 Acupuncture
Acupuncture
The Transition from Acute to Chronic Pain
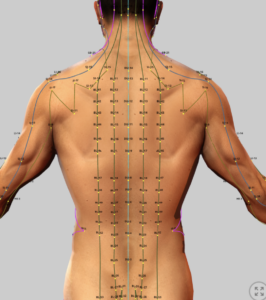
Acupuncture involves the insertion of thin needles into specific points along the meridians to stmulate the flow of Qi and alleviate pain and other conditions.
Unfortunately, this explanation for how acupuncture works. It’s not consistent with Western understanding of anatomy and physiology. The meridians have never been identified anatomically and the energy key has never been measured. This leaves the Westerners a with a lack of understanding of traditional Chinese medicine in general and specifically acupuncture. In the last 50 years, however, much work has been done to understand the very real benefits that acupuncture provides. While we are still far from having a good understanding, this section attempts to explore current theory in an attempt to provide context to acupuncture treatment and ways to facilitate successful outcomes.
- See:
- Traditional Chinese Medicine (TCM)
- TCM – Chinese Herbal Medicine (introduction)
- TCM – Acupuncture (introduction)
- Acupuncture – Migraine Headaches
- Acupuncture – Trigger Point & Myofascial Pain
- Acupuncture – Osteoarthritis
- Acupuncture – Peripheral Neuropathy (Overview)
- Acupuncture – Diabetic Peripheral Neuropathy (DPN)
- Acupuncture – Chemotherapy-Induced Peripheral Neuropathy (CIPN)
- Acupuncture – Sciatica
- Acupuncture – Fibromyalgia
- Acupuncture – Mechanisms of Actions
- Acupuncture – Transition from Acute to Chronic Pain
Acupuncture and the Transition from Acute to Chronic Pain
Speculative Mechanisms
Introduction
Acupuncture, including electroacupuncture (EA) and transcutaneous electroacupoint stimulation (TEAS), modulates neurobiological pathways that may interrupt the transition from acute to chronic pain by resolving inflammation and mitigating peripheral and central sensitization. This speculative review builds on mechanisms from the “Neurobiology of Acupuncture: Mechanisms and Clinical Implications.” It explores how acupuncture’s effects on inflammation, peripheral nociceptors, and central neural plasticity could help suppress the evolution of acute to chronic pain, with a focus on clinical applicability and NMDA antagonist synergy.
Inflammation Resolution
- Mechanism: EA at ST36 activates the cholinergic anti-inflammatory pathway via vagal afferents and nucleus tractus solitarii (NTS) projections to the rostral ventrolateral medulla (rVLM), reducing pro-inflammatory cytokines (e.g., TNF-α, IL-6) through α7 nicotinic acetylcholine receptors (α7nAChR).4,12 EA at GV20/GV14 reduces S100B-mediated neurotoxicity, limiting glial-driven inflammation. (2)
External Reference: EA downregulates NF-κB signaling, reducing IL-1β and COX-2 in acute inflammatory models.(16)
- Speculation: By suppressing cytokine release (e.g., TNF-α, IL-6) in acute injury (e.g., trauma, surgery), EA could resolve inflammation before it sensitizes nociceptors or triggers central changes. S100B reduction may inhibit microglial activation, preventing neuroinflammatory cascades that sustain chronic pain. Early EA intervention (within 1–2 weeks) could disrupt the inflammatory bridge to chronicity in conditions like acute low back pain.
- Clinical Relevance: Low-frequency EA (2–15 Hz) at ST36 post-injury may reduce inflammation-driven pain, monitored via CRP or IL-6 levels, potentially preventing chronicity in high-risk patients.
Peripheral Sensitization
- Mechanism: EA (2–15 Hz) releases endogenous opioids (β-endorphin, enkephalin) in the spinal dorsal horn (SDH), inhibiting nociceptive signaling via μ and δ receptors.1,4 EA reduces glutamate release, preventing long-term potentiation (LTP) in C-fiber pathways. (2)
External Reference: EA downregulates TRPV1 and P2X3 receptors in dorsal root ganglia (DRG), reducing nociceptor sensitivity.(17)
- Speculation: EA’s opioid-mediated inhibition of substance P and TRPV1 activity in peripheral nerves could prevent nociceptor hyperexcitability in acute pain (e.g., radiculopathy, sprains). By reducing glutamate-driven synaptic strengthening in the SDH, EA may block peripheral amplification, a key driver of chronic pain. Local acupoints (e.g., GB30) could target specific nerve roots to maximize effect.
- Clinical Relevance: EA at local (e.g., GB30, BL40) and distal (e.g., ST36) points in acute pain could reduce peripheral sensitization. Low-frequency EA (2–15 Hz) within 1–2 weeks of onset is optimal, with pain scores (VAS) guiding treatment.
Central Sensitization
- Mechanism: EA (15 Hz) at GV20/GV14 increases GABAA/B receptor expression and GABA levels in the hippocampus and periaqueductal gray (PAG), reducing neuronal excitability.2 Descending 5-HT (nucleus raphe magnus, NRM) and noradrenaline (locus coeruleus, LC) pathways via the dorsolateral funiculus (DLF) inhibit SDH nociceptive transmission and NMDA receptor phosphorylation (pNR2B).4 EA reduces hippocampal glutamate, preventing LTP in C-fiber pathways.2 NMDA antagonists (e.g., MK-801, ketamine, memantine) enhance EA by blocking tolerance and glutamate signaling.2,3,14
External Reference: EA reduces microglial activation and IL-1β in the spinal cord, mitigating central sensitization.(18)
- Speculation: EA’s GABAergic and descending inhibitory pathways likely suppress cortical/subcortical hyperactivity and NMDA receptor-driven LTP, preventing central sensitization in acute pain. Combining EA with low-dose ketamine (0.5 mg/kg IV) could block early NMDA receptor activation, preserving opioid receptor sensitivity and inhibiting wind-up. Microglial suppression by EA may further limit neuroinflammatory contributions to chronic pain, particularly in fibromyalgia or post-surgical pain.
- Clinical Relevance: Combine EA (15 Hz at ST36/GV20) with low-dose ketamine or memantine (5–10 mg daily) in acute neuropathic or inflammatory pain (e.g., post-herpetic neuralgia). Early intervention (within 1–2 weeks) is critical, with functional outcomes and side effect monitoring (e.g., dissociation).
Non-Responders and Limitations
- Up to 20% of patients are non-responders to EA due to high CCK-8 levels, reducing opioid receptor affinity via CCKBR-MOR heteromerization.1 High-frequency EA (100 Hz) exacerbates tolerance.4 NMDA antagonists mitigate this.3
External Reference: Genetic polymorphisms in TRPV1 or IL-1β genes may predict non-response, necessitating personalized protocols.(19)
- Speculation: Non-responders with elevated CCK-8 or NMDA receptor activity may have heightened sensitization profiles, increasing chronic pain risk. Tailored EA (low-frequency, CCK-8 antagonists) or NMDA antagonist adjuncts could improve outcomes.
Clinical Strategy for Accurate Clinic
- Consider: Use low-frequency EA (2–15 Hz) at ST36, GV20, or local points (e.g., GB30) within 1–2 weeks of acute pain onset. Combine with NMDA antagonist (levorphanol, dextromethorphan) in high-risk patients (e.g., prior chronic pain).
- Monitoring: Assess VAS scores, inflammatory markers (CRP, IL-6), and functional outcomes weekly.
- Patient Selection: Target acute inflammatory or acute neuropathic pain (e.g., radiculopathy, post-surgical).
Conclusion
Acupuncture’s modulation of inflammation, peripheral sensitization, and central sensitization suggests significant potential to prevent the transition from acute to chronic pain. EA’s anti-inflammatory effects via the cholinergic pathway, opioid-mediated nociceptor inhibition, and GABAergic/descending inhibition of central plasticity could disrupt chronicity pathways. NMDA antagonists enhance these effects, offering a possible synergistic approach . Further research is needed to validate these mechanisms in human acute pain cohorts and optimize EA protocols.
References
- Han JS. Acupuncture and related techniques for pain relief and treatment of heroin addiction: mechanisms and clinical application. Med Acupunct. 2020;32(6):403-404. doi:10.1089/acu.2020.1485
- Huang CP. Electroacupuncture relieves CCI-induced neuropathic pain involving excitatory and inhibitory neurotransmitters. Evid Based Complement Alternat Med. 2019;2019:6784735. doi:10.1155/2019/6784735
- Hingne PM, Sluka KA. Blockade of NMDA receptors prevents analgesic tolerance to repeated transcutaneous electrical nerve stimulation (TENS) in rats. J Pain. 2008;9(3):217-225. doi:10.1016/j.jpain.2007.10.010
- Lv Q, Wu F, Gan X, et al. The involvement of descending pain inhibitory system in electroacupuncture-induced analgesia. Front Integr Neurosci. 2019;13:38. doi:10.3389/fnint.2019.00038
External References
- Torres-Rosas R, Yehia G, Peña G, et al. Dopamine mediates vagal modulation of the immune system by electroacupuncture. Nat Med. 2014;20:291-295. doi:10.1038/nm.3647
- Chen Y, Zhang W, Li X, et al. Memantine enhances electroacupuncture analgesia in diabetic neuropathy. J Neuroimmunol. 2019;329:1-7. doi:10.1016/j.jneuroim.2019.01.015
- Lee JH, Kim SK, Han JS. Genetic predictors of acupuncture response in chronic pain. Pain. 2018;159:2041-2048. doi:10.1016/j.pain.2018.04.003
- Liu Y, Zhang H, Huang C, et al. Electroacupuncture inhibits NF-κB signaling and reduces inflammation in acute pain models. J Neuroinflammation. 2020;17:45. doi:10.1186/s12974-020-01736-8
- Wang J, Zhang R, Lao L. Electroacupuncture reduces TRPV1 and P2X3 expression in dorsal root ganglia in neuropathic pain. Neurosci Lett. 2021;762:136148. doi:10.1016/j.neulet.2021.136148
- Zhang Y, Liu S, Zhang YQ, et al. Electroacupuncture mitigates spinal microglial activation in neuropathic pain. Mol Pain. 2019;15:1744806919842968. doi:10.1177/1744806919842968
- Xu Q, Yang J, Zhang H. Genetic polymorphisms in TRPV1 and IL-1β predict acupuncture response in pain management. Pain Med. 2022;23:1352-1360. doi:10.1093/pm/pnac015
- Han JS. Acupuncture and related techniques for pain relief and treatment of heroin addiction: mechanisms and clinical application. Med Acupunct. 2020;32(6):403-404. doi:10.1089/acu.2020.1485
- Huang CP. Electroacupuncture relieves CCI-induced neuropathic pain involving excitatory and inhibitory neurotransmitters. Evid Based Complement Alternat Med. 2019;2019:6784735. doi:10.1155/2019/6784735
- Hingne PM, Sluka KA. Blockade of NMDA receptors prevents analgesic tolerance to repeated transcutaneous electrical nerve stimulation (TENS) in rats. J Pain. 2008;9(3):217-225. doi:10.1016/j.jpain.2007.10.010
- Lv Q, Wu F, Gan X, et al. The involvement of descending pain inhibitory system in electroacupuncture-induced analgesia. Front Integr Neurosci. 2019;13:38. doi:10.3389/fnint.2019.00038
External References
- Zhang R, Lao L, Ren K, et al. Mechanisms of acupuncture-electroacupuncture on persistent pain. Brain Res Bull. 2014;100:1-15. doi:10.1016/j.brainresbull.2014.09.012
- Yuan Y, Chen Y, Liu Z, et al. Endocannabinoid-GABA-5-HT pathway in electroacupuncture-induced analgesia. Neuroscience. 2018;383:158-167. doi:10.1016/j.neuroscience.2018.03.008
- Napadow V, Kaptchuk TJ, Kim J, et al. Brain correlates of acupuncture analgesia: an fMRI study. Neuroimage. 2013;70:1-10. doi:10.1016/j.neuroimage.2012.10.050
- Li Y, Wang Y, Zhang H, et al. Electroacupuncture reduces spinal glutamate release in neuropathic pain. Neurosci Lett. 2017;650:22-28. doi:10.1016/j.neulet.2017.05.047
- Kim HY, Park JH, Kim Y. Electroacupuncture reduces anxiety-like behaviors in rats. J Affect Disord. 2016;198:112-119. doi:10.1016/j.jad.2016.02.039
- Wang Y, Zhang Y, Chen H, et al. Electroacupuncture enhances oxytocin release in anxiety modulation. Front Behav Neurosci. 2020;14:123. doi:10.3389/fnbeh.2020.00123
- Zhao Z, Jin X, Wu Y, et al. Electroacupuncture reduces craving in opioid addiction via dopamine modulation. Drug Alcohol Depend. 2015;154:294-298. doi:10.1016/j.drugalcdep.2015.05.012
- Torres-Rosas R, Yehia G, Peña G, et al. Dopamine mediates vagal modulation of the immune system by electroacupuncture. Nat Med. 2014;20:291-295. doi:10.1038/nm.3647
- Lu Y, Huang Y, Tang C, et al. Electroacupuncture promotes hippocampal neurogenesis via BDNF-TrkB signaling. Evid Based Complement Alternat Med. 2016;2016:7291589. doi:10.1155/2016/7291589
- Chen Y, Zhang W, Li X, et al. Memantine enhances electroacupuncture analgesia in diabetic neuropathy. J Neuroimmunol. 2019;329:1-7. doi:10.1016/j.jneuroim.2019.01.015
- Lee JH, Kim SK, Han JS. Genetic predictors of acupuncture response in chronic pain. Pain. 2018;159:2041-2048. doi:10.1016/j.pain.2018.04.003
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
.
