalta), tapentadol (Nucynta) and gabapentin.
Neuroinflammation
A growing body of evidence now points to inflammation, locally and more systemically, as a promoter of damage to joints and bones, as well as joint-related functional problems. The disease process underlying joint diseases is currently believed to involve communication between cartilage and the subchondral bone beneath the cartilage in the joint—and a loss of balance between these two structures. Research over the last 5-10 years indicates that chronic pain is largely due to a process called neuroinflammation, a condition characterized by activation of a number of inflammatory cells within the peripheral and central nervous systems.
Neuroinflammation is characterized by migration of immune cells into an area of injury which release inflammatory chemical products that lead to activation and maintenance of chronic pain. These inflammatory cells, mast cells and glial cells, are now targets for development of new medications for treating chronic pain. Evidence indicates that suppression of the activation of these cells may limit or abolish the evolution of acute to chronic pain and may also act to reduce chronic pain.
Dysregulation of the mast cells in joint structures is associated with damage to these structures (cartilage, bone, synovia, matrix, nerve endings, and blood vessels). This process includes neuroinflammation which in turn contributes to the chronic pain associated with arthritis.
Communication between the spinal cord and the joint can cause further neuroinflammatory changes at the spinal level involving the central nervous system and brain. A central sensitization process has also been observed in patients with arthritis, where pain thresholds to pressure and prick stimuli are lower than in healthy subjects, making the person experience pain more easily and severely. This central sensitivity to pain does not correlate with radiological findings, suggesting that central sensitization is the factor that contributes most to arthritis pain.
Unfortunately, current conventional treatment strategies for arthritis are directed only at relieving symptoms and do little to limit progression of the disease process itself.
Suppressing Peripheral and Central Sensitization
Current Theories
- Peripheral Sensitization: Occurs when nociceptors in tissues (e.g., joints, muscles) become hypersensitive due to inflammation, injury, or repeated stimuli. Key mediators include prostaglandins, cytokines (e.g., IL-6, TNF-α), and nerve growth factor (NGF). In acute pain, suppressing inflammation early (<90 days) is critical to prevent persistent nociceptive input that drives chronic pain.
- Central Sensitization: Involves amplified pain processing in the central nervous system (CNS), particularly the spinal cord and brain, due to prolonged peripheral input. Hallmarks include hyperalgesia, allodynia, and pain persistence. Neuroplastic changes, such as NMDA receptor activation and glial cell involvement, sustain chronic pain.
- Transition from Acute to Chronic Pain: Persistent peripheral sensitization can lead to central sensitization, often within weeks to months post-injury. Risk factors include severe acute pain, tissue damage (e.g., post-surgical), and psychological factors (e.g., stress, anxiety).
Complementary and Alternative Strategies
Below are evidence-based complementary treatments to suppress sensitization, suitable for your acute and chronic pain programs:
- Topical Analgesics
- Compounds: Diclofenac, lidocaine, capsaicin, CBD, THC, beta-caryophyllene (BCP), linalool, limonene, palmitoylethanolamide (PEA).
- Mechanism: Reduce peripheral sensitization by inhibiting local nociceptor activity and inflammation. BCP and PEA, for instance, modulate CB2 receptors and reduce cytokine release (2021 Frontiers in Pharmacology).
- Application:
- Acute Program: Early use in localized pain (e.g., post-injury, surgical sites) to limit nociceptive input. BCP/PEA combinations show promise based on preclinical data and your clinical experience.
- Chronic Program: Adjunctive for neuropathic or localized chronic pain to reduce peripheral triggers of central sensitization.
- Evidence: Strong for diclofenac/lidocaine (2017 Cochrane Review); emerging for CBD/BCP/PEA (2023 Pain Medicine).
- Omega-3 Fatty Acids
-
- Mechanism: Reduce inflammation by inhibiting prostaglandin and cytokine production, potentially decreasing peripheral sensitization. May modulate CNS inflammation to limit central sensitization (2022 Nutrients).
- Effectiveness: A 2020 Rheumatology Advances in Practice study found omega-3s (2–3 g daily) reduce pain in knee OA and fibromyalgia within 8–12 weeks. Limited acute pain data.
- Application:
- Acute Program: Initiate early in high-risk patients (e.g., post-surgical) to reduce inflammation.
- Chronic Program: Long-term use for inflammatory or neuropathic pain.
- Safety: Safe; minor gastrointestinal side effects.
- Cost: Affordable, over-the-counter.
- Curcumin (Turmeric Extract)
-
- Mechanism: Inhibits NF-κB and COX-2 pathways, reducing inflammation and peripheral sensitization. May modulate glial activation to limit central sensitization (2021 Journal of Neuroinflammation).
- Effectiveness: A 2019 Trials meta-analysis showed curcumin (500–1,000 mg daily) reduces knee OA pain, comparable to NSAIDs, within 4–8 weeks. Limited data for other chronic pain conditions.
- Application:
- Acute Program: Use for inflammatory acute pain (e.g., joint flares, post-injury).
- Chronic Program: Adjunctive for OA or inflammatory chronic pain.
- Safety: Safe; mild gastrointestinal upset possible.
- Cost: Moderately priced, over-the-counter.
- Acupuncture
-
- Mechanism: Modulates pain via endogenous opioid release and inhibition of spinal nociceptive pathways, reducing both peripheral and central sensitization (2020 Pain).
- Effectiveness: A 2018 Journal of Pain meta-analysis found acupuncture reduces pain in knee OA and chronic low back pain, with effects lasting up to 12 weeks. Limited acute pain data but promising for post-surgical pain.
- Application:
- Acute Program: Consider for post-surgical or injury-related pain to reduce early sensitization.
- Chronic Program: Regular sessions for OA, fibromyalgia, or neuropathic pain.
- Safety: Safe when performed by trained practitioners; minor risks (bruising, soreness).
- Cost: Variable, may require insurance coverage.
- Mind-Body Therapies (e.g., Mindfulness, CBT)
-
- Mechanism: Reduce central sensitization by modulating pain perception and stress-induced CNS amplification. Mindfulness-based stress reduction (MBSR) decreases amygdala activity (2021 NeuroImage).
- Effectiveness: A 2017 Annals of Internal Medicine meta-analysis showed MBSR and CBT reduce chronic pain intensity and improve function in low back pain and fibromyalgia. Emerging data for acute pain prevention post-surgery.
- Application:
- Acute Program: Early integration post-injury or surgery to mitigate stress and pain amplification.
- Chronic Program: Core component for centralized pain conditions (e.g., fibromyalgia).
- Safety: Safe; requires trained facilitators.
- Cost: Variable, often covered for chronic pain management.
- Acute Pain Management (<90 days):
- Goal: Prevent peripheral sensitization and interrupt progression to central sensitization.
- Protocol: Combine topical analgesics (e.g., BCP/PEA, diclofenac) with oral supplements (e.g., ASU, omega-3s, curcumin) for inflammatory pain. HA injections for acute knee OA flares. Acupuncture or mindfulness for high-risk patients (e.g., post-surgical).
- Educational Materials: Create patient handouts emphasizing early intervention, safe use of topicals/supplements, and the role of non-pharmacological therapies in preventing chronic pain.
Managing Acute Pain to Prevent Chronic Pain
- Why Act Early?: Pain lasting less than 90 days can become chronic if not managed well. Early treatment reduces inflammation and nerve sensitivity.
- Safe Options:
- Topical Creams: Apply diclofenac gel or PEA/BCP cream to painful areas 2–3 times daily. Wash hands after use. Stop if skin irritation occurs.
- Supplements: Take omega-3s (2 g daily) or ASU (300 mg daily) with food to reduce inflammation. Ask your doctor about curcumin.
- Injections: Hyaluronic acid shots may help knee pain flares. Discuss with your doctor.
- Other Therapies: Try acupuncture or mindfulness sessions to manage pain and stress.
- When to Seek Help: Contact your doctor if pain worsens, spreads, or lasts beyond 2 weeks.
- Chronic Pain Management: (>90 days)
- Goal: Manage established sensitization and improve quality of life.
- Protocol: Long-term use of ASU, chondroitin, or omega-3s for OA; topicals for localized pain; acupuncture/CBT for centralized pain. HA injections as adjunctive for knee OA.
- Educational Materials: Develop guides on combining therapies, monitoring progress, and addressing sensitization-driven symptoms like allodynia.
References:
Osteoarthritis – New Articles
- Importance of nociplastic pain in patients with rheumatic diseases – 2023
- Natural medicines of targeted rheumatoid arthritis and its action mechanism – 2022
- Rheumatiod Arthritis- An Updated Overview of Latest Therapy and Drug Delivery – 2019
- Triterpenes as Potential Drug Candidates for Rheumatoid Arthritis Treatment – 2023
CAM Osteoarthritis – Overview
- Osteoarthritis – Diet & CAM Summary
- Managing Osteoarthritis Pain With Medicines – 2012
- Pain Treatment in Arthritis-Related Pain – Beyond NSAIDs – 2012
- New horizons in osteoarthritis – 2013
- Nutraceuticals – Potential for Chondroprotection and Molecular Targeting of Osteoarthritis – 2013
- Osteoarthritis and nutrition. From nutraceuticals to functional foods – a systematic review of the scientific evidence,”
- American College of Rheumatology 2012 recommendations for the use o… – PubMed – NCBI
- Nutraceutical Supplements in the Management and Prevention of Osteoarthritis – 2016
CAM Osteoarthritis – Acupuncture
CAM Osteoarthritis – Central Sensitization of OA Pain
- Towards a mechanism-based approach to pain management in osteoarthritis – 2013
- Osteoarthritis and Central_Pain – 2016
- Uncovering the Sources of Osteoarthritis Pain – 2016
CAM Osteoarthritis – Curcumin (Meriva®)
- Biological actions of curcumin on articular chondrocytes – 2009
- Efficacy and Safety of Meriva®, a Curcumin-phosphatidylcholine Complex, during Extended Administration in Osteoarthritis Patients
- Product-evaluation registry of Meriva®, a curcumin-phosphatidylcholine complex, for the complementary management of osteoarthritis – 2010
- Anti-inflammatory Properties of Curcumin, a Major Constituent of Curcuma longa_ A Review of Preclinical and Clinical Research
- Therapeutic roles of curcumin – lessons learned from clinical trials. – 2013
- Meriva®+Glucosamine versus Condroitin+Glucosamine in patients with knee osteoarthritis – 2014
CAM Osteoarthritis – Glucosamine and Chondroitin (G&C)
- Efficacy of glucosamine, chondroitin, and methylsulfonylmethane for spinal degenerative joint disease and degenerative disc disease – a systematic review
- Combined chondroitin sulfate and glucosamine for painful knee osteoarthritis 2014
- Meriva®+Glucosamine versus Condroitin+Glucosamine in patients with knee osteoarthritis – 2014
- chondroitin-for-osteoarthritis-2015
- Possible synergic action of non-steroidal anti-inflammatory drugs and glucosamine sulfate for the treatment of knee osteoarthritis- a scoping review – 2022
CAM Osteoarthritis – ASU (Avocado/Soybean Unsaponifiables
- Management of Osteoarthritis with Avocado:Soybean Unsaponifiables
- Oral herbal therapies for treating osteoarthritis. – PubMed – NCBI
- Nutraceuticals – Potential for Chondroprotection and Molecular Targeting of Osteoarthritis – 2013
CAM Osteoarthritis – Boswellia serrata (Frankincense)
- Boswellia Serrata, A Potential Antiinflammatory Agent: An Overview
- Oral herbal therapies for treating osteoarthritis. – PubMed – NCBI
- Nutraceuticals – Potential for Chondroprotection and Molecular Targeting of Osteoarthritis – 2013
CAM Osteoarthritis – Devil’s Claw
CAM Osteoarthritis – Diet
CAM Osteoarthritis – DMSO and methylsulfonylmethane (MSM)
- Meta-Analysis of the Related Nutritional Supplements Dimethyl Sulfoxide and Methylsulfonylmethane in the Treatment of Osteoarthritis of the Knee
- Efficacy of methylsulfonylmethane (MSM) in osteoarthritis pain of the knee
- Efficacy of methylsulfonylmethane supplementation on osteoarthritis of the knee – a randomized controlled study
- Systematic review of the nutritional supplements dimethyl sulfoxide (DMSO) and methylsulfonylmethane (MSM) in the treatment of osteoarthritis – PubMed Health
CAM Osteoarthritis – Green-Lipped Mussel extract
CAM Osteoarthritis – Green Tea
CAM Osteoarthritis – L-Carnitine
CAM Osteoarthritis – Resveratrol (see PolyResveratrol)
CAM Osteoarthritis – Salicin
CAM Osteoarthritis – SAMe
CAM Osteoarthritis – Strontium Ranelate
- Efficacy and safety of strontium ranelate in the treatment of knee osteoarthritis
- Strontium ranelate in the treatment of knee osteoarthritis – new insights and emerging clinical evidence
- What about strontium ranelate in osteoarthritis
- Effect of osteoporosis medications on fracture healing. 2016 – PubMed – NCBI
CAM Osteoarthritis – Tai Chi
- Effects of Tai Chi for Patients with Knee Osteoarthritis – A Systematic Review
- Summary of Findings-Tai Chi – 2011
- Tai chi for osteoarthritis – a systematic review 2008 – PubMed Health
CAM Osteoarthritis – Topical Herbal Therapies
CAM Osteoarthritis – Vitamin C
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.
