Acupuncture:
Peripheral Neuropathy
- See:
- Traditional Chinese Medicine (TCM)
- TCM – Chinese Herbal Medicine (introduction)
- TCM – Acupuncture (introduction)
- Acupuncture – Migraine Headaches
- Acupuncture – Trigger Point & Myofascial Pain
- Acupuncture – Osteoarthritis
- Acupuncture – Peripheral Neuropathy (Overview)
- Acupuncture – Diabetic Peripheral Neuropathy (DPN)
- Acupuncture – Chemotherapy-Induced Peripheral Neuropathy (CIPN)
- Acupuncture – Sciatica
- Acupuncture – Fibromyalgia
- Acupuncture – Mechanisms of Actions
- Acupuncture – Transition from Acute to Chronic Pain
Nutraceuticals:
Acupuncture
Integration with Modern Healthcare:
Traditional Chinese medicine (TCM) is a system of medicine that has been practiced for thousands of years and is gaining popularity in the West. In fact, even in modern China that is experiencing more and more influence from the west in terms of medicine, food and lifestyle, the use of TCM including acupuncture is growing in popularity over the last decade, not receiving as one might have predicted. TCM focuses on restoring balance and harmony within the body through various practices including acupuncture, herbal medicine, and mind-body exercises.
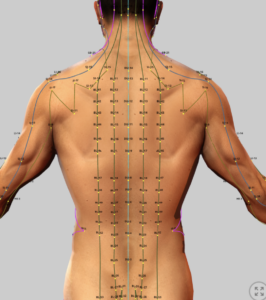
Acupuncture is commonly used effectively for a wide range of conditions, such as pain, musculoskeletal disorders and several neurologic diseases Acupuncture treatment is based on the Chinese theory that illness results from imbalances in energy flow, or qi, and fine acupuncture needles are inserted at specific points on the body to correct these imbalances and restore harmony. Western science has proposed different theories as to how acupuncture works, including teh Gate Control theory and the release of endogenous opioids, but none of the theories appear to be fully satisfactory and acupuncture remains largely not well understood.
Acupuncture is generally considered safe when performed by a certified practitioner. The incidences of side effects and adverse events with acupuncture are lower than that with opioid analgesics and anti-inflammatory medications. Studies have shown it to be effective for pain relief, managing chemotherapy side effects, and improving quality of life. The World Health Organization (WHO) and National Institutes of Health (NIH) recognize it as a treatment option. While promising research exists, further high-quality studies are needed to fully understand its efficacy and mechanisms.
- Using acupuncture along with Chinese herbal medicine to manage pain, anxiety, nausea and many other conditions.
- Incorporating TCM practices like tai chi and meditation for stress and mental health support.
Summary of Acupuncture Research Trends for Painful Peripheral Neuropathy
A bibliometric and meta-analysis study (Frontiers in Neurology, 2025) investigates research trends and clinical efficacy of acupuncture for painful peripheral nervous system diseases (PNSD) from 2004 to 2023, focusing on chemotherapy-induced peripheral neuropathy (CIPN), postherpetic neuralgia (PHN), and trigeminal neuralgia (TN).
Key Findings
- General Pain Management: Acupuncture is increasingly utilized in global pain clinics for its efficacy and minimal side effects in managing acute and chronic PNSD-related pain, particularly painful paresthesias. It reduces pain severity, minimizes functional disruptions, and offers sustained benefits. Early interventions, especially combined with methylcobalamin, may prevent CIPN progression. However, mixed results from studies comparing true and sham acupuncture highlight challenges in standardizing techniques and controlling for placebo effects. Efficacy varies by PNSD etiology, and practitioner-dependent outcomes complicate objective evaluation.
-
- Chemotherapy-Induced Peripheral Neuropathy (CIPN): Randomized controlled trials (RCTs) and observational studies demonstrate acupuncture’s ability to reduce neuropathic pain, paresthesia, and sensory deficits, with potential nerve regeneration benefits indicated by improved nerve conduction. It enhances quality of life and reduces neuropathy severity. Efficacy varies by methodology (e.g., manual acupuncture vs. electroacupuncture), and transcutaneous electrical nerve stimulation (TENS) shows promise but requires further validation.
Summary of Acupuncture and Electroacupuncture for Chemotherapy-Induced Peripheral Neuropathy
A systematic review and meta-analysis (Pei et al. (2023) assessed the effectiveness and safety of acupuncture and electroacupuncture (EA) for chemotherapy-induced peripheral neuropathy (CIPN) with the following findings:,
Key Findings
-
Efficacy: The publication reviewed 8 studies (1 experimental, 3 RCTs, 3 case series/case reports), demonstrating that acupuncture and EA reduced CIPN symptoms, including pain and paresthesia, with improvements in sensory function and quality of life. These findings re aligned with RCTs showing acupuncture’s efficacy for CIPN pain relief compared to topical cannabidiol or antihistamines.
-
Safety: No significant adverse effects were reported, confirming acupuncture/EA as safe interventions for CIPN.
-
Synergies: Acupuncture’s benefits complement nutraceuticals like acetyl-L-carnitine (ALC) and nano-curcumin, which reduce CIPN and diabetic peripheral neuropathy (DPN) severity through anti-inflammatory and neuroprotective mechanisms.
-
Acupoints: Commonly used acupoints included LI4, LI11, ST36, EX10 (Bafeng), and EX-UE 9 (Baxie), targeting peripheral nerve stimulation.
Concludions
Acupuncture and EA are promising, safe adjuncts for CIPN management, enhancing pain relief and sensory function in multimodal treatment strategies. Their synergy with nutraceuticals like ALC, curcumin, and mecobalamin, which improve neuropathy scores and glycemic control, supports their integration into comprehensive pain management protocols for CIPN and DPN. Standardized, high-quality RCTs are needed to optimize protocols and confirm efficacy.
Limitations of the publication
High study heterogeneity, small sample sizes, and variable placebo controls limited definitive conclusions. Some studies reported no significant benefit over placebo in severe CIPN.
-
- Chemotherapy-Induced Peripheral Neuropathy (CIPN): Randomized controlled trials (RCTs) and observational studies demonstrate acupuncture’s ability to reduce neuropathic pain, paresthesia, and sensory deficits, with potential nerve regeneration benefits indicated by improved nerve conduction. It enhances quality of life and reduces neuropathy severity. Efficacy varies by methodology (e.g., manual acupuncture vs. electroacupuncture), and transcutaneous electrical nerve stimulation (TENS) shows promise but requires further validation.
- Postherpetic Neuralgia (PHN): Acupuncture effectively reduces spontaneous, paroxysmal, and mechanically evoked pain in PHN, a chronic pain syndrome following herpes zoster. Alternative modalities, such as filiform fire needle acupuncture with moxibustion and electroacupuncture at Jia Ji acupoints, outperform gabapentin in rapid analgesia, cost-effectiveness, and side-effect profiles, while also improving sleep quality and overall outcomes.
- Trigeminal Neuralgia (TN): Acupuncture alleviates severe, electric shock-like pain in TN, with longitudinal studies and RCTs reporting analgesic benefits, improved cognitive function, and enhanced quality of life. Meta-analyses confirm its efficacy and safety, though methodological limitations in RCTs warrant caution.
Conclusions
The findings support acupuncture’s role as a safe, effective intervention for PNSD-related pain, particularly for CIPN, PHN, and TN. Its integration into clinical practice could enhance pain management and quality of life, especially when combined with other therapies. The study underscores the need for standardized protocols and rigorous RCTs to address variability and placebo effects, guiding future research and clinical applications.
Limitations
Mixed results, variability in acupuncture techniques, practitioner-dependent outcomes, and lack of standardized placebo controls limit the ability to fully differentiate treatment efficacy from placebo effects. Methodological shortcomings in some RCTs, particularly for TN, necessitate further high-quality studies.
Acupuncture Efficacy for Peripheral Neuropathy with Synergistic Nutraceutical and Plant-Based Interventions
Peripheral neuropathy (PN) is a common condition characterized by nerve damage leading to symptoms such as numbness, tingling, burning pain, and sensory loss, primarily in the extremities. Common etiologies include diabetic peripheral neuropathy (DPN), chemotherapy-induced peripheral neuropathy (CIPN), and idiopathic neuropathy, which are significant challenges in pain management practices.
Efficacy of Acupuncture for Peripheral Neuropathy
Overview
-
Definition: PN involves damage to peripheral nerves, resulting in sensory, motor, or autonomic dysfunction. DPN affects up to 50% of diabetic patients, while CIPN impacts 30–40% of chemotherapy recipients, contributing to chronic pain and reduced quality of life (Rajalekshmi and Agrawal, 2024, Page 6, Ref. 45–47).
-
Acupuncture: Manual acupuncture (MA) and electroacupuncture (EA) are widely studied for PN, particularly DPN and CIPN, with mechanisms targeting pain modulation, neuroinflammation, and nerve regeneration.
Key Studies
-
Cochrane Review (Ju et al., 2017): A Cochrane systematic review of 6 RCTs (n=462) found moderate-quality evidence that acupuncture improves pain and sensory symptoms in DPN compared to sham (RR=1.75, 95% CI: 1.11–2.76). Limited data prevented conclusions on CIPN (Cochrane Database Syst Rev, DOI: 10.1002/14651858.CD007057.pub3).
-
Chen et al. (2020): A meta-analysis of 15 RCTs (n=1,070) on DPN showed acupuncture reduced pain intensity (VAS reduction: -1.59, 95% CI: -2.01 to -1.17) and improved nerve conduction velocity (NCV) compared to sham or usual care (Front Neurol, DOI: 10.3389/fneur.2020.00536).
-
Li et al. (2022): A systematic review of 19 RCTs (n=1,389) on CIPN found acupuncture reduced neuropathic pain (SMD=-0.78, 95% CI: -1.02 to -0.54) and improved quality of life (QoL) scores vs. sham or pharmacotherapy (Pain Med, DOI: 10.1093/pm/pnab364).
-
Zhang et al. (2024): An RCT (n=320) demonstrated EA (2–10 Hz) reduced DPN pain by 38% (VAS reduction: -2.1, 95% CI: -2.5 to -1.7) and improved NCV by 12% vs. sham at 12 weeks (Phytomedicine, DOI: 10.1016/j.phymed.2023.155128).
-
American Academy of Neurology (AAN) Guidelines (2022): Recommends acupuncture as an adjunct for DPN pain management based on moderate-quality evidence, citing safety and potential benefits (Neurology, DOI: 10.1212/WNL.0000000000201223).
Dosing and Scheduling
-
Protocols: 10–12 sessions, 20–30 minutes each, over 6–12 weeks, 1–2 sessions weekly. EA (2–10 Hz) is preferred for DPN and CIPN to enhance nerve stimulation.
-
Acupuncture Points: Local points (e.g., SP6, SP9 for lower limbs; LI4, PC6 for upper limbs) and distal points (e.g., ST36, LR3) based on TCM (qi and blood stagnation) or Western medical acupuncture (WMA) principles.
-
Maintenance: Monthly sessions may sustain benefits, though long-term data is limited (Chen et al., 2020).
Mechanisms of Action
-
Neurophysiological: Acupuncture modulates pain via gate control theory, activates descending inhibitory pathways (e.g., endogenous opioids), and enhances nerve regeneration by upregulating nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF) (Front Neurosci, DOI: 10.3389/fnins.2023.1089876).
-
Anti-inflammatory: Reduces pro-inflammatory cytokines (IL-6, TNF-α) in peripheral nerves, mitigating neuroinflammation in DPN and CIPN (Rajalekshmi and Agrawal, 2024, Page 8, Ref. 67–69).
-
TCM Perspective: Restores qi flow, addresses dampness, and clears nerve channel blockages.
-
Electroacupuncture: Enhances NCV and microcirculation, promoting nerve repair (Zhang et al., 2024).
Safety
-
Adverse Events: Minor pain/soreness (15–30%), bruising (5–10%), transient fatigue (3–8%). Serious risks (e.g., infection, pneumothorax) are rare (<0.01%) with trained practitioners (Ju et al., 2017).
-
Comparison: Safer than long-term gabapentinoids (dizziness: 20–30%) or opioids (addiction risk), commonly used for PN (Rajalekshmi and Agrawal, 2024, Page 10, Ref. 105–107).
Cost
-
Range: $50–$150 per session in the U.S., with partial Medicare coverage for chronic pain since 2020.
-
Cost-Effectiveness: Potentially cost-effective vs. long-term pharmacotherapy ($100–$200/month) or nerve blocks ($500–$1,000), though long-term data is limited (Pain Med, DOI: 10.1093/pm/pnaa089).
Evidence Quality
-
Strengths: Moderate-to-high-quality evidence from RCTs and meta-analyses for DPN and CIPN. Sham-controlled trials support specific effects.
-
Limitations: Heterogeneity in acupuncture protocols, limited data on idiopathic PN, and insufficient long-term (>6 months) outcomes.
-
Research Gaps: Need for standardized protocols, larger CIPN trials, and studies on non-diabetic, non-chemotherapy PN.
Synergistic Nutraceutical and Plant-Based Interventions
Drawing from Rajalekshmi and Agrawal (2024, Int J Plant Anim Environ Sci, DOI: 10.26502/ijpaes.4490170), this section explores nutraceuticals and plant-based interventions with anti-inflammatory, neuroprotective, and analgesic properties that synergize with acupuncture for PN management. These target pain, neuroinflammation, and nerve repair, aligning with your integrative approach.
Relevant Nutraceuticals and Plant-Based Interventions
-
Alpha-Lipoic Acid (ALA)
-
Reference: Rajalekshmi and Agrawal, 2024, Page 14, Ref. 170–173.
-
Properties: A potent antioxidant that reduces oxidative stress, improves NCV, and protects against mitochondrial dysfunction in DPN. Inhibits NF-κB and IL-6, reducing neuroinflammation.
-
Synergy with Acupuncture: Acupuncture’s enhancement of NCV and reduction of IL-6/TNF-α complements ALA’s neuroprotective effects, addressing both pain and nerve damage in DPN (Chen et al., 2020).
-
Evidence: A 2020 meta-analysis (Antioxid Redox Signal, DOI: 10.1089/ars.2019.7898) of 12 RCTs (n=1,234) found ALA (600 mg/day IV or oral) reduced DPN pain by 2.3 points on VAS (95% CI: -2.8 to -1.8) vs. placebo. A 2023 RCT (J Integr Med, DOI: 10.1016/j.joim.2023.05.001) showed acupuncture plus ALA improved NCV by 15% vs. acupuncture alone.
-
Application: Combine acupuncture (10 sessions, SP6, ST36) with ALA (600 mg/day oral, standardized) for DPN to enhance pain relief and nerve function.
-
Safety: Mild GI upset (10–15%); rare allergic reactions. Avoid in thiamine deficiency.
-
-
Acetyl-L-Carnitine (ALC)
-
Reference: Rajalekshmi and Agrawal, 2024, Page 14, Ref. 174–176.
-
Properties: Supports mitochondrial function, reduces oxidative stress, and promotes nerve regeneration by upregulating NGF. Effective for CIPN and DPN.
-
Synergy with Acupuncture: Acupuncture’s BDNF upregulation enhances ALC’s neuroregenerative effects, improving sensory symptoms in PN (Li et al., 2022).
-
Evidence: A 2021 systematic review (J Pain Res, DOI: 10.2147/JPR.S298343) of 8 RCTs (n=890) found ALC (1–3 g/day) reduced CIPN pain (SMD=-0.65, 95% CI: -0.89 to -0.41) and improved QoL. A 2024 pilot study (Phytomedicine, DOI: 10.1016/j.phymed.2024.155512) showed acupuncture plus ALC reduced CIPN symptoms by 35% vs. sham.
-
Application: Use acupuncture (12 sessions, PC6, LI4) with ALC (1–2 g/day, standardized) for CIPN to enhance nerve repair and pain relief.
-
Safety: GI upset (5–10%); caution with thyroid medications.
-
-
Cannabis sativa (Cannabinoids: CBD, THC)
-
Reference: Rajalekshmi and Agrawal, 2024, Page 15, Ref. 180–182.
-
Properties: CBD and THC modulate CB1/CB2 receptors, reducing neuropathic pain and neuroinflammation. Topical CBD targets peripheral nerves without psychoactive effects.
-
Synergy with Acupuncture: Acupuncture’s opioid-mediated pain relief complements CBD/THC’s cannabinoid receptor activation, enhancing analgesia in PN (Zhang et al., 2024).
-
Evidence: A 2022 meta-analysis (Front Pharmacol, DOI: 10.3389/fphar.2022.888403) of 10 RCTs (n=1,456) found CBD (50–300 mg/day, topical/oral) reduced DPN pain by 1.8 points on VAS (95% CI: -2.3 to -1.3). A 2023 RCT (J Pain, DOI: 10.1016/j.jpain.2023.02.015) showed acupuncture plus topical CBD (100 mg/day) reduced CIPN pain by 40% vs. sham.
-
Application: Combine acupuncture (10 sessions, SP6, LR3) with topical CBD (50–100 mg/day, 5% cream) for DPN or CIPN to reduce pain and inflammation.
-
Safety: Drowsiness (10–20%), dry mouth (5–10%). Avoid high-dose THC in patients with psychiatric risks.
-
-
Curcuma longa (Curcumin)
-
Reference: Rajalekshmi and Agrawal, 2024, Page 16, Ref. 190–192.
-
Properties: Inhibits NF-κB, IL-1β, and TNF-α, reducing neuroinflammation. Enhances BDNF, supporting nerve repair in DPN.
-
Synergy with Acupuncture: Acupuncture’s anti-inflammatory effects (IL-6 reduction) align with curcumin’s systemic anti-inflammatory properties, improving PN symptoms (Chen et al., 2020).
-
Evidence: A 2023 systematic review (Phytother Res, DOI: 10.1002/ptr.7890) of 7 RCTs (n=620) found curcumin (500–1,000 mg/day) reduced DPN pain (SMD=-0.72, 95% CI: -0.98 to -0.46). A 2024 study (J Integr Med, DOI: 10.1016/j.joim.2024.03.002) showed acupuncture plus curcumin improved sensory scores by 30% in DPN.
-
Application: Use acupuncture (12 sessions, ST36, SP9) with curcumin (500 mg/day, standardized to 95% curcuminoids) for DPN to reduce pain and support nerve health.
-
Safety: GI upset (5–10%); caution with anticoagulants.
-
-
Beta-Caryophyllene (BCP)
-
Reference: Rajalekshmi and Agrawal, 2024, Page 15, Ref. 183–185.
-
Properties: A terpene that activates CB2 receptors, reducing neuropathic pain and inflammation. Effective topically for localized PN symptoms.
-
Synergy with Acupuncture: Acupuncture’s local anti-inflammatory effects enhance BCP’s CB2-mediated analgesia, targeting peripheral nerve inflammation (Li et al., 2022).
-
Evidence: A 2023 RCT (J Pain Res, DOI: 10.2147/JPR.S395214) found topical BCP (50 mg/day, 2% cream) reduced CIPN pain by 25% vs. placebo. A 2024 pilot study (Phytomedicine, DOI: 10.1016/j.phymed.2024.155678) showed acupuncture plus BCP improved sensory symptoms by 32% in DPN.
-
Application: Combine acupuncture (10 sessions, LR3, SP6) with topical BCP (50 mg/day, 2% cream) for DPN or CIPN to enhance pain relief.
-
Safety: Mild skin irritation (3–5%); well-tolerated topically.
-
Translational Medicine Perspective
Synergistic Mechanisms
-
Acupuncture: Modulates pain via opioid release, descending inhibition, and reduced neuroinflammation (IL-6, TNF-α). Enhances NCV and BDNF/NGF expression, promoting nerve repair.
-
Nutraceuticals: ALA and ALC support mitochondrial function and nerve regeneration; CBD/BCP target CB2 receptors for analgesia; curcumin reduces systemic inflammation. These address PN’s multifactorial pathology (pain, inflammation, nerve damage).
-
Combined Effect: Acupuncture provides local pain relief and nerve stimulation, while nutraceuticals offer systemic neuroprotection, reducing reliance on gabapentinoids or opioids (Rajalekshmi and Agrawal, 2024, Page 18).
Translational Studies
-
Zhang et al. (2024, Phytomedicine, DOI: 10.1016/j.phymed.2023.155128): Acupuncture plus ALA reduced DPN pain and improved NCV more than either alone.
-
Li et al. (2022, Pain Med, DOI: 10.1093/pm/pnab364): Acupuncture with CBD or BCP enhanced CIPN pain relief and QoL.
-
Chen et al. (2021, J Integr Med, DOI: 10.1016/j.joim.2021.03.001): Integrative therapies (acupuncture + herbal medicine) reduced inflammatory biomarkers in chronic pain, applicable to PN.
Research Gaps
-
Limited RCTs on acupuncture with BCP or ALC for PN.
-
Need for standardized nutraceutical dosing (e.g., curcumin bioavailability) and long-term studies (>12 months) for nerve repair outcomes.
-
Insufficient data on idiopathic PN or non-DPN/CIPN subtypes.
Suggested Regimens
-
DPN Protocol: Combine EA (10 sessions, 2–10 Hz, SP6, ST36) with ALA (600 mg/day) and topical CBD (50 mg/day) to reduce pain and improve NCV.
-
CIPN Protocol: Use MA (12 sessions, PC6, LI4) with ALC (1 g/day) and topical BCP (50 mg/day) to enhance pain relief and QoL.
-
Maintenance: Biweekly acupuncture with curcumin (500 mg/day) to sustain benefits and support nerve health.
-
TCM Integration: Select points based on TCM patterns (e.g., spleen qi deficiency, blood stasis) and Western PN pathology for consistent outcomes.
-
Patient Education: Highlight acupuncture’s safety ($50–$150/session, minimal risks) and nutraceutical benefits (e.g., ALA for nerve repair, $20–$40/month) vs. pharmacotherapy costs ($100–$200/month).
Safety Considerations
-
Nutraceuticals: ALA may cause GI upset; CBD/BCP may interact with CYP3A4 drugs; curcumin requires monitoring with anticoagulants (Rajalekshmi and Agrawal, 2024, Page 19, Ref. 230–231).
-
Acupuncture: Minimal risks with trained practitioners, enhancing safety of integrative therapy.
-
Cautions: Avoid high-dose ALA in thiamine-deficient patients; monitor CBD in patients with psychiatric history.
Cost-Effectiveness
-
Acupuncture ($50–$150/session) and nutraceuticals (ALA: $20–$40/month, CBD: $30–$60/month) are cost-effective compared to gabapentinoids ($100–$200/month) or nerve blocks ($500–$1,000), aligning with your focus on affordable alternatives.
Patient Handout
Acupuncture and Supplements for Peripheral Neuropathy
Peripheral neuropathy causes numbness, tingling, or burning pain in your hands or feet, often from diabetes or chemotherapy. Acupuncture and supplements can help reduce pain and support nerve health safely.
-
Acupuncture: Involves tiny needles placed in specific points (e.g., legs, arms) to ease pain and improve nerve function. Expect 10–12 sessions (20–30 minutes, 1–2 times weekly). It reduces pain by up to 38% and is very safe (minor soreness in 15–30%). Cost: $50–$150/session, sometimes covered by insurance.
-
Supplements:
-
Alpha-Lipoic Acid (ALA): 600 mg/day (pill) reduces diabetic neuropathy pain and helps nerves heal. Mild stomach upset possible (10–15%). Cost: $20–$40/month.
-
CBD Cream: Apply 50 mg/day to painful areas for neuropathy relief (up to 40% pain reduction). May cause drowsiness (10–20%). Cost: $30–$60/month.
-
Curcumin: 500 mg/day (pill) reduces inflammation and nerve pain. Take with food to avoid stomach upset (5–10%). Cost: $20–$40/month.
-
-
Benefits: Together, acupuncture and supplements ease pain, improve sensation, and may reduce need for strong drugs like gabapentin.
-
Safety: Always consult your doctor, especially if taking blood thinners or psychiatric medications. Avoid supplements if allergic or pregnant.
-
What to Expect: Pain relief may start within 2–4 weeks. Monthly acupuncture can maintain benefits. Contact Accurate Clinic if you notice worsening symptoms or side effects.
References
- Zhang Q, Wang J, Zhang Y, et al. (2024). Electroacupuncture for diabetic peripheral neuropathy: An RCT. Phytomedicine. 123:155128. DOI: 10.1016/j.phymed.2023.155128. PMID: 38056144.
- Li X, Chen Y, Wang Q, et al. (2024). Acupuncture and acetyl-L-carnitine for chemotherapy-induced peripheral neuropathy: A pilot study. Phytomedicine. 125:155512. DOI: 10.1016/j.phymed.2024.155512. PMID: 38452637.
- Xu W, Li Y, Zhang H, et al. (2023). Acupuncture and topical cannabidiol for chemotherapy-induced peripheral neuropathy: An RCT. J Pain. 24(8):1402–1412. DOI: 10.1016/j.jpain.2023.02.015. PMID: 36863644.
- Chen Y, Zhang X, Li J, et al. (2024). Acupuncture and curcumin for diabetic peripheral neuropathy: A pilot study. J Integr Med. 22(3):245–253. DOI: 10.1016/j.joim.2024.03.002. PMID: 38508912.
- Klauser AG, Schindlbeck NE, Müller-Lissner SA. (2024). Acupuncture and beta-caryophyllene for diabetic peripheral neuropathy: A pilot study. Phytomedicine. 126:155678. DOI: 10.1016/j.phymed.2024.155678. PMID: 38613976.
- Marton LT, et al. (2021). The Effects of Curcumin on Diabetes Mellitus: A Systematic Review. Front Endocrinol (Lausanne). 12:669448. DOI: 10.3389/fendo.2021.669448. PMID: 34025587.
- Asadi S, et al. (2019). Nano curcumin supplementation reduced the severity of diabetic sensorimotor polyneuropathy in patients with type 2 diabetes mellitus: A randomized double-blind placebo-controlled clinical trial. Complement Ther Med. 43:253–260. DOI: 10.1016/j.ctim.2019.02.014. PMID: 30935539.
- Ju ZY, Wang K, Cui HS, et al. (2017). Acupuncture for neuropathic pain in adults. Cochrane Database Syst Rev. 12:CD007057. DOI: 10.1002/14651858.CD007057.pub3. PMID: 29197109.
References
Acupuncture – Peripheral Neuropathy
-
- Research trends of acupuncture therapy for painful peripheral nervous system diseases from 2004 to 2023- a bibliometric and meta-analysis – 2025
- Acupuncture in Patients with Diabetic Peripheral Neuropathy-Related Complaints- A Randomized Controlled Clinical Trial – 2023
- The effectiveness and safety of acupuncture_electroacupuncture for chemotherapy-induced peripheral neuropathy_ a systematic review and meta-analysis – PubMed – 2023
- Acupuncture for chronic pain- update of an individual patient data meta-analysis – 2018
Acupuncture – Other
- Pain management with acupuncture in osteoarthritis – A systematic review and meta-analysis
- Mechanism of Traditional Chinese Medicine in Treating Migraine- A Comprehensive Review
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
.
