“The greatest evil is physical pain.”
― Saint Augustine
Toll-Like Receptor (TLR-4) Antagonists
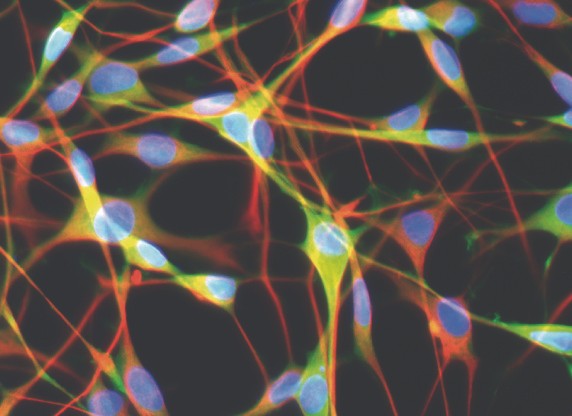
Toll-like receptors (TLRs) are a class of receptors found in the glia cells in the peripheral and central nervous system. Glial cells play a key role in the immune system by recognizing infectious agents such as bacteria and viruses. Activating TLR receptors stimulates the production of proteins (cytokines) that lead to inflammation as part of an immune response. Of the different TLRs, the TLR-4 receptor has gained attention recently in pain management.
TLR-4 activity is believed to play a role in pain, including the use of opioids. Research on the use of TLR-4 antagonists in fibromyalgia supports their potential for benefit in reducing the pain of fibromyalgia. As a side effect, opioids activate TLRs, especially the TLR-4 receptor, triggering the release of inflammatory modulators. With chronic use of opioids there is a constant low-level release of these modulators which is thought to reduce the effectiveness of opioids for pain over time (opioid analgesic tolerance, OAT) and contribute to the development of hypersensitivity to pain (OIH).
Medications that block these TLR-4 receptor (TLR-4 antagonists) appear to reduce pain, especially related to OAT, OIH and possibly opioid withdrawal-induced hyperalgesia (WIH). Hyperalgesia is an exaggerated, increased painful response to a stimulus which is normally painful.
See:
Resolving Inflammation
Also see:
Opioid Induced Hyperalgesia (OIH)
Withdrawal-Induced Hyperalgesia (WIH)
Naltrexone for Pain (coming soon)
Gabapentin (Neurontin) & Pregabalin (Lyrica)
Definitions and Terms Related to Pain
Key to Links:
Grey text – handout
Red text – another page on this website
Blue text – Journal publication
.
Please note: This page is still pending further development
Toll-Like Receptor (TLR-4) Antagonists
Toll-like receptors (TLRs) play a key role in the immune system by responding to pathogen-associated molecular patterns (PAMPs) such as lipopolysaccharide (LPS) that are expressed on infectious agents such as bacteria and viruses. In particular, the TLR-4 receptors stimulate the production of proteins (cytokines) including the inflammatory modulators TNF-α and interleukin-1 that are key players in immune response.
The stimulation of these TLR-4 receptors is believed to contribute to neuropathic pain and the expression of central sensitivity, hyperalgesia (hypersensitivity to painful stimuli), and allodynia (the perception of pain as the result of a non-painful stimulus). These conditions are associated with painful diagnoses including fibromyalgia, migraine headaches, chronic low back pain, TMJ syndrome, interstitial cystitis and endometriosis. TLR-4 receptors are also believed to be involved in opioid-induced hyperalgesia (OIH) and withdrawal-induced hyperalgesia (WIH).
See:
Opioids
Opioids are well known to be effective for pain of all types, though somewhat less so for neuropathic pain. Their effectiveness for pain is based on their activity of stimulating opioid receptors, most importantly the mu-opioid receptor (See Opioids). However, opioids also activate specific TLRs such as TLR-4 which leads to the release of inflammatory modulators including tumor necrosis factor (TNF-α) and interleukin-1 (Il-1). Constant low-level release of these modulators is thought to reduce the effectiveness of opioids for pain with time and to be involved in both the development of opioid analgesic tolerance and in the emergence of opioid-induced hypersensitivity to pain (OIH).
Morphine‐3‐glucuronide (M3G), a liver metabolite (breakdown product) of morphine, increases neuronal excitability via Toll‐like
receptors (TLR). Morphine activation of TLR4, concentrated in spinal glial cells, causes the release of inflammatory proteins Il‐1 and TNF‐α that result in neuroinflammation and increased pain. It is believed that M3G is a significant contributor to the side effects of morphine and that individual variants, genetic-based or otherwise, lead to greater M3G levels in some patients causing greater intolerance of morphine. This can be especially true in patients with compromised renal function which leads to reduced elimination of M3G and greater symptoms of toxicity.
Opioid Antagonists
Opioid antagonists that have the opposite effect of opioids by blocking the activity of opioids are now being explored for new applications in pain management. Certain opioid antagonists (actually reverse agonists), including naloxone and naltrexone, not only function to block opioid activity at opioid receptors but they also block or antagonize activity at the TLR-4 receptors as well. This is believed to reduce the neuroinflammation triggered by TLR-4 and may be of benefit in the treatment of the neuropathic pain conditions described above. In fact, there is a growing body of research suggesting that low dose naltrexone (LDN) may be effective for fibromyalgia and other conditions associated with central sensitivity.
See: Low- & Ultra Low-Dose Naltrexone for Pain (coming soon)
Due to their antagonizing activity with opioids, opioid antagonists ordinarily cannot be given simultaneously with opioids unless at very low doses (<1 mg). However, research has shown that naloxone and naltrexone both exist as enantiomers which are left- and right-handed versions that are molecular mirror images of one another much like a left or right handed glove. While typically medications are manufactured as combinations of both left- and right enatiomers in equal distributions, it is possible to isolate the left- from the right- enantiomer. Chemically identical but structurally different, the right (dextro) version of naltrexone antagonizes activity of TLR-4 but has no affinity for, and does not affect, opioid receptors. Thus, the dextro-enantiomer of naltrexone may be effective in treating pain by blocking TLR-4 while not affecting the opioid receptors, thereby avoiding adverse effects associated with blocking the opioid receptors. This discovery represents a potentially useful breakthru in the management of neuropathic pain and related syndromes.
Other Microglial Inhibitors
Some research suggests that minocycline, an antibiotic, may inhibit microglial activity by mechanims unrelated to antibiotic activity, possibly at the TLR-4 receptor. Animal studies have shown that minocycline inhibits heat-related hyperalgesia.
See:
Palmitoylethanolamide (PEA)
Minocycline (coming soon)
Reference Articles:
TLR-4 Antagonists – Overviews
Toll-Like Receptors in Chronic Pain – 2012
TLR-4 Antagonists – Naltrexone
TLR-4 Antagonists – Ultra Low Dose Naltrexone
- Ultra Low Dose Naltrexone – For Lower Opiate Tolerance – Research Summary – Khemcorp –
- Solutions for Autism, Social Anxiety, ADHD and Drug Tolerance
- Ultra-low-dose naltrexone suppresses rewarding effects of opiates and aversive effects of opiate withdrawal in rats. – PubMed – NCBI
- Ultra-low-dose opioid antagonists enhance opioid analgesia while reducing tolerance, dependence and addictive properties
- Ultra-low dose naltrexone attenuates chronic morphine-induced gliosis in rats – 2010
- Ultra-Low Doses of Naltrexone Enhance the Antiallodynic Effect of Pregabalin or Gabapentin in Neuropathic Rats. – PubMed – NCBI
- Ultra-Low-Dose Naloxone or Naltrexone to Improve Opioid Analgesia – The History, the Mystery and a Novel Approach – 2010
- Ultra-low-dose opioid antagonists enhance opioid analgesia while reducing tolerance, dependence and addictive properties – 2005
TLR-4 Antagonists – Minocycline
- Minocycline blocks lipopolysaccharide induced hyperalgesia by suppression of microglia but not astrocytes – 2015
- Minocycline, a microglial inhibitor, blocks spinal CCL2-induced heat hyperalgesia and augmentation of glutamatergic transmission in substantia gelatinosa neurons – 2014
TLR-4 Antagonists – Interstitial Cystitis & Systemic Inflammation
- Inflammation and Inflammatory Control in Interstitial Cystitis: Bladder Pain Syndrome – Associations with Painful Symptoms – 2014
- Inflammation and Symptom Change in Interstitial Cystitis: Bladder Pain Syndrome – A Multidisciplinary Approach to the Study of Chronic Pelvic Pain Research Network Study – 2016
- Toll-like Receptor 4 and Comorbid Pain in Interstitial Cystitis: Bladder Pain Syndrome – A Multidisciplinary Approach to the Study of Chronic Pelvic Pain Research Network Study – 2015
- Inflammation and central pain sensitization in Interstitial Cystitis:Bladder Pain Syndrome – 2015
- Toll-like Receptor 4 Mediates Morphine-Induced Neuroinflammation and Tolerance via Soluble Tumor Necrosis Factor Signaling – 2017
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.
