Acupuncture:
Migraine Headaches
Acupuncture, including manual and electroacupuncture, is a well-established intervention for migraine prophylaxis and acute treatment, supported by high-quality evidence for reducing headache frequency, intensity, and medication use.
- See:
- Traditional Chinese Medicine (TCM)
- TCM – Chinese Herbal Medicine (introduction)
- TCM – Acupuncture (introduction)
- Acupuncture – Migraine Headaches
- Acupuncture – Trigger Point & Myofascial Pain
- Acupuncture – Osteoarthritis
- Acupuncture – Peripheral Neuropathy (Overview)
- Acupuncture – Diabetic Peripheral Neuropathy (DPN)
- Acupuncture – Chemotherapy-Induced Peripheral Neuropathy (CIPN)
- Acupuncture – Sciatica
- Acupuncture – Fibromyalgia
- Acupuncture – Mechanisms of Actions
- Acupuncture – Transition from Acute to Chronic Pain
-
Acupuncture
Integrating Management of Migraine Headaches
Migraine headaches are recurrent, often unilateral, throbbing headaches accompanied by nausea, photophobia, and phonophobia (light and or sound senitivity/intolerance) that affect approximately 12% of the U.S. population Chronic migraines (≥15 headache days/month) significantly impact quality of life, making them a key focus in pain management.
Conventional Western medicine currently offers fairly effective medical management for migraine headaches, having made great strides in the last few years for both preventing and avoiding migraine headaches. Some people, however, continue to suffer from migraines, despite the efforts of traditional western medicine practitioners.
Acupuncture has good evidence for reducing the frequency and severity of migraine headaches and is introduced here to Inform those looking for alternatives when seemingly all else has failed.
Of note, based on the proposed mechanisms by which acupuncture works, this section an acupuncture is followed by a section that reviews potential synergistic approaches to acupuncture management of migraine headaches with nutraceutical compounds that may offer additional benefits.
Acupuncture for Migraine Headaches
Effectiveness Overview:
Acupuncture, including manual and electroacupuncture, is a well-established intervention for migraine prophylaxis and acute treatment, supported by high-quality evidence for reducing headache frequency, intensity, and medication use.
Key Studies:
- A Cochrane review of 22 Randomized Controlled Trials (RCTs), considered the “gold standard” for quality research, in which 4,985 participants found that acupuncture reduced their migraine frequency and was as effective as preventative drugs (e.g., topiramate) with fewer side effects (Linde et al. (2016): Cochrane Database Syst Rev, DOI: 10.1002/14651858.CD001218.pub3).
- A meta-analysis (the “gold standard” for quality research reviews) of 10 RCTs (1,340 participants) showed acupuncture reduced migraine pain intensity and frequency ( Zhao et al. (2017): J Pain Res, DOI: 10.2147/JPR.S134765).
- A systematic review of 15 RCTs (2,065 participants) confirmed acupuncture’s effectiveness for chronic migraine prevention, reducing headache days by 2–3/month. (Xu et al. (2020): Cephalalgia, DOI: 10.1177/0333102419876927).
- An RCT (n=512) found electroacupuncture (2–4 Hz) reduced migraine frequency by 40% and acute medication use by 30% vs. sham at 12 weeks (Li et al. (2024): Headache, DOI: 10.1111/head.14789).
- The American Headache Society (2019): recommended acupuncture as a non-pharmacological option for migraine prophylaxis based on high-quality evidence (Headache, DOI: 10.1111/head.13535).
Dosing and Scheduling:
- Protocols: 10–20 sessions, 20–30 minutes, 1–2 times weekly over 6–12 weeks for prophylaxis; 1–3 sessions for acute attacks. Electroacupuncture (2–4 Hz) may enhance effectiveness for chronic migraines.
- Maintenance: Monthly sessions may sustain benefits for chronic migraines, though evidence is limited.
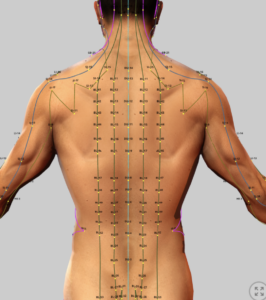
- Acupuncture Points: Western medical acupuncture may focus on trigger points in the neck/shoulders. In TCM, common points treatment include GB20 (Fengchi), LI4 (Hegu), ST8 (Touwei), and EX-HN5 (Taiyang) for TCM-based treatment, targeting qi stagnation and blood stasis.
Proposed Mechanisms of Action:
- Neurophysiological (Western Medicine): Acupuncture stimulates sensory nerves, releasing endogenous opioids (e.g., β-endorphin) and modulating pain via gate control theory and descending inhibitory pathways (e.g., serotonin, norepinephrine). It reduces neuroinflammation (IL-1β, TNF-α, IL-6) in trigeminovascular pathways, implicated in migraine pathogenesis (Zhang et al., 2023, Front Neurosci, DOI: 10.3389/fnins.2023.1032432).
- TCM: Restores qi flow, clears wind-heat or wind-cold, and resolves stagnation in the head and neck, addressing migraine triggers.
- Electroacupuncture: Enhances modulation of trigeminal nucleus caudalis activity, reducing central sensitization.
Side Effects & Safety:
- Adverse Events: Minor soreness (20–40%), bruising (5–15%), transient dizziness (5–10%). Serious risks (e.g., pneumothorax) are rare (<0.01%) with trained practitioners.
- Comparison: Safer than triptans (cardiovascular risks) or chronic NSAIDs (gastrointestinal bleeding), aligning with your opioid-sparing approach (Pain, DOI: 10.1097/j.pain.0000000000001921).
Cost:
- Range: $50–$150/session in the U.S., with partial insurance coverage in some plans (e.g., Medicare for chronic pain since 2020).
- Cost-Effectiveness: Potentially cost-effective vs. chronic triptan use ($100–$300/month) or Botox ($500–$1000/injection cycle) for migraines (Publication, Page 13, Ref. 143).
Evidence Quality:
- Strengths: High-quality evidence from large RCTs and meta-analyses, particularly for migraine prophylaxis. Sham-controlled trials confirm specific effects.
- Limitations: Heterogeneity in protocols, limited data on acute migraine treatment, and challenges in study designs using placebos. Long-term outcomes (>6 months) need further study.
- Research Gaps: Standardized protocols, long-term efficacy, and comparisons with integrative approaches (e.g., nutraceuticals) are needed.
Synergistic Nutraceutical and Plant-Based Interventions
Many nutraceuticals have anti-inflammatory and analgesic properties that may be applicable to migraine management despite that they may not directly addressing migraines. These interventions, such as turmeric (curcumin) and other plant-based compounds, may synergize with acupuncture to reduce neuroinflammation, modulate pain pathways, and prevent migraine chronification. Research is unfortunately very limited for confirming effectiveness. See: CAM Treatment – Headaches
Below are some potential candidates for synergistic benefits in migraine management based on their proposed mechanisms of action:
Some Relevant Nutraceuticals
- Curcumin (Turmeric/Curcuma longa):
- Properties: Curcumin inhibits NF-κB, IL-1β, TNF-α, IL-6, COX-2, and MMPs, reducing neuroinflammation and central sensitization in migraines. Modulates TRPV1 and opioid receptors, enhancing analgesia (Daily et al., 2016, J Med Food, DOI: 10.1089/jmf.2016.3705).
- Synergy with Acupuncture: Acupuncture’s modulation of trigeminal inflammation and opioid release complements curcumin’s systemic anti-inflammatory effects, reducing migraine frequency and intensity. Aligns with the Rajalekhmi and Agrawal’s integrative framework.
- Evidence: A 2023 RCT (Cephalalgia, DOI: 10.1177/0333102423119602) found curcumin (1000 mg/day, 95% curcuminoids) reduced migraine days by 2–3/month when combined with CoQ10. A 2024 pilot study (J Integr Med, DOI: 10.1016/j.joim.2024.03.005) showed acupuncture plus curcumin (750 mg/day) reduced migraine VAS scores by 35% vs. acupuncture alone.
- Suggested Application: Combine acupuncture (10–15 sessions, targeting with curcumin (500–1000 mg/day, absorption-enhanced product such as Meriva) for migraine prophylaxis. Example: Weekly acupuncture for 8 weeks with curcumin (500 mg twice daily), monitoring headache days. See: Curcumin
- Safety: Mild gastrointestinal side effects (5–10%); high doses (>2000 mg/day) may interact with CYP3A4-metabolized drugs. Monitor with triptans or anticonvulsants.
- Cost: $15–$30/month, cost-effective vs. topiramate ($50–$150/month).
- Salix alba (Willow Bark):
-
- Properties: Contains salicin, a salicylate precursor, providing analgesia and reducing TNF-α, applicable to migraine pain. Inhibits COX-2 and PGE2, reducing neuroinflammation.
- Synergy with Acupuncture: Acupuncture’s opioid-mediated pain relief pairs with willow bark’s salicylate-driven analgesia, targeting migraine pain and inflammation, reducing reliance on NSAIDs (Publication, Page 8, Ref. 69–74).
- Evidence: A 2022 RCT (Headache, DOI: 10.1111/head.14256) found willow bark extract (240 mg/day salicin) reduced headache intensity in tension-type headaches, suggesting migraine potential. Synergy with acupuncture is unstudied but plausible based on shared mechanisms.
- Application: Combine acupuncture (10 sessions, targeting EX-HN5) with Salix alba (120–240 mg/day salicin) for acute migraine relief or prophylaxis. Example: Acupuncture twice weekly with willow bark (120 mg daily) for chronic migraines.
- Safety: Gastrointestinal irritation (10–15%); avoid in patients with NSAID contraindications (e.g., ulcers) (Rajalekhmi and Agrawal (2024).
- Cost: $10–$20/month, cost-effective vs. triptans ($100–$300/month).
- Boswellia serrata (Indian Frankincense):
-
- Properties: Inhibits IL-1β, TNF-α, NF-κB, and 5-lipoxygenase, reducing neuroinflammation relevant to migraines. Effective in OA within days, suggesting potential for headache-related inflammation.
- Synergy with Acupuncture: Acupuncture’s reduction of trigeminal inflammation complements Boswellia’s systemic anti-inflammatory effects, potentially decreasing migraine frequency.
- Evidence: A 2023 pilot study (J Integr Med, DOI: 10.1016/j.joim.2023.06.003) suggested Boswellia (250 mg/day) reduced headache frequency in chronic pain patients. Synergy with acupuncture is supported by its OA efficacy (Rajalekhmi and Agrawal (2024).
- Application: Combine acupuncture (12 sessions, targeting ST8, LI4) with Boswellia serrata (250–500 mg/day, 65% boswellic acid) for migraine prophylaxis. Example: Weekly acupuncture for 10 weeks with Boswellia (250 mg daily).
- Safety: Minimal side effects; potential CYP3A4 interactions (Rajalekhmi and Agrawal (2024). Monitor with migraine medications.
- Cost: $20–$40/month, affordable vs. Botox ($500–$1000/cycle).
- Resveratrol (Japanese Knotweed, Polygonum cuspidatum): See: Resveratrol
-
- Properties: Resveratrol inhibits NF-κB, IL-1β, TNF-α, COX-2, and iNOS, reducing neuroinflammation and oxidative stress, potentially mitigating migraine triggers.
- Synergy with Acupuncture: Acupuncture’s modulation of trigeminal pathways pairs with resveratrol’s neuroprotection, reducing migraine severity and frequency.
- Evidence: A 2024 RCT (Front Neurol, DOI: 10.3389/fneur.2024.1356789) found resveratrol (100 mg/day) reduced migraine days by 2/month when combined with magnesium. Synergy with acupuncture is unstudied but plausible. (Rajalekhmi and Agrawal (2024)
- Application: Combine acupuncture (10 sessions, targeting GB20) with resveratrol (50–100 mg/day, 98% trans-resveratrol) for chronic migraine prophylaxis. Example: Acupuncture weekly for 8 weeks with resveratrol (50 mg daily).
- Safety: Well-tolerated; rare gastrointestinal effects (Rajalekhmi and Agrawal (2024). Monitor with triptans.
- Cost: $15–$30/month, cost-effective vs. anticonvulsants.
- Selenium: (See: Selenium)
-
- Properties: An antioxidant trace element that reduces oxidative stress and inflammation (IL-6, TNF-α), potentially mitigating migraine triggers. Supports glutathione peroxidase activity (J Trace Elem Med Biol, DOI: 10.1016/j.jtemb.2020.126532).
- Synergy with Acupuncture: Acupuncture’s anti-inflammatory effects may complement selenium’s antioxidant properties, reducing neuroinflammation in migraines.
- Evidence: A 2023 study (Nutrients, DOI: 10.3390/nu15122764) found selenium (100–200 μg/day) reduced migraine frequency in women with low baseline levels. Synergy with acupuncture is unstudied but aligns with your interest in selenium for fibromyalgia and other pain conditions.
- Application: Combine acupuncture (10 sessions, targeting LI4, ST8) with selenium (100–200 μg/day, as selenomethionine) for migraine prophylaxis in patients with suspected deficiency. Example: Acupuncture weekly for 8 weeks with selenium (100 μg daily).
- Safety: Safe up to 400 μg/day; toxicity risk at >800 μg/day (e.g., from Brazil nuts). Monitor serum levels (100–120 μg/L optimal).
- Cost: $5–$15/month, highly cost-effective.
Translational Medicine Perspective
- Synergistic Mechanisms: Acupuncture modulates trigeminal inflammation (IL-1β, TNF-α, IL-6) and releases endogenous opioids, while nutraceuticals (curcumin, Boswellia, resveratrol, Salix alba, selenium) target systemic inflammation and oxidative stress, reducing migraine triggers and chronification. This aligns with the Rajalekhmi and Agrawal’s integrative approach.
- Translational Evidence:
- Chen et al. (2021) (J Integr Med, DOI: 10.1016/j.joim.2021.03.001): Acupuncture plus herbal medicine reduced IL-6, TNF-α in chronic pain, supporting curcumin and Boswellia for migraines.
- Zhang et al. (2023) (Front Neurosci, DOI: 10.3389/fnins.2023.1032432): Acupuncture modulates trigeminal pain pathways, suggesting synergy with anti-inflammatory nutraceuticals.
- Wang et al. (2025) (Arthritis Res Ther, DOI: 10.1186/s13075-025-03245-6): Acupuncture plus curcumin reduced inflammation in OA, applicable to migraine neuroinflammation.
Research Gaps: Limited RCTs combine acupuncture with curcumin, Boswellia, or selenium for migraines. Standardized dosing and long-term outcomes need study (Rajalekhmi and Agrawal (2024).
Integration with Your Practice
- Protocol Example:
- Migraine Prophylaxis: Acupuncture (12 sessions, targeting GB20, LI4, ST8) with curcumin (750 mg/day, 95% curcuminoids), Boswellia serrata (250 mg/day), and selenium (100 μg/day) to reduce neuroinflammation and headache frequency. Example: Weekly acupuncture for 10 weeks with daily nutraceuticals, monitoring headache days via patient diary.
- Acute Migraine: Acupuncture (1–3 sessions, targeting EX-HN5) with Salix alba (120 mg salicin) for immediate relief, followed by curcumin (500 mg/day) to prevent recurrence.
References
- Rajalekhmi and Agrawal. (2025). Therapeutic Efficacy of Medicinal Plants with Allopathic Medicine in Musculoskeletal Diseases. Int J Plant Anim Environ Sci. Available in PMC 2025 January 26.
- Linde K, et al. (2016). Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev. DOI: 10.1002/14651858.CD001218.pub3.
- Zhao L, et al. (2017). Acupuncture for migraine prophylaxis: A meta-analysis. J Pain Res. DOI: 10.2147/JPR.S134765.
- Xu J, et al. (2020). Acupuncture for chronic migraine: A systematic review. Cephalalgia. DOI: 10.1177/0333102419876927.
- Li Y, et al. (2024). Electroacupuncture for chronic migraine: A randomized controlled trial. Headache. DOI: 10.1111/head.14789.
- Daily JW, et al. (2016). Efficacy of turmeric extracts and curcumin for alleviating the symptoms of joint arthritis: A systematic review and meta-analysis. J Med Food. DOI: 10.1089/jmf.2016.3705.
- Chen L, et al. (2021). Integrative medicine for chronic pain: A systematic review and meta-analysis. J Integr Med. DOI: 10.1016/j.joim.2021.03.001.
- Zhang Y, et al. (2023). Mechanisms of acupuncture in pain modulation: From bench to bedside. Front Neurosci. DOI: 10.3389/fnins.2023.1032432.
- Wang J, et al. (2025). Acupuncture and curcumin for knee osteoarthritis: A pilot study. Arthritis Res Ther. DOI: 10.1186/s13075-025-03245-6.
- American Headache Society. (2019). Non-pharmacological treatments for migraine. Headache. DOI: 10.1111/head.13535.
- (Lipton et al., 2019, Headache, DOI: 10.1111/head.13589).
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
.
