“Illness is the doctor to whom we pay most heed; to kindness, to knowledge, we make promise only; pain we obey.”
-Marcel Proust
Prescription Medications:
Levorphanol
Levorphanol is an opioid that has been around for many decades, but despite it’s many unique and advantageous characteristics it remains under-utilized.
It is recommended to first read the following sections to become familiarized with some of the terms and concepts related here:
Also see:
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
.
Opioids – Levorphanol
Levorphanol was originally synthesized as a pharmacological alternative to morphine and was first approved for use in 1953. Levorphanol is an opioid that has many advantageous characteristics that make it a potentially very useful opioid for moderate to severe pain management.
- Due to its unique characteristics, levorphanol can be used to advantage for the treatment of pain in a variety of scenarios. Arguably it would not be warranted for initial management of acute pain, but when acute pains persists levorphanol may serve to suppress the development of peripheral and central sensitization and their role in transitioning from acute to chronic pain.
- Based on levorphanol’s multiple mechanisms for pain, it is believed to offer greater benefit than traditional opioids for neuropathic pain including conditions such as fibromyalgia (when opioids are needed) and peripheral neuropathies.
- With levorphanol’s purported ability to limit or reverse opioid analgesic tolerance, it is also appropriate for opioid rotation when chronic pain is refractory to treatment with other opioids. It can also be considered when there is potential for drug-drug or drug-food interactions that may limit the use of alternative opioids.
- Finally, because of its multiple mechanisms for its analgesic activity, levorphanol appears to impact respiratory depression to a lesser degree than traditional opioids at morphine analgesic-equivalent doses. This suggests levorphanol to potentially be a safer opioid for use in patients with sleep apnea and other conditions where concerns are present for respiratory depression. That being said, this potential for levorphanol’s improved safety remains theoretical as it has not been quantified nor should it be relied upon to avoid respiratory depression.
Multiple Mechanisms of Action
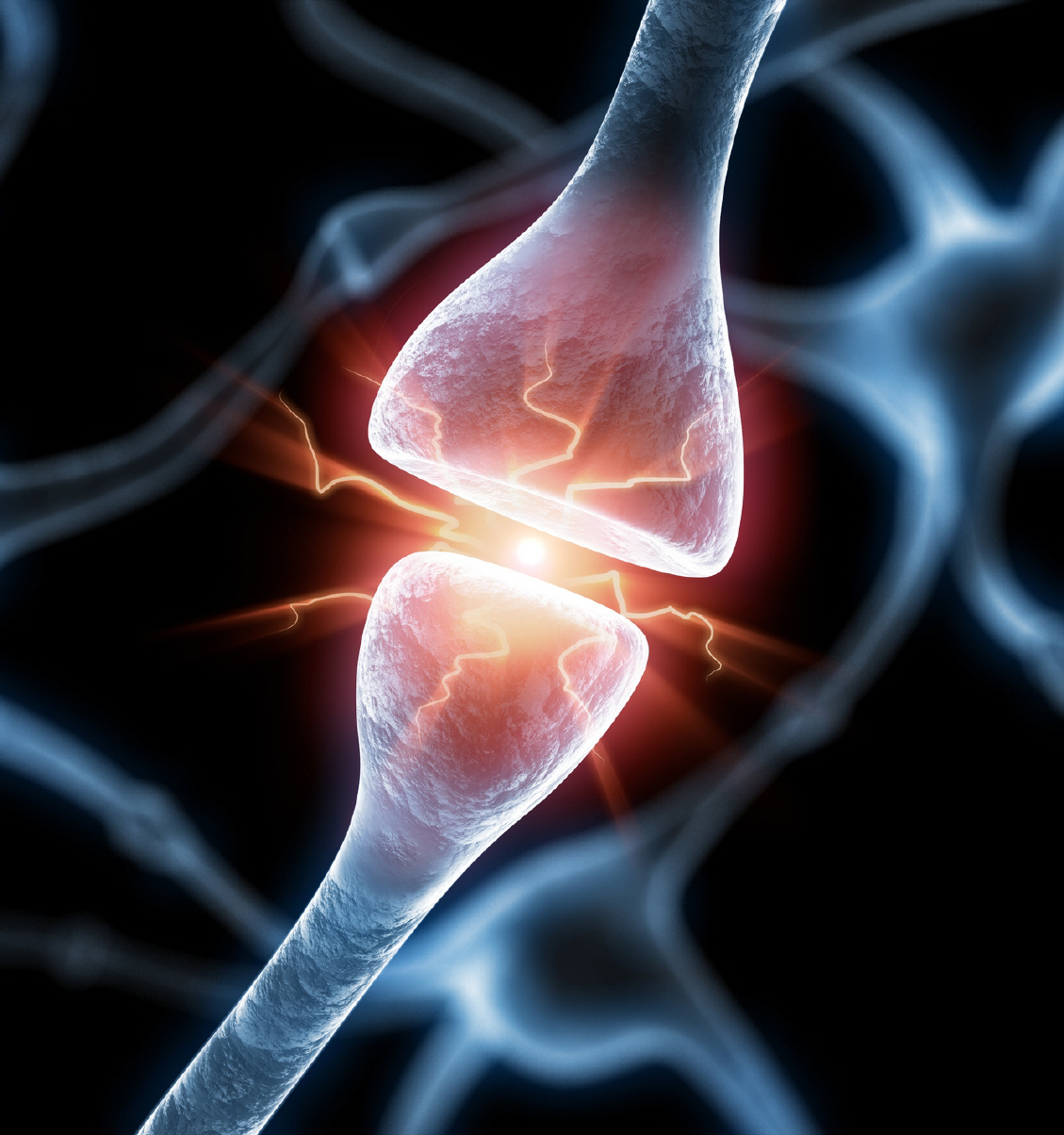
In addition to its direct action on the mu opioid receptor typical of all opioids, levorphanol has multiple additional mechanisms that contribute to its analgesic benefits. It also is an agonist of the delta and kappa (kappa 1 and 3) opioid receptors. Delta receptor agonists provide limited analgesic benefits, possibly for situations of persistent pain. Kappa receptor agonists produce analgesia primarily at spinal levels.
Levorphanol is an antagonist of the N-methyl-D-aspartate (NMDA) receptor which plays an important role in pain signalling and contibute to opioid analgesic tolerance and possibly the development of opioid induced hyperalgesia.
Levorphanol also acts of ascending and descending pain pathways between the brain and spinal cord inhibiting reuptake of both norepinephrine and serotonin. These mechanisms allow for analgesic benefits independend of the opioid system.
Potency
Milligram for milligram, levorphanol is considered to be 4-8x more potent than morphine when used orally (ME= 4-8). The usual recommended starting oral dose is 2 mg repeated every 6, 8 (most common), or 12-hours, depending on patient age and comorbidities. It is generally recommended to not exceed a total daily dose of 6 to 12 mg except in opioid-tolerant patients. When indicated, dosing can be slowly increased bearing in mind that it takes about 3 days for blood levels to stabilize after a dosage change.
When rotating from another opioid to levorphanol, care should be taken to do so cautiously due to wide variations in different patients responses. As such, one should assume a potential ME of levorphanol to be from 12 to 20 depending on how high the starting ME is as well as the potential for limited cross tolerance. It is suggested:
- If target rotation is less than 100 ME/day, levorphanol should be assigned a 12 ME
- If target rotation is between 100-299 ME/day, levorphanol should be assigned a 15 ME
- If target rotation is between 300-500 ME/day, levorphanol should be assigned a 20 ME
Important Caveats for Rotation
The above being an overview of rotation, it should also be advised that rotation need not be limited to one step but instead a gradual rotation can be implemented in stages to minimize sudden changes in analgesic benefits and marked impact of side effects. This also provides the patient greater confidence in managing the rotation since sudden changes is opioid management can be very intimidating to patients, especially when they are confronted with an unfamiliar opioid.
Additionally, when rotating opioids it is important to be available to provide close support by phone with the patient to ease them through the process and monitor potential safety and tolerability concerns.
Extended Duration of Action
Levorphanol has a longer duration of action than most opioids with pain benefit lasting from 6 to 15 hours. This is not a time-release medication so it can be broken in half to modify its dose and it can also be useful for those patients with gastrointestinal conditions that otherwise might not allow for use of time-release medications. Because the half-life of levorphanol is as long as 16-30 hours (the time required for half of a dose of a medicine to be metabolized and blood level reduced by 50%) , with chronic, daily use levorphanol does build up in the blood and caution is advised to not exceed recommended dosing.
Effectiveness for Nerve Pain
Levorphanol has a strong affinity and interaction with mu, kappa and delta opioid receptors along with a strong ability to block the NMDA receptor on nerve cells (see Neurobiology of Pain). While the exact mechanisms remain unclear, levorphanol potentially offers greater effectiveness for neuropathic (nerve) pain and fibromyalgia pain than other opioids. Another mechanism proposed for levorphanol’s analgesic benefit is its reuptake inhibition of both norepinephrine and serotonin, the same mechanism which it is believed that duloxetine (Cymbalta) provides pain benefits. Unlike methadone, levorphanol does not affect electrical conduction in the heart making it a potentially safer opioid alternative to methadone.
Some clinical studies have shown that levorphanol is effective for cancer and non-cancer pain even when other opioids have not been.
Possibly Effective for Opioid Tolerance and OIH
One of the proposed advantages for the use of levorphanol in the management of chronic pain lies in it’s proposed NMDA blocking action. Blocking the NMDA receptor is thought to limit or reverse opioid tolerance and opioid induced hyperalgesia (OIH) (see Neurobiology of Pain). Activation of NMDA receptors by glutamate is important in the development of OIH and NMDA antagonists like ketamine have been used to treat or reduce the development of OIH. Research has shown that methadone, another opioid thought to block NMDA, may be especially useful for patients with high opioid tolerance and OIH.
Levorphanol’s NMDA blocking action has been shown to be five times stronger than methadone, making levorphanol an especially attractive choice in these circumstances. Studies have also shown that methadone reverses analgesic tolerance resulting from chronic use of morphine. Based on levorphanol’s greater NMDA antagonist potency as compared with methadone, it has been postulated that levorphanol too may offer reversal of opioid analgesic tolerance, perhaps even more effectively. Ongoing research continues to explore this further.
Limited Drug Interactions
Metabolism by the Liver
Because levorphanol is not metabolized by the cytochrome P-450 (CYP-450) enzymes in the liver and other tissues as is the case with tramadol, oxycodone, hydrocodone, fentanyl and methadone, it is not susceptible to the common drug interactions that impact these enzymes. Instead, levorphanol is metabolized in the liver by 2nd phase metabolism, glucuronidation (UGT2B7), a mechanism much less vulnerable to drug interactions. Levorphanol’s inactive glucuronide metabolite is reported to be slowly re-converted to levorphanol again, arguing for one explanation for its extended duration of action.
While levorphanol has a relative lack of interaction with other medications compared with many other opioids, medications that impact UGT2B7 can affect levorphanol blood levels to increase or decrease the effects of levorphanol. Medications that inhibit UGT2B7 such as tricyclic antidepressants doxepin and(elavil/amitiptyline, phenothiazines (phenergan), may slow metabolic breakdown of levorphanol and increase or prolong the effects of levorphanol. Medications that induce or enhance UGT2B7 breakdown of levorphanol such as carbamazepine (Tegretol), phenobarbital and phenytoin (Dilantin), can reduce or shorten the effects of levorphanol.
P-glycoprotein (P-gp) transport
Levorphanol is not affected by the P-glycoprotein (P-gp) transporters so it ls less susceptible to genetic variants and drug interactions that impact P-gp-mediated levels of levorphanol in the brain and central nervous system.
Levorphanol, Liver and Kidney Disease
While all opioids should be used with caution in the presence of impaired liver function, those opioids metabolized by CYP-450 enzymes are more likely to be impacted then those metabolized by glucuronidation.
Levorphanol’s glucuronide metabolite is inactive and is slowly excreted through the kidneys but little unchanged levorphanol is found in the urine, bile or feces. As such dosage of levorphanol is not necessary in the presence of kidney disease.
Other Drug Interactions
It is important to remember that levorphanol, like all opioids, must be used with great caution with any other drug or medication that is sedating such as alcohol, benzodiazepines (Valium, Xanax, Klonopin etc.) and sleeping medications. This is especially true in patients at risk for sleep apnea and those with sleep apnea that are not consistent with their use of CPAP.
Side Effects
The potential adverse effects with levorphanol are similar to other mu opioid analgesics including nausea, vomiting, euphoria, altered mood or impaired thought processing, pruritus, flushing, difficulty urinating, constipation, and biliary spasm. No effects of levorphanol on the cardiac QT interval have been identified.
References
Levorphanol – Patient Information
Levorphanol – Overviews
- Levorphanol-forgotten-opioid_2007
- Is Levorphanol a Better Option than Methadone – 2015
- Levorphanol – Revisiting an Underutilized Analgesic
- Levorphanol use: past, present and future. – PubMed – NCBI
- levorphanol-an-optimal-choice-for-opioid-rotation-2016
Levorphanol – Pain Unresponsive to other Opioids
- Can levorphanol be used like methadone for intractable refractory pain? – PubMed – NCBI
- Kappa 3 receptors and levorphanol-induced analgesia. – PubMed – NCBI
Levorphanol – Opioid Tolerance, Hyperalgesia and NMDA Antagonism
- Changing Mechanisms of Opiate Tolerance and Withdrawal during Early Development – Animal Models of the Human Experience – 2011
- Are Glycine-B Sites Involved in the Development of Morphine Tolerance? – 2004
- A Comprehensive Review of Opioid-Induced Hyperalgesia – 2011
- Opioid-induced hyperalgesia – What to do when it occurs? – 2012
- Mu Opioids and Their Receptors – Evolution of a Concept – 2013
Levorphanol – Norepinephrine (Noradrenaline)
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.
