Topical Medications for Pain

“Foolish is the doctor who despises the knowledge acquired by the ancients.” — Hippocrates
Topically applied medications are important treatment options for those with both acute and chronic pain. The world of topical pain medications is complex and can be daunting for the uninformed, especially when selecting an over-the-counter (OTC) product. This section provides the information needed to make informed decisions regarding OTC products as well as providing insight as to prescription medications recommended by a clinician.
Link to videos on this topic on Dr. Ehlenberger’s Youtube channel:
Links to other Pertinent Educational Pages:
Commercial Topical Medications Products:
- LA Marijuana Products – Topicals
- CBD/BCP from AliceCBD.com
- Soothe from TullaBotanicals..com
See also:
The medical information on this site is provided as a resource for information only, and is not to be used or relied upon for any diagnostic or treatment purposes and is not intended to create any patient-physician relationship. Readers are advised to seek professional guidance regarding the diagnosis and treatment of their medical concerns.
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
Links to topical medications by condition:
Links to individual topical medications:
- Amitriptyline
- Arnica
- Baclofen
- Camphor
- Capsaicin
- CBD/BCP
- BCP/PEA (“Soothe”)
- Chinese Topical Medications
- Compounded Medications
- Diclofenac
- Doxepin
- Frankincense
- Gabapentin
- Ketamine
- Lidocaine
- Menthol
- Naproxen
- PEA (palmitoylethanolamide)
- Salicylates (Trolamine and Methyl Salicylate)
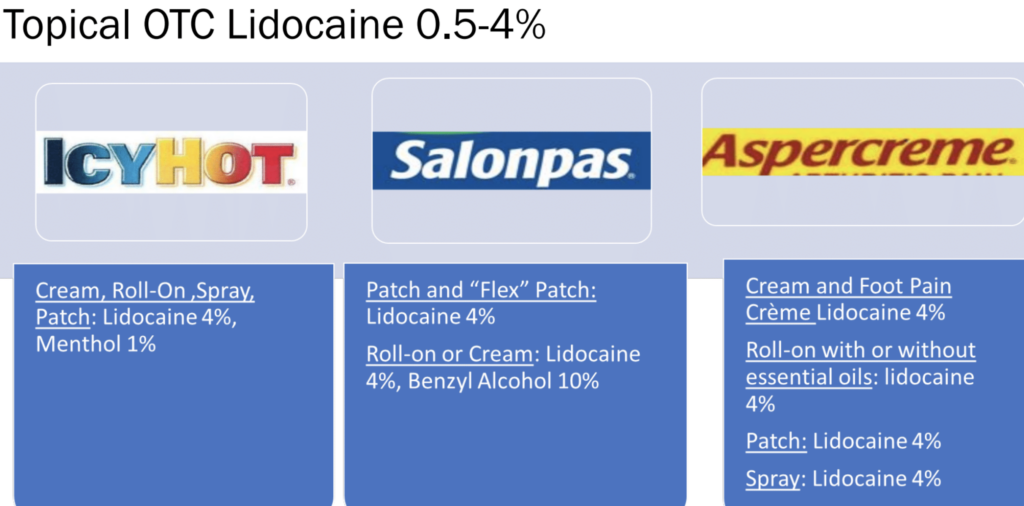
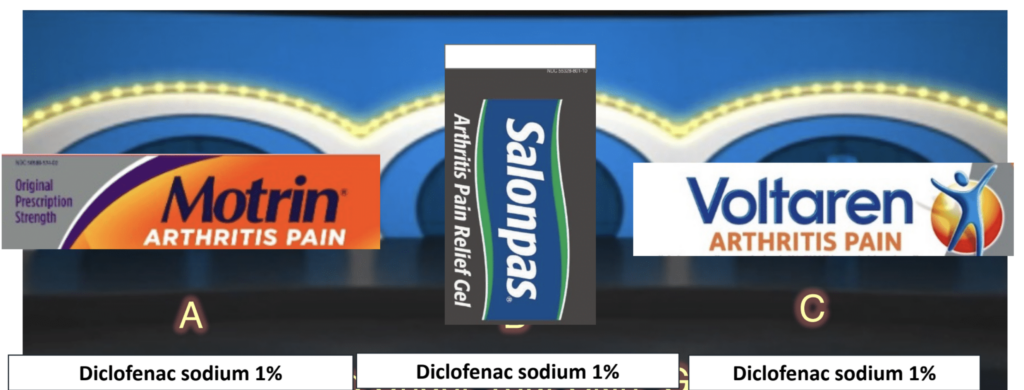
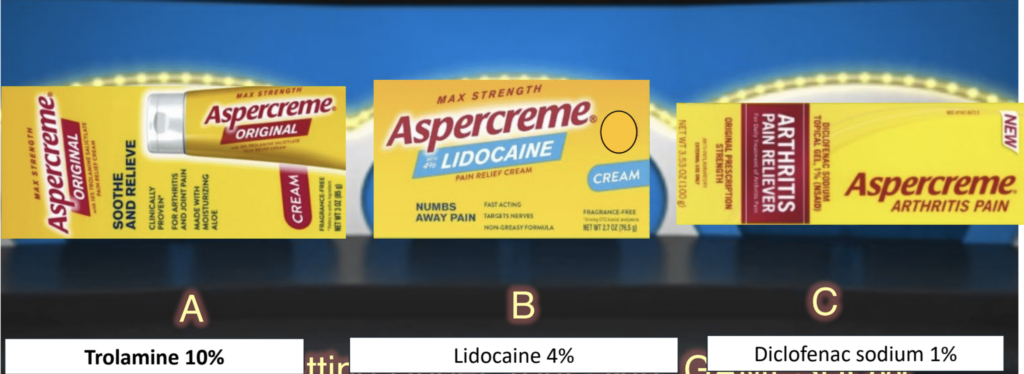
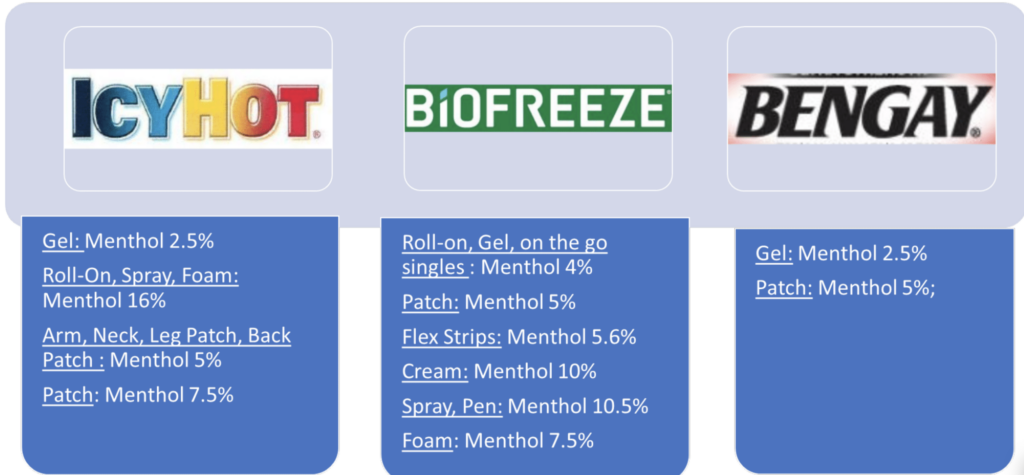
OTC Watch: Always review the ingredients in topical medications. Many, if not most, of the well-known brand name topical medications have multiple products that each may have different ingredients where some may contain lidocaine, diclofenac, salicylates, menthol and camphor. Some products may also include additional ingredients such as herbal extracts.
Topically Applied Medications
To begin, medications designed to be applied topically to the skin for therapeutic purposes are generally referred to as “topicals.” Technically, however, topically applied medications may be either “transdermal” or “topical.” The distinction is quite important and determines the therapeutic impact of the product. This web section focuses only on topical medications for pain.
Transdermal vs Topical
Transdermalmedications are designed to penetrate the skin barrier in order to enter the blood and provide systemic (whole body) benefits. By penetrating through the epidermis, the topmost layers of the skin, and into the underlying dermis layer where the blood vessels are, transdermal products enter the blood vessels and are then transported through the blood to the organs, including the central nervous system (spinal cord and brain) to provide therapeutic benefits.
Topicalformulations, on the other hand, refers to creams, lotions, ointments, and other products designed to be applied to the skin (epidermis) to permeate (travel) through the skin to act regionally (e.g., for the treatment of muscle or join pain) for local therapeutic benefits only. They are not formulated to transport medications into the blood vessels of the subcutaeous dermal layer below and therefore are not meant to enter systemic circulation for the treatment of symptoms at sites a distance away.
Due to the wide variety of medical conditions associated with pain, the selection of an appropriated topical pain medication requires an understanding of the underlying mechanism(s) underlying both the pain and the medications potentially available to treat that pain.
Topically Applied vs Orally Ingested Medications
An important point to emphasize is that some medications, notably diclofenac, achieve significantly higher levels in muscle and joint (synovial) tissue when applied topically vs when taken orally. This suggests that a topical medication is likely to work better than an oral version although studies identify a similar pain response. Furthermore, because blood (serum) levels are much lower (@1%) than with topical medications, there is far less toxicity and side effects, especially gastrointestinal, when medications are applied topically. This is particularly of value with the NSAIDs class of medications.
In a 2010 study, systemic bioavailability and pharmacodynamics of topical diclofenac sodium gel 1% were compared with those of oral diclofenac sodium 50-mg tablets. In a randomized, 3-way crossover study, 40 healthy volunteers received three 7-day diclofenac regimens:
- 16 g gel applied as 4 g to 1 knee 4 times daily (4 g on surface area 400 cm(2)),
- 48 g gel applied as 4 g per knee 4 times daily to 2 knees plus 2 g gel per hand applied 4 times daily to 2 hands (12 g on 1200 cm(2)), and
- 150 mg oral diclofenac applied as 50-mg tablets 3 times daily.
Results:
-
- Systemic exposure was greater with oral diclofenac (AUC(0-24), 3890 +/- 1710 ng x h/mL) than with topical treatments A (AUC(0-24), 233 +/- 128 ng x h/mL) and B (AUC(0-24), 807 +/- 478 ng x h/mL).
- Oral diclofenac inhibited platelet aggregation, cyclooxygenase-1 (COX-1), and COX-2.
- Topical diclofenac did not inhibit platelet aggregation and inhibited COX-1 and COX-2 less than oral diclofenac.
- Treatment-related adverse events were mild and limited to application site reactions with diclofenac sodium gel 1% (n = 4) and gastrointestinal reactions with oral diclofenac (n = 3).
- Systemic exposure with diclofenac sodium gel 1% was 5- to 17-fold lower than with oral diclofenac.
- Systemic effects with topical diclofenac were less pronounced.
Where to Start?
For those simply looking for where to start, this section will guide you.
For more in-depth exploration of individual medications and their indications, move forward to the next section below and explore Topical Medications for Pain – Synergy
In general, start with inexpensive but effective topical medications first. Since insurance often pays for only the prescription topicals lidocaine and diclofenac, one should start with either lidocaine or diclofenac first to determine their individual benefits then try the two together to determined their combined benefit.
It should be noted that simultaneous use of a topical menthol product such as Biofreeze or Icy Hot can enhance the absorption of the diclofenac resulting in greater pain benefits although possible greater local. skin side effects.
Unfortunately, the other prescription topical medications effective for pain are not usually covered by insurance and are relatively expensive, so the next less-expensive topicals to add are OTC products with CBD, BCP and/or PEA. There are tw0 products providing a different two of these three:
- CBD/BCP (AliceCBD.com): This combination adds both CBD and BCP
- Soothe” (BCP/PEA) (TullaBotanicals.com): This combination adds both BCP and PEA
After adding one of these products and determining its benefit, try the other to determinne its benefit and onsider implementing the better of the two into your regimen. The next step if desired is to identify and add. the the missing element, either CBD or PEA depending on the product you preferred.
Following this regiment you may find the combination of lidocaine, diclofenac and BCP along with PEA and/or CBD to be your best. But if you wish to explore further, the next steps would include exploring diffferent prescription medications that can be compounded by a special compounding pharmacy. Sometmes compounded medications can be covered by insurance. The following compounded medications should be considered, especially for neuropathic pain such as peripheral neuropathies:
- Gabapentin
- Ketamine
- Amitriptyline
- Clonidine
Additional alternative topical medications offering potential pain benefits are reviewed below.
1. Acute & Chronic Muscle Pain (sore muscles and trigger points), Sprains and Tendonitis
Acute muscle pain may arise from tissue damage from trauma or overuse and may include an inflammatory component. Therefore a topical medication with anti-inflammatory properties and analgesic benefits would be recommended. However, a neuropathic pain component should be anticipated as well when circumstances suggest the tissue pain potentially to be transitioning from acute to chronic pain (>>3 months) or it has already transitioned as in the case with trigger points. This transition is driven by neuro-inflammation and oxidative stress and therefore topical medications to suppress the development of neuro-inflammation would be advised. Such topicals should include anti-inflammatory, antioxidant and neuropathic agents.
The following topical medications are recommended for muscle, sprain and tendonitis pain:
- Diclofenac gel 1% (OTC or Rx); or 3%) (Rx)
- Topical CBD, BCP and/or THC cream (OTC/Rx) including combination CBD/BCP and BCP/PEA)
- Lidocaine: cream (OTC or Rx) or
- Lidocaine: patches (OTC; Lidoderm 5% or ZTLido patches (Rx)
- Topical Palmitoylethanolamide PEA (OTC)
- Topical Baclofen 6% (Rx/Compounded)
- Topical Gabapentin 6% (Rx/Compounded)
- Menthol (OTC: products such as Biofreeze)
- Magnesium (creams and/or Epsom salt baths)
Priority of choice is largely dependent on financial considerations and insurance coverage. Since the mechanisms of action of each of these medications are all different, they can be used simultaneously on the same day but not necessarily applied together.
2. Arthritis (Degenerative or Osteoarthrits and Rheumatoid Arthritis)
Osteoarthritis & Bursitis
The term arthritis is typically applied to osteoarthritis or degenerative arthritis, the arthritis associated mostly with aging. It is a condition that does have an inflammatory component, but also has a significant neuropathic component (nerve pain). Therefore topical medications directed at inflammation as well as those directed at nerve pain would be expected to benefit someone with osteoarthritis. Bursitis is an inflammatory condition involving joint structures called bursa. A bursa is a closed, fluid-filled sac located next to tendons near large joints and functions as a cushion and gliding surface. Bursitis would be expected to respond to the same topical medications as arthritis with emphasis on the NSAIDs.
The following topical medications are recommended for osteoarthritis and bursitis pain:
- Topical Diclofenac gel 1% (OTC or Rx); or 3%) (Rx)
- Topical CBD, BCP and/or THC cream (OTC/Rx) including combinations CBD/BCP and BCP/PEA)
- Topical Lidocaine cream (OTC or Rx),
- Lidoderm 4% patches (OTC), 5% patches(Rx) or ZTLido patches (Rx)
- Topical palmitoylethanolamide PEA (OTC)
- Topical Gabapentin 6% (Compounded)
Rheumatoid Arthritis
In the case of rheumatoid arthritis and other immune related, arthritis is such as those associated with psoriasis or lupus, there is a dominant component of inflammation, underlying the disease process, and therefore these conditions would benefit most from anti-inflammatory topical medication (NSAID or steroid). The strongest anti-inflammatory, topical medication’s are steroids, such as dexamethasone and Cortisone. However, steroid medication’s have the potential for toxicity or detrimental effects, so treatment with topical steroids should generally be prescribed by rheumatologists or other physicians with specific expertise to avoid complications.
The following topicals are recommended for rheumatoid arthritis pain:
- Diclofenac gel 1% (OTC or Rx); or 3%) (Rx)
- Topical CBD, BCP and/or THC cream (OTC/Rx) including combinations CBD/BCP and BCP/PEA)
- Topical Lidocaine: cream (OTC and/or Rx) or patches (OTC; Lidoderm 5% or ZTLido patches (Rx)
- Topical PEA (palmitoylethanolamide) cream (OTC)
- Topical Compounded Gabapentin 6%
- Corticosteroids as advised by a rheumatologist
Priority of choice is largely dependent on financial considerations and insurance coverage. Since the mechanisms of action of each of these medications is different, they can be used simultaneously on the same day but not necessarily applied together.
3. Neuropathic Pain – Neuropathy, Fibromyalgia, Carpal Tunnel Syndrome
Neuropathic pain may be a significant component of various conditions, not typically thought of as based on pathology of the nervous system, such as arthritis, headaches, and visceral pain, it is the dominant contributor to the pain associated with conditions, such as diabetic peripheral neuropathy, chemotherapy induced neuropathy, post-herpetic neuropathy,and various polyneuropathies and mononeuropathies related to peripheral nerve compression syndrome, such as carpal tunnel syndrome. Also included in pain conditions based in neuropathic pain are fibromyalgia and chronic regional pain syndrome amongst others. For the most part, these conditions have not demonstrated significant benefit from the application of topical NSAID medications.
The following topical medications are recommended for neuropathic pain:
- Topical Lidocaine: cream (OTC or Rx) or patches (OTC; Lidoderm 5% or ZTLido patches (Rx)
- Topical CBD, BCP and/or THC cream (OTC/Rx) including combinations CBD/BCP and BCP/PEA)
- Topical Gabapentin 6% (Compounded)
- Topical PEA (palmitoylethanolamide) cream (OTC)
- Topical Baclofen 6% (Compounded)
- Capsaicin 8% patches (Rx)
Priority of choice is largely dependent on financial considerations and insurance coverage. Since the mechanisms of action of each of these medications is different, they can be used simultaneously on the same day but not necessarily applied together.
Recommended Topical Medications
Cannabidiol (CBD)
Cannabidiol (CBD)is a cannabinoid found in marijuana and hemp plants which has shown anti-inflammatory and pain benefits when applied topically. CBD may be used effectively as a topical salve for pain, including arthritis pain, pain due to peripheral neuropathy and muscle pain related to spasm.
Peripheral Neuropathy
There has been an increasing evidence for the benefits of cannabinoids in the treatment of chronic, neuropathic pain. A 2020 study evaluated the effectiveness of topical cannabidiol (CBD) oil in the management of neuropathic pain associated with peripheral neuropathy. The 29 test subjects with a mean age of 68 year had at least one of the following underlying conditions that caused the peripheral neuropathy: type 1 or type 2 diabetes, alcoholic neuropathy, idiopathic neuropathy, congenital hypomyelinating neuropathy or neuropathy as a result of syphilis or leprosy. Subjects were studied in a four-week, randomized crossover and placebo-controlled trial with treatment including the use of a product containing 250 mg CBD/3 fl. oz.
Results showed a statistically significant reduction in intensity of pain, cold and itchy sensations in the CBD group when compared to the placebo group. The treatment product was well tolerated with no adverse events reported.
For further information regarding CBD, see: CBD and Topical Marijuana Products
Effectiveness
A treatment course of 4 weeks of CBD cream (250 mg/3 oz) applied up to 4 times daily has been shown to be effective for neuropathic pain, with improvement in pain intensity
Dermal penetration/bioavailability:
Penetration of CBD through the skin is poor so penetration enhancers are needed such as shea butter.
Mechanism of Action
CBD does not directly act on cannabinoid-receptor (CB) 1 or 2•Potential CBD targets in the skin••CBD products available outside a dispensary are hemp-derived (THC content <0.3%) •Some evidence that online and retail products are inaccurately labeled.
Beta-Caryophyllene (BCP)
Beta-Caryophyllene (BCP) is a terpene found in marijuana as well as many other plants including black pepper, hops, cinnamon and cloves. BCP has powerful analgesic anti-inflammatory benefits with topical use (as well as oral use.)
For further in-depth information regarding BCP, see: Beta-Caryophyllene (BCP)
Effectiveness
BCP has demonstrated potent benefit for muscle pain including myofascial trigger points, joint pain in osteoarthritis and rheumatoid arthritis and neuropathic pain associated with diabetic and chemotherapy-induced peripheral neuropathy, plantar fasciitis and CRPS. It has also demonstrated benefits in wound healing.
Dermal penetration/bioavailability:
Penetration of BCP through the skin is poor so penetration enhancers are needed such as shea butter.
Mechanism of Action
BCP is believed to have many mechanisms of action which allows it to provide therapeutic benefits for many diverse conditions. It acts directly as an agonist of the CB2 cannabinoid-receptor and as such is considered to be a cannabinoid as well as a terpene. This action supports anti-inflammation and pain reduction. It also acts as an antagonist of the Transient Receptor Potential Melastatin 8 (TRPM8), a cation channel found on both Aδ and C fiber nerve fibers that signal pain and cold sensation peripherally to the spinal cord.
This blocking of the TRPM8 is thought to contribute not only to its benefit for nerve pain in fibromyalgia and neuropathy but it may also reduce the sensitivity to cold pain experienced by so many individuals with chronic pain associated with many conditions.
BCP can be found as a stand-alone topical agent but is best used in combination with either CBD (AliceCBD) or PEA Tulla Botanicals (see below).
Topical PEA (Palmitoylethanolamide) (OTC)
Palmitoylethanolamide (PEA) is an endogenous (manufactured by the body) fatty acid amide which is emerging as a new agent in the treatment of pain and inflammation, particularly nerve pain. It is found in foods such as milk and eggs and is completely safe with no side effects. PEAt works in synergy with other pain medications including baclofen and CBD (see Synergy between CBD and PEA).
Topical PEA is recommended for:
- Arthritis – osteoarthritis & rheumatoid athritis
- Fibromyalgia
- Peripheral neuropathies – diabetic neuropathy & chemotherapy-induced peripheral neuropathy
- Carpal tunnel syndrome
- Low back pain – herniated disc disease, failed back surgery syndrome, other
- Neuropathic pain – related to multiple sclerosis
There are currently, multiple OTC topical PEA products available on the internet. Unfortunately, no clinical trials have been performed to compare the effectiveness of one versus another. PEA topical cream is available in 2% strength, with recommended application 4x/day as needed.
See: Vitalitus – Soothamide (Palmitoylethanolamide 2% Topical Cream), 100 ml. Additional ingredients include: immondsia chinensis (Jojoba) Oil, Vitellaria paradoxa (Shea) Butter, Aloe Vera, Palmitoylethanolamide, Boswellia serrata (Indian Frankincense) Resin, Commiphora myrrha (Myrrh).
For more information about PEA, see: Palmitoylethanolamide (PEA)
CBD/BCP (OTC from AliceCBD.com)
While cannabidiol, CBD, has both anti-inflammatory and pain properties. It has been shown to work in synergy with BCP to provide pain relief for inflammatory pain conditions as well as neuropathic pain conditions. In addition to the CBD and BCP, this product also contains lavender and frankincense oils that provide fragrance but also may have therapeutic properties as well. Lavender has anti-inflammatory properties while frankincence may prevent the production of inflammatory substances in joints. Current evidence, suggests they may have beneficial effects with osteoarthritis.
Topical CBD/BCP is recommended for:
- Acute & Chronic Muscle Pain (sore muscles and trigger points, Sprains and Tendonitis)
- Arthritis (joints) & Bursitis
- Neuropathic Pain (diabetic, Ehler-Danlos, Multiple Sclerosis, post-radiation, polyneuropathy, Fibromyalgia)
- Plantar Fasciitis
Currently, only one OTC topical product is known to be available that contains CBD and BCP (cannabidiol and beta caryophylline), CBD/BCP from AliceCBD.com. A few years ago another similar product with CBD & BCP was available from Entourage that was quite effective for many pain conditions. Over 100 Accurate Clinic patients found it be helpful with 9/10 patients choosing to continue using it. Unfortunately, this product is no longer available. However, the AliceCBD version is quite similar, sharing the inclusion of CBD, BCP, lavender oil and shea butter.
Topical CBD/BCP appears to be very helpful for muscle and joint pain, including arthritis and painful myofascial trigger points commonly accompanying neck and back pain associated with disc problems and arthritis of the spine. Experience has also identified this topical to likely help with painful neuropathy associated with diabetes, chemo- and radiation therapy and polyneuropathy of uncertain etiologies.
CBD has been shown to work in synergy with palmitoylethanolamide (PEA) in studies of oral use, suggesting this benefit may also extend to topical use of these compounds together (see below).
For more information, see CBD, CBD Synergy with PEA, Topical Marijuana, and BCP.
Link: CBD/BCP from AliceCBD.com.
BCP/PEA (“Soothe”) – TullaBotanicals.com
“Soothe” is a topical medication that combines 3.75% Beta-Caryophyllene (BCP) and 1% Palmitoylethanolamide (PEA), thereby offering the benefits provided by these two constituents. BCP is a powerful analgesic with anti-inflammatory benefits and PEA is also good for inflammation and pain, particularly nerve pain.
- For further in-depth information regarding BCP, see: Beta-Caryophyllene (BCP)
- For further in-depth information regarding PEA, see: Palmitoylethanolamide (PEA)
- For further in-depth information regarding “Soothe”, see: “Soothe” or: TullaBotanicals.com
OTC Watch: Always review the ingredients in topical medications. Many, if not most, of the well-known brand name topical medications have multiple products that each may have different ingredients where some may contain lidocaine, diclofenac, salicylates, menthol and camphor. Some products may also include additional ingredients such as herbal extracts.
Topical Lidocaine
Topical lidocaine is available in creams gels and patches. It is also available over the counter in strength up to 4% and buy prescription patches up to 5%. Prescription lidocaine is generally well covered by insurance and probably provides superior benefit to over-the-counter products. Of note, the brand ZTLido patches while only labelled as 1.8% are equally effective as the Lidoderm 5% patches. Further, does ZTLido patches seem to adhere better to the skin than the 5% lidoderm patches.
Effectiveness:
Evidence confirms effectiveness of topical lidocaine gel (5 percent) to treat pain when applied to intact skin. Topica lidocaine is FDA approved for treating neuropathic pain after herpes zoster infection (postherpetic neuralgia). It is considered effective for many conditions associated with neuropathic pain.
Dermal penetration/bioavailability:
There is limited evidence on the dermal penetration and bioavailability of topical lidocaine gel (5 percent). Although as a reference, the absorption of lidocaine from a lidocaine patch (5 percent) is minimal (less than 3 percent). Modifications to the ingredient or excipient may increase aqueous solubility and increase absorption.
Safety and adverse effects:
Topical lidocaine gel is safe in strengths up to (5%). With the topical application of Lidoderm (lidocaine patch (5%), the systemic exposure of lidocaine is minimal. However, when recommended doses are exceeded resulting in extensive systemic absorption, there is potential for adverse effects including precipitating CNS disturbances, such as psychosis and seizures .
Mechanism of Action
Lidocaine is a nonselective, voltage-gated sodium channel inhibitor, affecting both the generation and conduction of nerve impulses. It stabilizes nerve membranes, reducing ectopic activity in damaged afferent pain receptors. Other effects on skin cells (keratinocytes) and immune cells, or activation of irritant receptors (TRPV1 and TRPA1), may also contribute to the analgesic effect of topical lidocaine.
Brand names of different formulations of lidocaine include:Icy Hot, Salon Pas, Bengay, Two Old Goats – Arthritis, Sore No More, and Aspercreme.

Topical Diclofenac (OTC & Rx)
As with the case of lidocaine, diclofenac, topical is available over the counter and my prescription. OTC topical diclofenac is limited to a 1% concentration while prescription strength provides either 1% or 3%. Patients report the 3% concentration to be more effective than the 1% as would be expected and the 3% appears to be covered by Medicaid, at least in some cases. Topical NSAIDs provided similar pain relief to oral NSAIDs yet are much safer with fewer side effects. In fact, diclofenac when applied topically results in significantly higher muscle and joint (synovial) tissue levels compared with orally ingested diclofenac. While there is no research that distinguishes one topical NSAID as being better than another, diclofenac appears to be the most commonly available.
Recent studies have raised concerns regarding the safety of oral NSAIDs use in older adults and those with high blood pressure, diabetes, or cardiovascular comorbidities. Current research, however, indicates that topically applied diclofenac is associated with significantly lower rates of side effect in these high risk groups, noting that gastrointestinal, kidney and cardiovascular side effects are rare and did not differ by age or comorbidities.
There is some evidence that in acute pain, gels may be better than patches, but for chronic pain, patches may better (lower blood levels).
Topical diclofenac is recommended for most musculoskeletal pain, including:
- Acute & Chronic Muscle Pain (sore muscles and trigger points), Sprains and Tendonitis
- Arthritis – osteoarthritis & rheumatoid arthritis, bursitis
- Carpal tunnel syndrome
- Neck and Low back pain – herniated disc disease, failed back surgery syndrome
Dosing of topical diclofenac by using the Dosing Card that comes in the box:
- Upper body areas (hand, wrist, elbow): 2.25 inches = 2 g of diclofenac 1%; Max: 8 g/joint/day up to 32 g/day totals; use lowest effective dose, shortest effective tx duration; avoid occlusive dressings or hea
- Lower body areas (foot, ankle, knee): 4.5 inches = 4 g of diclofenac 1%; Max: 16 g/joint/day up to 32 g/day totals; use lowest effective dose, shortest effective tx duration; avoid occlusive dressings or hea
- Use 4 times a day every day for up to 21 days (OTC label)
- Avoid applying larger amounts than recommended which could lead to significant systemic absorption and the associated side effects
Per OTC label: “may take up to 7 days to work for arthritis pain; it is not for immediate relief.”
A word of caution is needed when selecting OTC topical pain medicines – beware of brand names that mislead as to the content of the product. For example, in the images below note that the constituent found in the product is not suggested by the product name. Always identify the product constituent, do not be mislead by the product name.

Capsaicin
Capsaicin is a compound derived from chili peppers that has analgesic properties. It is used as a homeopathic remedy counter-irritantnto treat burning pain using the concept of “treating like with like.” It is available in many OTC products at strengths ranging from 0-25-0.75% and as an 8% prescription medication.
Mechanism of Action:
Capsaicin binds to nerve endings in the skin (cutaneous pain receptors or nociceptors) to activates the transient receptor potential vanilloid 1 (TRVP1) pain receptor. Repeated applications or high concentrations provide pain relief due to reduction in activity of TRPV1 c by depleting their chemical stores.
OTC Capsaicin
Effectiveness:
While approximately half the time patients using OTC products obtain significant benefit at 4 weeks of application, half or more users experience side effects that often drive discontinuation of use. OTC capsaicin is not generally recommemded by arthritis experts.
Side Effects:
Application of capsaicin causes an initial burning sensation along with redness of the skin that often persists.
Capsaicin 8% (Qutenza) patches (Rx)
Prescription 8% (Qutenza) patches are applied by clinicians in their office every 30 days. Up to four patches are placed applied to the painful areas after pre-treatment with local anesthetic and left in place for 30 minutes (feet) to 60 minutes (other areas). Conditions treated include painful diabetic neuropathy and post-herpetic neuralgia.
Effectiveness:
Approximately 30% or more patient achieve at least 50% reduction in their pain, although a full response may require a minimum of two treatments
Application of the 8% capsaicin are generally well tolerated, particularly in painful diabetic neuropathy due to the destruction of small fiber nerves associated with the disease.
Other OTC Topical Medications
Menthol & Camphor
These compounds have deep roots in Eastern medicine and have historically been used for alleviating pain, cold symptoms, and pruritus in various cultures. However, as these compounds are not as well recognized in Western medicine, clinical research is sparse. Based on existing research, topical agents containing menthol and camphor are potentially effective at treating pain, upper respiratory infection symptoms, and pruritus in addition to potentially functioning as an antimicrobial. However, with a limited number of studies addressing these compounds, no definitive recommendation can be made regarding their use, especially for pain. Menthol also functions as a penetration enhancer when used with other medications, helping drive the other medication into the subcutaneous tissues and enhancing their effectiveness.
Effectiveness:
Analgesic benefits include muscle pain and muscle spasm, knee osteoarthritis and neuralgias.
Mechanisms of Action
Menthol is a selective activator of transient receptor potential melastatin-8 (TRPM8) channels and is also a vasoactive compound. As a topical agent, it acts as a counter-irritant by imparting a cooling effect and by initially stimulating nociceptors and then desensitizing them. Topically applied menthol may also activate central analgesic pathways. At high concentrations, menthol may generate cold allodynia. Camphor activates TRPV1 and inhibits TRPA1, on which menthol also has a bimodal action, resulting in an analgesic effect.
Brand names of different formulations of these compounds include: Icy Hot, Biofreeze, Salon Pas, Bengay, Two Old Goats – Arthritis,Sore No More, and Tiger Balm.

Menthol and. Diclofenac
In 2017 study, 18 healthy volunteers aged 18 – 50 years underwent consecutive 3-day treatment regimens in each of 3 treatment groups:
- 4 g of topical 1% diclofenac + 3% menthol gel administered 4 times daily;
- 4 g of topical 1% diclofenac sodium gel (Voltaren Gel) applied 4 times daily;
- Oral diclofenac sodium tablets 50 mg 3 times daily.
The diclofenac/menthol combination delivered significantly higher exposures of diclofenac compared with Voltaren Gel. A higher number of adverse events (AEs) occurred with the topical diclofenac/menthol combination (61%) vs. Voltaren Gel (22%) or oral diclofenac (6%); but most were local skin reactions. No difference in systemic AEs was observed among the groups.
Systemic exposure was significantly lower with the topical diclofenac/ menthol treatment regimens compared with oral diclofenac.
Salicylates
Some OTC formulations include trolamine salicylate, methyl salicylate and other salicylates that are chemically related to aspirin and may also be found in herbal based products including willow bark. Salicylates relieves minor pain in muscles and joints works by decreasing inflammation. There is little definitive evidence comparing different salicylates effectiveness but they are commonly used especially in traditional and folk remedies.
Brand names of different formulations that may have salicylate compounds include: Aspercreme, Blue Emu, and others.
Natural, Plant-Based Compounds
Terpenes: (BCP, Linalool)
Terpenes are fragrant chemicals found in many plants and spices. They may serve two functions when applied topically: they may provide an enhanced carrier function to other constituents with which they are applied, including CBD. Additionally, some terpenes offer their own therapeutic benefits, particularly β-caryophyllene.
For information regarding specific terpenes, see below:
Arnica
Arnica belongs to the Asteraceae family, a group of flowering plants containing several well-known members, such as marigold, daisy, and chamomile. Arnica has been used in traditional medicines for centuries in Europe and North America and has been used in homeopathic medicine for dozens of pathological conditions, including joint and muscle pain, inflammation, and arthritis. It has been proposed to have various therapeutic properties, including anti-inflammatory, analgesic, anti-microbial, anti-rheumatic, antiarthritic, and antineoplastic activities.
There are several forms of homeopathic arnica commercial products, including gels, creams, roll-ons, teas, pellets, liquids, and tablets but topical preparations are the most commonly used. These products are widely available in retail pharmacies ranging in strengths.
Effectiveness
Arnica offers comparable benefits to topical NSAID medications such as ibuprofen and diclofenac for pain with different medical conditions including post-traumatic ankle sprains, tendinitis, arthritis and chronic low back pain. It also has fewer adverse effects along with lower costs. In a 2013 Cochrane review, arnica gel was reported to be non-inferior to topical ibuprofen and “probably improves pain and function as well as topical NSAID drugs do …with no better (and possibly worse) adverse event profile.”
Safety
In clinical trials, adverse skin reactions have been reported with topical arnica. Contact dermatitis can develop, resulting in a rash, itching, and dry skin. Allergic reactions with topical arnica are cross-reactive with plants in the Compositae and Asteraceae families.
Mechanisms of Action
It is not clear as to how specifically arnica works on pain but it involves inhibitory activity on the expression of TNF-α, IL-1β, IL-6, and IL-12.
Frankincense (Boswellia serrate)
Indian frankincense is a plant extract used in Ayurvedic medicine as a remedy to treat inflammation and pain and a number of diseases. Frankincense is a natural product of Boswellia trees and oil and water extracts have long been used topically.
Effectiveness
Of interest are case reports of individuals with long-standing, debilitating benign essential blepharospasm (spasm of eyelids) achieving significant symptom relief after regular use of topical frankincense essential oil. Topical frankincense appears to offers an effective treatment option for this chronic, progressive condition.
Taken orally frankincense reduces inflammation in joints to aid in arthritis pain but definitive evidence is lacking for its benefit when applied topically. In the first randomized, double blind, placebo controlled study of topical frankincence for knee osteoarthritis, a 2023 study demonstrated decreased pain severity and stiffness of the knee and improved daily activity.
Mechanisms of action
Boswellic acids present in frankincense resin reduce inflammation by inhibiting 5-lipoxigenase enzyme as well as NF-ĸB (nuclear factor kappa B) and TNF-α (tumor necrosis factor in many inflammatory pathways. Additionally, findings suggest that topical application of frankincense with its active ingredients (including the terpenes α-pinene, linalool, and 1-octanol) have significant anti-inflammatory and analgesic benefits by inhibiting cyclooxygenase-2 (COX-2), in a similar mechanism by which NSAIDs such as ibuprofen and naproxen work.
Compounded Topical Medications
Based on a Cochrane review published recently in 2020 (Compounded Topical Pain Creams- Review of Select Ingredients for Safety, Effectiveness, and Use (2020)):
In most if not all cases there is simply inadequate research to provide definitive conclusions regarding the effectiveness of the medications reviewed. Additional research is needed to determine the effectiveness of all these medications. However, when topically applied appropriately, there are no significant safety concerns for any of the medications described here other than local skin irritation. Importantly, however, the absence of safety data does not prove safety or indicate that adverse events have not occurred. Indiscriminate use over large skin areas or use on non-intact skin can have safety concerns. Typically a large percentage of the time, when a product or medication cannot be patented there is a lack of meaningful research.
Key Definitions
- Creams: A semisolid oil-in-water emulsion for application to the skin. Creams are spreadable and easily rub into the skin without a greasy residue, and can be washed off with water.
- Excipient: A pharmacologically inactive ingredient used in the formulation of a drug that lends various functional properties to the drug formulation (i.e., dosage form, drug release, etc.). They are also sometimes referred to as diluents, bases, or carriers and can sometimes increase absorption of active ingredients.
- Gels: Also referred to as jellies, gels are a semi-solid dosage form that appears transparent or translucent and employs either a hydrophobic or hydrophilic base.
- Lotions: While similar to a cream, lotions have a more liquid consistency. The lower viscosity may provide a cooling effect to the area where applied when solvents in the lotion evaporate.
- Ointments: A semi-solid preparation with four general classes ranging from occlusive, hard to remove hydrocarbon bases, to easily washable water soluble bases.
- Penetration enhancer: An excipient or vehicle that aids in absorption of ingredients through the skin.
- Vehicles: A component that is used as a carrier or diluent in which liquids, semi-solids, or solids are dissolved or suspended.
The Terms Effectiveness and Efficacy
When reading any of the journal articles listed below, one will encounter the terms Effectiveness and Efficacy. While similar, the terms are not synonymous. Efficacy refers to the therapeutic effect of a treatment under controlled conditions, while effectiveness refers to the therapeutic effect in “real-world” situations in which certain contextual measures (e.g., placebo effect) may not be strictly controlled and broad outcome measures (e.g., health-related quality of life) are considered.
Non-Steroid Anti-inflammatory Drugs (NSAIDs)
Nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit the cyclooxygenase enzyme to reduce inflammation and pain. Compared with oral formulations, topical NSAIDs work only locally (when limited to concentations < 5%. Studies have shown that topical NSAIDs provided similar pain relief to oral NSAIDs for patients with chronic osteoarthritis and for patients with acute musculoskeletal pain. High-quality evidence supports the analgesic benefit of several topical NSAIDs, including diclofenac and ketoprofen. Some OTC formulations include methyl salicylate or other salicylates that are chemically related to aspirin and may also be found in herbal based products including willow bark. There is little definitive evidence for salicylates effectiveness but they are commonly used especially in traditional and folk remedies.
Systematic reviews of placebo-controlled randomized controlled trials confirm the effectiveness of several topical NSAIDs in treating pain from soft tissue injuries and chronic osteoarthritis. For acute sprains and strains, topical diclofenac and ketoprofen improved pain by 50% from baseline within 1 week. For chronic hand and knee osteoarthritis, topical diclofenac and ketoprofen improved pain by 50% within 6 weeks.
Topical NSAIDs are safer than oral NSAIDs by avoiding the risks of gastritis, G.I. bleeding, injury to kidneys or liver and risk of cardiovascular complications. Common adverse events from topical agents are mild and include local skin reactions (e.g., dry skin) and itching).
Naproxen
Naproxen has been used in compounded formulations, but no evidence is available that it is superior to topical diclofenac. Since topical diclofenac is available both by prescription and over-the-counter, compounding with naproxen is not generally recommended in favor of diclofenac.
Effectiveness:
There is limited and inconsistent evidence to suggest that naproxen (1–10 percent gel) is effective to treat pain related to soft tissue injuries. A double- blinded, randomized study that compared 10 percent naproxen gel and a placebo in 120 patients with soft tissue injuries (mostly synovitis and tendinitis) did find the naproxen gel significantly reduced pain.
Dermal penetration/bioavailability:
One study compared topical application of naproxen topical application of 1 percent naproxen sodium gel prepared without penetration enhancers. Compared to oral administration of sodium naproxen tablets, topical application showed significantly lower maximum blood concentration, similar time to reach the peak blood concentration, earlier terminal elimination half- life (1 hour sooner), but higher area under the curve (total exposure time.
Unfortunately, no studies are available that evaluate the intra-articular joint levels of naproxen resulting from topical versus oral administration of the drug.
Safety and adverse effects:
Topical naproxen may be associated with skin irritation and itching.
Neuropathic Agents:
Clonidine
Clonidine has been in clinical use for over 40 years, initially for treatment of hypertension, but later shown to be effective for treatment of acute and chronic pain. Clonidine ihas been described as an extremely potent pain medication with potency equal to or greater than that of morphine when used to treat acute and chronic pain intravenously or into the spine. However, systemic use of clonidine is limited by significant side effects including sedation, dry mouth, low blood pressure, and rebound hypertension.
Topical forms of clonidine are used to limit side effects but obtain analgesic benefits. Clonidine is lipophilic and easily penetrates the skin to reach the local pain pathways. The half-life of clonidine is about eight hours, thus it should be applied three times daily. Clonidine must be prepared by compounding pharmacies because no commercial preparation is available.
Effectiveness
Several animal and some human studies have shown that topical clonidine is an effective analgesic forf neuropathic pain but not likely for postoperative or inflammatory pain. A Cochrane review published in 2022 concluded “that a higher percentage of adults with painful diabetic neuropathy (PDN) may achieve pain relief of 30% or greater when treated with topical clonidine ( compared with placebo (48% versus 36%); however, the evidence for this outcome is very uncertain. Eight more people would have to be treated with topical clonidine compared to placebo for one more person to achieve moderate benefit. As such, topical clonidine used as a compounded cream may be recommended for peripheral neuropathic pain, probably in combination with other agents such as gabapentin or ketamine for someone with neuropathic pain otherwise resistant to more commonly recommended agents.
How clonidine works
Clonidine is a presynaptic alpha-2-adrenergic receptor agonist and targets receptors located in the brain, spinal cord, and dorsal root ganglia and on sensory neurons.
Gabapentin
Gabapentin (Neurontin) along with pregabalin (Lyrica) is one of the gold standard treatments for neuropathic pain. Evidence of benefit with oral use of gabapentin is quite good although not everybody does respond and it is not tolerated by some due to drowsiness or other side effects. Evidence for topical gabapentin is scarce, but nevertheless there is evidence to support topical use and safety.
Effectiveness:
Randomized controlled trials There are no relevant RCTs that examine the single-drug use of gabapentin in compounded topical creams to treat pain when applied to intact skin. However, a published case series in patients with mixed neuropathic pain reported benefit in 20 of 23 patients when treated with gabapentin 6% topically applied three times per day. Eleven of 23 patients reported at least 30 percent pain reduction, and 2 of 3 patients with postherpetic neuralgia reported reduction in pain by 60 percent and 57 percent..
Dermal penetration/bioavailability:
Evidence demonstrates that topical gabapentin can be detected at low concentrations in urine confirming that topical gabapentin penetrates the skin but the absorption varies greatly with the excipient used.Studies of urine concentration in patients exposed to topical gabapentin suggest very low to undetectable absorption rates.In patients taking oral gabapentin, average urine concentration levels are greater than 10,000 ng/mL. In contrast, in patients using topical gabapentin, average concentrations are 261 ng/mL.
Penetration enhancers:
Studies showed that gabapentin 6% with Carbopol hydrogels containing dimethyl sulfoxide (DMSO) or 70% ethanol, and a compounded gabapentin 10 percent in Lipoderm formulation, were able to facilitate permeation of the gabapentin molecule across human skin. Another study demonstrated formulations compounded using Lipoderm and Lipoderm ActiveMax enhancerss were able to permeate skin.
Safety and adverse effects:
There is insufficient evidence to determine the safety of topical gabapentin. However, if systemic absorption to therapeutic levels is achieved through topical application, there is potential for side effects similar to other routes of administration (e.g., oral). That being said, topical application is not likely to allow for therapeutic blood levels based on the urinary concentration data noted above as well as the rare, if any, complaints of systemic side effects reported.
Ketamine
Ketamine is a medication, gaining much attention in the recent times largely for it’s affective Ness with severe depression, but also regarding its effectiveness for neuropathic pain when used intravenously. Evidence for benefit with topical ketamine remains limited, but when doses are maintained as recommended, there appears to be very few side effects. There is off label use of ketamine delivered by nasal spray which is also getting some attention but research is lacking as to its benefits and safety.
Effectiveness:
There is mixed evidence regarding topical ketamine, some indicating that it is not superior to placebo for conditions including postherpetic neuralgia, complex regional pain syndrome (types I and II), painful diabetic neuropathy, and other types of neuropathic pain. Other trials suggest that topical ketamine in 5-10% gel may reduce pain in diabetic neuropathy and neuropathic pain associated with spinal cord injury and it may reduce allodynia in complex regional pain syndrome.
In a case of a 72-year-old woman with with CRPS I and severe pain, swelling, and a poor quality of life was treated with ketamine 10% cream and PEA (palmitoylethanolamide) capsules. The swelling improved, and the patient was more mobile at 1 month and continued to improve at 2 months.
Dermal penetration/bioavailability:
Topical ketamine can penetrate human skin. Serum concentrations of ketamine and its metabolite norketamine have been detected following topical use, although far below therapeutic concentrations. Modifications to the ingredient or excipient may increase absorption.
Limited evidence suggests that topical ketamine is associated with minimal adverse effects after therapeutic application. Application of excessive amounts of ketamine containing topical products can lead to significant altered mental status and seizures. In a case report, a 35-year-old man who applied excessive amounts of a topical pain cream containing ketamine, baclofen, amitriptyline, lidocaine, and ketoprofen presented to the hospital unresponsive after a seizure.
Antispasmodic Agents:
Baclofen
There are insufficient studies to provide evidence on the effectiveness of topical baclofen to treat pain when applied to intact skin. However, there are case reports supporting its benefit and safety.
Muscle Spasm
Oral and topical baclofen is FDA approved to treat reversible muscle spasticity. Baclofen is thought to be primarily a centrally acting drug, is a structural analogue of GABA, and an agonist of GABAB receptors in the CNS with the greatest density in the dorsal horn of the spinal cord. By binding to these receptors, synaptic spinal reflexes are inhibited, thus reducing muscle tone and especially flexor spasms.
Pain
Evidence from animal studies suggests that baclofen may have a peripheral analgesic effect also. A case report describing a 65-year-old woman with neuropathic pain in her legs reported as 9 on a 0–10 scale. She was initially treated with a compounded analgesic cream, based on baclofen 5 percent and advised to apply 1 gram maximally three times per day. After 2 weeks, she reported reduction of her pain by more than 95 percent based on one application daily, but she complained of numbness in her legs. The dose was reduced to baclofen 2 percent, and she reported benefits with use only 1–3 times per week for 6 months without side effects.
Another case report describes a 54-year-old woman with neuropathic pain in both feet reported as 8 out of 10 on the NRS following chemotherapy treatment despite being prescribed oral gabapentin 2,000 mg daily and oxycodone 20 to 30 mg daily. Pain was reduced to 3 by a test application of compounded topical baclofen 5% cream,
Antidepressant Agents:
Amitriptyline
Amitriptyline taken orally has long been recommended for treating neuropathic pain and is considered in some recommendations to be a first level treatment. More recent studies have offered little support for its pain benefit taken orally and side effects include dry mouth and drowsiness are not uncommon. In fact, amitriptyline is commonly prescribed for night time use for insomnia.
Effectiveness:
There is limited evidence to suggest that topical amitriptyline is effective to treat neuropathic pain when applied to intact skin. Case reports demonstrate amitriptyline (5% and 10%) is effective with neuropathic pain in the hands and feet where all patients noted partial relief with the 5% cream and almost complete relief with the 10% cream. Two patients reported tiredness & drowsiness with 10% cream.
Dermal penetration/bioavailability:
Limited evidence suggests that a minimal amount of topically applied amitriptyline penetrates through human skin. Serum concentrations of topical amitriptyline have been detected at very low levels following topical use. A 62-year-old woman with pain in the upper arms and left foot attributable to multiple sclerosis was prescribed 5% amitriptyline cream applied to the upper forearms that resulted in decreased pain in the foot and upper arms after several minutes delay.
Safety and adverse effects:
Topical amitriptyline is associated with minimal adverse effects such as skin irritation, dryness, itching and redness, and drowsiness.
Oral amitriptyline is an FDA-approved tricyclic antidepressant that was originally developed as a mood-regulating agent. It is thought to work by inhibiting the reuptake of norepinephrine and serotonin by presynaptic neuronal membranes in the CNS. At the spinal cord, amitriptyline exhibits ion-channel blocking effects on sodium, potassium, and NMDA channels. Norepinephrine, and sodium and NMDA channels, are involved in maintenance of some types of neuropathic pain. Off-label use of the oral formulation has been found to consistently reduce neuropathic forms of pain to a greater degree than comparison placebo groups.
Doxepin
Doxepin, like amitriptyline, is an oral antidepressant medication frequently prescribed for night time use for insomnia. However, also like amitriptyline, it is
Effectiveness:
There is limited evidence to suggest that topical doxepin may be effective to treat chronic neuropathic pain when administered at 3.3 percent concentration as an aqueous cream on intact skin. A case report showed that a 32-year-old female patient with complex regional pain syndrome type 1 resulting from a wrist injury experienced significantly reduced pain after 2 weeks of twice-daily topical application of doxepin cream.
Dermal penetration/bioavailability:
There is limited evidence to suggest that topical doxepin penetrates through human skin. One preclinical study detected serum concentrations that overlap with therapeutic concentrations (reported as 30–150 ng/mL).
Safety and adverse effects:
Evidence supports that topical doxepin is associated with minimal adverse effects. One clinical study determined potential effects include local stinging or burning, drowsi ness, headache, rash, and itching/allergic contact dermatitis. Drowsiness may be caused by systemic absorption.
Mechanism of Action
Doxepin is an FDA-approved psychotherapeutic agent (oral, topical) from the class of dibenzoxepin tricyclic compounds. The mechanism of action of doxepin has not been confirmed. The current understanding is that doxepin prevents reuptake of norepinephrine into nerve terminals by influencing activity in the synapse; this allows neurotransmitter activity to be prolonged. Norepinephrine is thought to be involved in the maintenance of some types of neuropathic pain, and this provides a rationale for off- label use of doxepin to treat certain types of pain.
Others
Ambroxol
Ambroxol is a drug with several properties including potent local anesthetic and anti-inflammatory activity. It has been studied in patients with neuropathic pain, including trigeminal neuralgia, and has shown good pain relief following topical application of 20% ambroxol cream. In a case series of CRPS patients, topical 20% ambroxol reduced spontaneous pain, edema, allodynia, hyperalgesia, and skin reddening and improved motor dysfunction and skin temperature. The evidence for topical ambroxol in neuropathic pain remains limited but it might be beneficial in some patients with localized neuropathic pain.
Mechanism of Action
Ambroxol is a very potent sodium channel (Nav) blocker, approximately 40 times stronger than lidocaine, and probably preferentially blocks the subtype Nav1.8, which is responsible for repetitive firing and neuronal excitability.
Compounded Drug Combinations
In Dr. Ehlenberger’s experience prescribing a compounded, topical cream containing amitriptyline, baclofen, diclofenac, gabapentin, ketamine and lidocaine over the last 15 years, he found a significant number of patients who experience meaningful pain relief from its use, often intermittently.
Case report described significant pain relief with a combination gel with gabapentin 6%/amitriptyline 2%/lidocaine 5%/ ketoprofen 10% in a patient following gall bladder surgery. There are multiple case reports of various combinations of topical medications demonstrating pain benefits but no gold standard double blinded, random controlled trials to offer definitive evidence of benefit.
Compounded Three-Drug Combinations: Ketamine, Amitriptyline, and Lidocaine
Effectiveness
Clinical studies: A 1% ketamine/2% amitriptyline/5% lidocaine gel was evaluated in 16 patients with neuropathic pain from radiation-induced dermatitis. Patients applied ~4 mL to the painful areas three times daily until 2 weeks after completion of radiotherapy. A reduction in scores for intensity, sharpness, burning, sensitivity, unpleasantness, and deepness was found 30 minutes after application and the reduction in burning was maintained for 2 weeks posttreatment.
Traditional Chinese Topical Medications
It should be noted that the traditional Chinese system of medicine (TCM) is based on completely different principles and understanding of health and disease. In TCM health becomes impaired related to the proper balance of flow of “chi.” the life energy that flows through meridians distributed throughout the body. This inherent difference in understanding disease states starts with different diagnostic approache and completely different treatment approaches not based on the western principles of anatomy and physiology.
Consequently one cannot simply establish a diagnosis based on western principles of diagnostio evaluation then proceed to select a TCM medication for treatment. It simply does not work that way. As with any medical systtem, the success of treatment is based on the accuracy of diagnosis. While the TCM medications reviewed here are typically used for common musculoskeletal ailments associated with pain, such as arthritis, it is important to seek a diagnostic evaluation by a clinician trained in TCM prior to reaching out for treatment.
Topical TCM treatment is widely utilized for muscle injuries within the Chinese community and comes in various forms, including paste, patch, balm, liniment or oil. Generally, side effects of these topicals are rare, although instances of contact allergy and dermatitis occasionally occur. However, many topical TCM products consist of multiple herbs, often ranging from 5 to over 20 herbs. This complex herbal mixing challenges our understanding of the individual components’ underlying therapeutic mechanisms. Only a few studies of TCM products have been able to provide evidence-based scientific data to support their efficacy.
Three popular and easily accessible herbs used topically for pain include:
(1) Carthami Flos (Carthamus tinctorius L.). A Chinese herb traditionally used for cardiovascular disease and bone injury in China to improve blood circulation. Limited studies support its benefit for vascular health.
(2) Dipsaci Radix (Dipsacus asperoides) A common herb used for musculoskeletal trauma. It promotes blood circulation to remove hematomas and alleviate pain. Recent scientific studies demonstated that Akebia Saponin D, the most abundant constituent of Dipsaci Radix, has anti-inflammatory effects.
(3) Rhei Rhizoma (Rheum palmatum Linn). A widely used traditional Chinese herb for wound healing. One of its derivatives, emodin, has been reported to promote the repair of excisional wounds in animal studies through complex mechanisms involving the stimulation of tissue regeneration .
CDR (Carthami Flos (Carthamus tinctorius L.), Dipsaci Radix (Dipsacus asperoides), Rhei Rhizoma (Rheum palmatum Linn)
A combination of the three herbs above as an herbal paste (named CDR) was found in clinical trials to be effective when applied topically for the treatment of conditions such as fifth metatarsal fractures and plantar fasciitis. A current study demonstrated that topical CDR treatment effectively enhances the regeneration, remodeling and maturation phases of muscle regeneration subsequent to injury.
DAEP – Dipsaci Radix, Achyranthis Bidentatae Radix, Eucommiae Cortex and Psoraleae Fructus
This herbal formula was simplified from a classic prescription “Xu Duan Wan” from “Fu Shou Jing Fang” has been used for treating the soreness and weakness of knees traditionally. These four herbs were selected for study in an animal model of knee arthritis based on their popularity in traditional practice. They include Dipsaci Radix (Dipsacus asperoides (DR), Achyranthis Bidentatae Radix (Achyranthis bidentata Blume) (ABR), Eucommiae Cortex (Eucommia ulmoides Oliv.) (EC) and Psoraleae Fructus (Psoralea corylifolia L.) (PF). An animal study evaluated the topical application of these four herbs as a paste named DAEP.
Effectiveness
Topical application of DAEP herbal paste to relieve knee pain due to osteoarthritis (OA) appears effective.
Mechanism of Action
Recognizing the underlying differences in TCM and western medicine, contemporary researchers still seek to determine a framework of how TCM medications work within a western model. In the case of DAEP, it is believed that its components are effective in arthritis pain because of its anti-inflammatory ingredients within the paste that target the suppression of the NF-κB pathway that promotes inflammation. Moreover, DAEP is thought to possibly suppress the progression of OA.
Constituent Ingredients Commonly Found In Chinese Herbal Medications (CHM)
Due to the large number of ingredients in Chinese herbal medication (CHM) formulations, the 3 most common are presented here.
Borneol
The most frequently included ingredient used in topical CHM formulations, borneol (bing pian), is non-toxic and non-irritating with a long history of use in CHM. Animal studies have shown it enhances permeation and drug delivery across skin, the blood-bran barrier and mucosal membranes.
Evidence for effectivness of borneol for pain includes a clinical study of 122 postoperative patients that found that when compared to placebo, a single topical application of 25% borneol for approximately 30 to 60minutes showed significantly greater reduction in postoperative pain without any adverse effects.
Xi Xin
The second most common ingredient is xi xin. Unfortunately no human studies of this ingredient alone appear to be available but animal studies support pain benefits for its extracts. The extracts include Methyl eugenol which is a major component of the essential oil of Asarum species, and Sarinin is a major lignin, a polyphenol known to have antioxidant, anti-inflammatory, and anti-cancer properties. Animal studies suggest methyl eugenol inhibits pain.
Xi Xin is derived from Asarum heterotropoides Fr. Schmidt var. mandshuricum (Maxim) Kitag., Asarum sieboldii Miq. var. seoulense Nakai, and Asarum sieboldii Miq.
Yan Hu Suo
The third most common ingredient in the topical CHMs is yan hu suo, derived from the rhizomes of Corydalis yanhusuo. In human studies, levo-tetrahydropalmatine (l-THP), an alkaloids found in yan hu suo, is thought to be effective for pain and drug addiction with dose-dependent reductions in pain. Animal studies demonstrate pain benefis for 3 alkaloids derived from Corydalis: dehydrocorybulbine (DHCB), levo-corydalmine (l-CDL) and dehydrocorydaline (DHC).
.
Penetration Enhancers
Application techniques to enhance absorption
The frequency that one applies a topical medication can affect absorption. Though studies are sparse, multiple doses of topically applied drug have been shown to deliver more drug through the skin than single doses. For example, 1 gram of cream applied twice daily may deliver more drug than 2 grams of cream applied once daily.
Compounds to enhance absorption
To improve the absorption of medications into the skin and deeper structures, topical medications may include compounds to enhance the depth and speed of absorption of the medication. Examples of penetration enhancers include:
- Menthol
- Eucalyptus oil
- Dimethylsulfoxide (DMSO)
Menthol
Menthols considered a rubefascient, a compound that simply turns the skin red, but functionally does so by increasing local blood circulation and vasodilation in areas in which it is applied. This process facilitates the absorption of medications into the skin and deeper structures which enhances their therapeutic benefits..
Eucalyptus Oil
Dimethyl sulfoxide (DMSO)
Dimethyl sulfoxide (DMSO) is a penetration enhancer used in compounded topical pain creams that has repeatedly occasioned concerns. DMSO appears to be used in compounded topical pain creams as both a penetration enhancer and as an active ingredient. While the evidence is far from conclusive, some studies suggest that DMSO may help treat osteoarthritis pain and complex regional pain syndrome . In fact, DMSO is the primary inactive ingredient in PENNSAID, an FDA-approved topical solution for osteoarthritis pain.
DMSO is a potent penetration enhancer but it may significantly enhance the absorption of other chemicals that could lead to their increased toxicity if applied at the same time. The instructions for use for PENNSAID caution patients to apply the medication to clean skin and to avoid the application of other drugs or cosmetics to the area due to the potential for an increased absorption that could potentially lead to toxicity.
Excipients or “inactive” ingredients
A wide range of bases, vehicles, and solvents are used to formulate topical pain creams, generally described as excipients, and these compounds can influence the attributes and characteristics of the topical (i.e., taste, smell, texture). Excipients are frequently called “inactive” ingredients but excipients can ultimately affect the final performance of the topical by affecting properties such as solubility, stability, release of the active ingredient, and skin penetration.
Safety Precautions
When using a topical analgesic:
- always read the package information before opening and using the medicine
- use the dose recommended on the packaging
- only apply to healthy, unbroken skin
- rub gently into the affected area
- do not use a heat or ice pack on skin where you have recently applied a topical analgesic (unless your health professional has said it is OK).
- Keep out of the reach of children and pets.
- Store between 20 and 25 degrees C (68 and 77 degrees F).
- Throw away any unused medication after the expiration date.
NOTE: These precautions are a summary and may not cover all possible information. If you have questions about your medicine, talk to your doctor, pharmacist, or health care provider.
Side Effects
All medicines, including those that are applied to the skin, have the potential to cause side effects. After topical analgesics are applied, most of the medicine is found in the skin and tissues where it was rubbed in. This can lead to skin irritation or redness, itching or rash.
A very small amount of active ingredient is also absorbed into the blood stream, so very rarely people may experience any of the following:
- breathlessness
- nausea
- indigestion
- abdominal pain
- swelling
- gastritis (inflammation of the stomach)
- allergy — skin rash, itching, hives, swelling of the face, lips, tongue, or throat
- Mild skin irritation, redness, or dryness
- contact dermatitis (inflammation of the skin following contact with the medicine).
This list may not describe all possible side effects. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Resources:
New Articles
New Articles – Synergy
- A Personal Retrospective: Elevating Anandamide (AEA) by Targeting Fatty Acid Amide Hydrolase (FAAH) and the Fatty Acid Binding Proteins (FABPs) – 2016
- Effect of Pharmacological Modulation of the Endocannabinoid System on Opiate Withdrawal: A Review of the Preclinical Animal Literature – 2016
- Dual-Acting Compounds Targeting Endocannabinoid and Endovanilloid Systems—A Novel Treatment Option for Chronic Pain Management – 2016
- Activation of Peripheral Cannabinoid Receptors Synergizes the Effect of Systemic Ibuprofen in a Pain Model in Rat – 2022
- Combination Therapy for Neuropathic Pain- A Review of Recent Evidence – 2021
- Combination Drug Therapy for the Management of Chronic Neuropathic Pain – 2023
- Local interactions between anandamide, an endocannabinoid, and ibuprofen, a nonsteroidal anti-inflammatory drug, in acute and inflammatory pain – PubMed – 2006
References:
Topicals – Analgesic Overviews
- Topical analgesics for acute and chronic pain in adults – an overview of Cochrane Reviews – 2017
- Topical Analgesics – Critical Issues Related to Formulation and Concentration – 2016
- Topical analgesic creams and nociception in diabetic neuropathy – towards a rationale fundament – 2016
- Skin Matters: A Review of Topical Treatments for Chronic Pain. Part One: Skin Physiology and Delivery Systems – 2015
- Skin Matters: A Review of Topical Treatments for Chronic Pain. Part Two: Treatments and Applications – 2016
Topicals – Arnica
Topicals – Formulations
Topical Cannabinoids
- Safety and Sourcing of Topical Cannabinoids – Many Questions, Few Answers – 2021
- Tolerability profile of topical cannabidiol and palmitoylethanolamide a compilation of single-centre randomized evaluator-blinded clinical and in vitro studies in normal skin – PubMed – 2021
- Cannabinoid Signaling in the Skin – Therapeutic Potential of the “C(ut)annabinoid” System – 2019
- Topical Cannabinoids for Treating Chemotherapy-Induced Neuropathy – A Case Series – 2021
- Cannabis-based medicines for chronic neuropathic pain in adults (Cochrane Review) – 2018
- Long-term and serious harms of medical cannabis and cannabinoids for chronic pain- a systematic review of non-randomised studies – 2022
- A Systematic Review on Cannabinoids for Neuropathic Pain Administered by Routes Other than Oral or Inhalation – 2022
- Antinociceptive and chondroprotective effects of prolonged β-caryophyllene treatment in the animal model of osteoarthritis Focus on tolerance development – 2021
- CB2 agonism controls pain and subchondral bone degeneration induced by mono-iodoacetate Implications GPCR functional bias and tolerance development – 2021
- Joint problems arising from lack of repair mechanisms can cannabinoids help – 2019
- Cannabinoid-based therapy as a future for joint degeneration. Focus on the role of CB2 receptor in the arthritis progression and pain an updated review – 2021
- CBD Effects on TRPV1 Signaling Pathways in Cultured DRG Neurons – 2020
CBD – Quality Control
- Safety and Sourcing of Topical Cannabinoids – Many Questions, Few Answers – 2021
- Quality Traits of “Cannabidiol Oils” – Cannabinoids Content, Terpene Fingerprint and Oxidation Stability of European Commercially Available Preparations – 2018
- Analysis of Cannabidiol, Δ9-Tetrahydrocannabinol, and Their Acids in CBD Oil:Hemp Oil Products – 2020
Topical CBD
Topical – Chinese (TCM)
- Traditional Chinese Medicine for Topical Treatment of Skeletal Muscle Injury – 2023
- Topical application of Chinese herbal medicine DAEP relieves the osteoarthritic knee pain in rats – 2019
- Chinese Herbs for Pain Relief + How to Use Them Plant-derived natural products targeting ion channels for pain – 2023
- Topical Traditional Chinese Medicines for Cancer Pain- A Systematic Review and Meta-analysis of Randomized Controlled Trials – 2023
Topical Clonidine
- Evaluation of the Percutaneous Absorption of Ketamine HCl, Gabapentin, Clonidine HCl, and Baclofen, in Compounded Transdermal Pain Formulations, Using the Franz Finite Dose Model – PubMed – 2016
- Topical clonidine for neuropathic pain in adults – 2022
Topical Compounded Medications
- Compounded Topical Pain Creams- Review of Select Ingredients for Safety, Effectiveness, and Use (2020)
- Evaluation of the Percutaneous Absorption of Ketamine HCl, Gabapentin, Clonidine HCl, and Baclofen, in Compounded Transdermal Pain Formulations, Using the Franz Finite Dose Model – PubMed – 2016
Topical Essential Oils & Aromatherapy
- Efficacy of Essential Oils in Relieving Cancer Pain- A Systematic Review and Meta-Analysis – 2023
- Effectiveness of aromatherapy for prevention or treatment of disease, medical or preclinical conditions, and injury- protocol for a systematic review and meta-analysis – 2022
- Efficacy of Topical Essential Oils in Musculoskeletal Disorders- Systematic Review and Meta-Analysis of Randomized Controlled Trials – 2023
Topical Frankincence (Boswellia Serrata)
- Evaluation of the effectiveness of topical oily solution containing frankincense extract in the treatment of knee osteoarthritis- a randomized, double-blind, placebo-controlled clinical trial – 2023
- α-Pinene, linalool, and 1-octanol contribute to the topical anti-inflammatory and analgesic activities of frankincense by inhibiting COX-2 – PubMed 2015
- Effects of Frankincense Compounds on Infection, Inflammation, and Oral Health – 2022
- Possible role of frankincense in the treatment of benign essential blepharospasm – 2023
Topical Gabapentin
- A Nutritional Supplement as Adjuvant of Gabapentinoids for Adults with Neuropathic Pain following Spinal Cord Injury and Stroke- Preliminary Results – 2023
- Gabapentin for chronic neuropathic pain in adults – 2017
- Gabapentin for chronic neuropathic pain and fibromyalgia in adults – 2014
- Evaluation of the Percutaneous Absorption of Ketamine HCl, Gabapentin, Clonidine HCl, and Baclofen, in Compounded Transdermal Pain Formulations, Using the Franz Finite Dose Model – PubMed – 2016
Topical Ketamine
- Treatment of chronic regional pain syndrome type 1 with palmitoylethanolamide and topical ketamine cream – modulation of nonneuronal cells – 2013
- Evaluation of the Percutaneous Absorption of Ketamine HCl, Gabapentin, Clonidine HCl, and Baclofen, in Compounded Transdermal Pain Formulations, Using the Franz Finite Dose Model – PubMed – 2016
- Topical and peripheral ketamine as an analgesic – PubMed – 2014
- Topical Ketamine with Other Adjuvants: Underutilized for Refractory Cancer Pain? A Case Series and Suggested Revision of the World Health Organization Stepladder for Cancer Pain – 2020
Topical Lidocaine
- Topical Lidocaine for Chronic Pain Treatment – 2021
- Topical Lidocaine plus Diclofenac as a Local Anesthetic Agent in Central Venous Catheterization; a Randomized Controlled Clinical Trial – 2021
- Topical Analgesia with Lidocaine Plus Diclofenac Decreases Pain in Benign Anorectal Surgery Randomized, Double-blind, and Controlled Clinical Trial – 2018
- Analgesic synergy between topical lidocaine and topical opioids – PubMed – 2000
Topical Menthol
- Looking Back to Move Forward- The Current State of Research on the Clinical Applications of Camphor- and Menthol-Containing Agents – 2023
- The role and mechanism of action of menthol in topical analgesic products – PubMed – 2018
- Menthol a natural analgesic compound – PubMed 2002
- Clinical efficacy of polyherbal formulation Eezpain spray for muscular pain relief – 2015
- Diclofenac systemic bioavailability of a topical 1% diclofenac + 3% menthol combination gel vs. an oral diclofenac tablet in healthy volunteers a randomized, open-label, crossover study – PubMed
Topical NSAIDs
- Topical nonsteroidal anti-inflammatory drugs – 2023
- Topical NSAIDs for acute musculoskeletal pain in adults – 2015
- Topical NSAIDs for chronic musculoskeletal pain in adults – 2016
- Topical analgesics for acute and chronic pain in adults – an overview of Cochrane Reviews (Review) – 2017
- Topical Anti-Inflammatories- Analgesic Options for Arthritis Beyond NSAIDs – 2021
- Pharmacological Treatment for Acute Traumatic Musculoskeletal Pain in Athlete – 2021
- Risk of Nonunion with Nonselective NSAIDs, COX-2 Inhibitors, and Opioids – 2020
- Topical Lidocaine plus Diclofenac as a Local Anesthetic Agent in Central Venous Catheterization; a Randomized Controlled Clinical Trial – 2021
- Topical Analgesia with Lidocaine Plus Diclofenac Decreases Pain in Benign Anorectal Surgery Randomized, Double-blind, and Controlled Clinical Trial – 2018
- Systemic bioavailability of topical diclofenac sodium gel 1% versus oral diclofenac sodium in healthy volunteers – PubMed
- Bioequivalence of diclofenac sodium 2% and 1.5% topical solutions relative to oral diclofenac sodium in healthy volunteers – PubMed
- Topical 3% diclofenac in 2.5% hyaluronic acid gel a review of its use in patients with actinic keratoses – PubMed
- Diclofenac systemic bioavailability of a topical 1% diclofenac + 3% menthol combination gel vs. an oral diclofenac tablet in healthy volunteers a randomized, open-label, crossover study – PubMed
Topical NSAIDs – Bioavailability
- Systemic bioavailability of topical diclofenac sodium gel 1% versus oral diclofenac sodium in healthy volunteers – PubMed
- Bioequivalence of diclofenac sodium 2% and 1.5% topical solutions relative to oral diclofenac sodium in healthy volunteers – PubMed
- Topical 3% diclofenac in 2.5% hyaluronic acid gel a review of its use in patients with actinic keratoses – PubMed
- Diclofenac systemic bioavailability of a topical 1% diclofenac + 3% menthol combination gel vs. an oral diclofenac tablet in healthy volunteers a randomized, open-label, crossover study – PubMed
Topical Opioids
- Topical opioids in mice analgesia and reversal of tolerance by a topical N-methyl-D-aspartate antagonist – PubMed – 1999
- μ‐Opioid receptors in primary sensory neurons are essential for opioid analgesic effect on acute and inflammatory pain and opioid‐induced hyperalgesia – 2019
- Efficacy and Safety of Topical Morphine A Narrative Review – 2022
- Analgesic synergy between topical lidocaine and topical opioids – PubMed – 2000
Topical PEA
- Immunomodulatory, Anti-Inflammatory, and Anti-Cancer Properties of Ginseng- A Pharmacological Update – 2023
- Efficacy of a fixed combination of palmitoylethanolamide and acetyl-l-carnitine (PEA+ALC FC) in the treatment of neuropathies secondary to rheumatic diseases – 2021
- Tolerability profile of topical cannabidiol and palmitoylethanolamide a compilation of single-centre randomized evaluator-blinded clinical and in vitro studies in normal skin – PubMed 2021
- Vulvodynia and proctodynia treated with topical baclofen 5 % and palmitoylethanolamide – PubMed 2014
- Topical analgesic creams and nociception in diabetic neuropathy – towards a rationale fundament – 2016
- Palmitoylethanolamide in the treatment of chronic pain caused by different etiopathogenesis – PubMed – 2012
- Clinical applications of palmitoylethanolamide in pain management- protocol for a scoping review – 2019
- Effects of Palmitoylethanolamide (PEA) on Nociceptive, Musculoskeletal and Neuropathic Pain- Systematic Review and Meta-Analysis of Clinical Evidence – 2022
- Palmitoylethanolamide in the Treatment of Chronic Pain- A Systematic Review and Meta-Analysis of Double-Blind Randomized Controlled Trials – 2023
- Palmitoylethanolamide is a new possible pharmacological treatment for the inflammation associated with trauma – PubMed 2013
- Efficacy of Palmitoylethanolamide for Pain- A Meta-Analysis – 2017
- New Approach to Chronic Back Pain Treatment- A Case Control Study – 2023
- Treatment of chronic regional pain syndrome type 1 with palmitoylethanolamide and topical ketamine cream- modulation of nonneuronal cells – 2013
- Tolerability profile of topical cannabidiol and palmitoylethanolamide a compilation of single-centre randomized evaluator-blinded clinical and in vitro studies in normal skin – PubMed – 2021
- Treatment of chronic regional pain syndrome type 1 with palmitoylethanolamide and topical ketamine cream – modulation of nonneuronal cells – 2013
Topicals – Neuropathic Pain
- Topical Treatments and Their Molecular Cellular Mechanisms in Patients with Peripheral Neuropathic Pain-Narrative Review – 2021
- Novel Drug Targets and Emerging Pharmacotherapies in Neuropathic Pain – 2023
- A pharmacological treatment algorithm for localized neuropathic pain – PubMed 2016
- Management of chronic neuropathic pain with single and compounded topical analgesics – PubMed – 2017
- A Systematic Review and Meta-Analysis on the Role of Nutraceuticals in the Management of Neuropathic Pain in In Vivo Studies – 2022
- Peripheral Mechanisms of Neuropathic Pain-the Role of Neuronal and Non-Neuronal Interactions and Their Implications for Topical Treatment of Neuropathic Pain – 2021
- Topical Treatments for Localized Neuropathic Pain – 2017
- Localized neuropathic pain- an expert consensus on local treatments – 2017
- Treatment of chronic regional pain syndrome type 1 with palmitoylethanolamide and topical ketamine cream – modulation of nonneuronal cells – 2013
- An Insight into Potential Pharmacotherapeutic Agents for Painful Diabetic Neuropathy – 2022
- Topical treatments for diabetic neuropathic pain (Review) – 2019
Topicals – Arthritis
- Antinociceptive and chondroprotective effects of prolonged β-caryophyllene treatment in the animal model of osteoarthritis Focus on tolerance development – 2021
- CB2 agonism controls pain and subchondral bone degeneration induced by mono-iodoacetate Implications GPCR functional bias and tolerance development – 2021
- Joint problems arising from lack of repair mechanisms can cannabinoids help – 2019
- Cannabinoid-based therapy as a future for joint degeneration. Focus on the role of CB2 receptor in the arthritis progression and pain an updated review – 2021
- CBD Effects on TRPV1 Signaling Pathways in Cultured DRG Neurons – 2020
- Local interactions between anandamide, an endocannabinoid, and ibuprofen, a nonsteroidal anti-inflammatory drug, in acute and inflammatory pain – PubMed – 2008
- Anti-Inflammatory Effect of Beta-Caryophyllene Mediated by the Involvement of TRPV1, BDNF and trkB in the Rat Cerebral Cortex after Hypoperfusion Reperfusion – 2022
- Assessment of NSAIDs as potential inhibitors of the fatty acid amide hydrolase I (FAAH-1) using three different primary fatty acid amide substrates in vitro – 2022
- Cannabinoid CB 2 Receptors Regulate Central Sensitization and Pain Responses Associated with Osteoarthritis of the Knee Joint – 2013
- β-Caryophyllene Mitigates Collagen Antibody Induced Arthritis (CAIA) in Mice Through a Cross-Talk between CB2 and PPAR-γ Receptors – 2019
- Prevalence and interference of neuropathic pain in the quality of life in patients with knee osteoarthritis – 2023
Topicals – Rheumatoid Arthritis
- Triterpenes as Potential Drug Candidates for Rheumatoid Arthritis Treatment – 2023
- Natural medicines of targeted rheumatoid arthritis and its action mechanism – 2022
- Rheumatiod Arthritis- An Updated Overview of Latest Therapy and Drug Delivery – 2019
Topical Terpenes
Terpenes – Routes of Use:
- The Effects of Essential Oils and Terpenes in Relation to Their Routes of Intake and Application – 2020
- Antiviral effect of phytochemicals from medicinal plants – Applications and drug delivery strategies – 2020
- Cannabinoid Delivery Systems for Pain and Inflammation Treatment – 2018
Terpenes – CB2 Receptor
- Cannabinoid-based therapy as a future for joint degeneration. Focus on the role of CB2 receptor in the arthritis progression and pain – an updated review – 2021
- β-Caryophyllene, a CB2 receptor agonist produces multiple behavioral changes relevant to anxiety and depression in mice – 2014
- The CB2 receptor and its role as a regulator of inflammation – 2016
- Cannabinoid CB2 Receptors Regulate Central Sensitization and Pain Responses Associated with Osteoarthritis of the Knee Joint
- Antinociceptive and chondroprotective effects of prolonged β-caryophyllene treatment in the animal model of osteoarthritis Focus on tolerance development – 2021
- CB2 agonism controls pain and subchondral bone degeneration induced by mono-iodoacetate Implications GPCR functional bias and tolerance development – 2021
- Joint problems arising from lack of repair mechanisms can cannabinoids help – 2019
- Cannabinoid-based therapy as a future for joint degeneration. Focus on the role of CB2 receptor in the arthritis progression and pain an updated review – 2021
- Antinociceptive and chondroprotective effects of prolonged β-caryophyllene treatment in the animal model of osteoarthritis Focus on tolerance development – 2021
- CB2 agonism controls pain and subchondral bone degeneration induced by mono-iodoacetate Implications GPCR functional bias and tolerance development – 2021
- Joint problems arising from lack of repair mechanisms can cannabinoids help – 2019
- Cannabinoid-based therapy as a future for joint degeneration. Focus on the role of CB2 receptor in the arthritis progression and pain an updated review – 2021
- Local interactions between anandamide, an endocannabinoid, and ibuprofen, a nonsteroidal anti-inflammatory drug, in acute and inflammatory pain – PubMed – 2008
- Anti-Inflammatory Effect of Beta-Caryophyllene Mediated by the Involvement of TRPV1, BDNF and trkB in the Rat Cerebral Cortex after Hypoperfusion Reperfusion – 2022
- Cannabinoid CB 2 Receptors Regulate Central Sensitization and Pain Responses Associated with Osteoarthritis of the Knee Joint – 2013
- β-Caryophyllene Mitigates Collagen Antibody Induced Arthritis (CAIA) in Mice Through a Cross-Talk between CB2 and PPAR-γ Receptors – 2019
Topical Terpenes – Wound Healing:
Topical Terpenes – Individual Terpenes
Topical β-Caryophyllene
- Beta-caryophyllene enhances wound healing through multiple routes – 2019
- Antinociceptive and chondroprotective effects of prolonged β-caryophyllene treatment in the animal model of osteoarthritis Focus on tolerance development – 2021
- CB2 agonism controls pain and subchondral bone degeneration induced by mono-iodoacetate Implications GPCR functional bias and tolerance development – 2021
- Joint problems arising from lack of repair mechanisms can cannabinoids help – 2019
- Cannabinoid-based therapy as a future for joint degeneration. Focus on the role of CB2 receptor in the arthritis progression and pain an updated review – 2021
- Antinociceptive and chondroprotective effects of prolonged β-caryophyllene treatment in the animal model of osteoarthritis Focus on tolerance development – 2021
- CB2 agonism controls pain and subchondral bone degeneration induced by mono-iodoacetate Implications GPCR functional bias and tolerance development – 2021
- Joint problems arising from lack of repair mechanisms can cannabinoids help – 2019
- Cannabinoid-based therapy as a future for joint degeneration. Focus on the role of CB2 receptor in the arthritis progression and pain an updated review – 2021
Synergies
- NSAIDs, Opioids, Cannabinoids and the Control of Pain by the Central Nervous System – 2010
- A Personal Retrospective: Elevating Anandamide (AEA) by Targeting Fatty Acid Amide Hydrolase (FAAH) and the Fatty Acid Binding Proteins (FABPs) – 2016
- Effect of Pharmacological Modulation of the Endocannabinoid System on Opiate Withdrawal: A Review of the Preclinical Animal Literature – 2016
- Dual-Acting Compounds Targeting Endocannabinoid and Endovanilloid Systems—A Novel Treatment Option for Chronic Pain Management – 2016
- Activation of Peripheral Cannabinoid Receptors Synergizes the Effect of Systemic Ibuprofen in a Pain Model in Rat – 2022
- Combination Drug Therapy for the Management of Chronic Neuropathic Pain – 2023
- Local interactions between anandamide, an endocannabinoid, and ibuprofen, a nonsteroidal anti-inflammatory drug, in acute and inflammatory pain – PubMed – 2006
- Involvement of Spinal CB1 Cannabinoid Receptors on the Antinociceptive Effect of Celecoxib in Rat Formalin Test – 2016
- Topical Lidocaine plus Diclofenac as a Local Anesthetic Agent in Central Venous Catheterization; a Randomized Controlled Clinical Trial – 2021
- Topical Analgesia with Lidocaine Plus Diclofenac Decreases Pain in Benign Anorectal Surgery Randomized, Double-blind, and Controlled Clinical Trial – 2018
- Efficacy and Safety of Topical Morphine A Narrative Review – 2022
- Analgesic synergy between topical lidocaine and topical opioids – PubMed – 2000
National Academy of Sciences
This website appears to be good resource for exploring medical marijuana.
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.
