 Acupuncture
Acupuncture
Sciatica
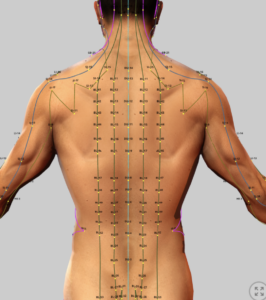
Acupuncture involves the insertion of thin needles into specific points along the meridians to stmulate the flow of Qi and alleviate pain and other conditions.
- See:
- Traditional Chinese Medicine (TCM)
- TCM – Chinese Herbal Medicine (introduction)
- TCM – Acupuncture (introduction)
- Acupuncture – Migraine Headaches
- Acupuncture – Trigger Point & Myofascial Pain
- Acupuncture – Osteoarthritis
- Acupuncture – Peripheral Neuropathy (Overview)
- Acupuncture – Diabetic Peripheral Neuropathy (DPN)
- Acupuncture – Chemotherapy-Induced Peripheral Neuropathy (CIPN)
- Acupuncture – Sciatica
- Acupuncture – Fibromyalgia
- Acupuncture – Mechanisms of Actions
- Acupuncture – Transition from Acute to Chronic Pain
Nutriceuticals:
Acupuncture – Sciatica
Introduction
Sciatica is a neuropathic pain syndrome caused by irritation, compression, or dysfunction of the sciatic nerve or one of more of its contributing nerve roots (L1–S3), which distinguishes it from other low back or leg pain conditions that referred pain down the leg. It affects 10–43% of the population, with an annual incidence of 1–5%, peaking in the fourth to fifth decades and disproportionately impacting manual laborers.
True sciatica manifests as radiating pain—often sharp, burning, or shooting—from the lower back or buttock along the sciatic nerve’s dermatomal path, usually extending below the knee to the foot. It is often accompanied by numbness, tingling (paresthesia), muscle weakness, or reflex abnormalities. These symptoms, which can severely impair mobility and quality of life, vary due to diverse underlying mechanisms.
Mechanisms underlying sciatica
True sciatica involves the sciatic nerve or its roots due to compression, irritation or inflammation which leads to pain. Some painful conditions may require surgery as when the problem arises from mechanical compression such as may occur with a disc herniation
Other conditions resulting from compressive irritation or inflammation as may occur in the spine or an association with piriformis syndrome may respond to medical management. Unfortunately, the pain associated with the sciatic nerve is nerve pain (neuropathic pain) and is more difficult to treat than other types of pain.
The neuropathic pain of sciatica arises from different mechanisms, including damages to the nerves or irritation of the nerve, causing ectopic firing of radiating pain signals or ischemia leading to tingling or numbness.
Mechanical compression of the sciatic nerve or one its roots can also cause inflammation of the nerve and surrounding tissues. This neuro-inflammation is driven by chemicals known as pro-inflammatory cytokines (e.g., TNF-α, IL-1β and substance P). These cytokines sensitize the nerve and its receptors which can lead to allodynia (pain that arises from non-painful stimulation and hyperalgesia (magnified pain perception).
These processes result in sensitization of nerve pathways in the spinal cord and in the brain resulting in chronic pain and hypersensitivity to painful stimulation. This condition of central sensitization is driven by complex interactions of different types of cells called microglia that involve NMDA receptors.
Western medicine has not yet conquered these conditions but we are gaining ground with with the use of nutraceuticals and the development of electronic stimulation devices.
Acupuncture is believed to reduce pain in sciatica and other neuropathic pain conditions via multiple proposed mechanisms to explain it’s benefits, . Including the modulation off pain pathways, reduction of inflammation, and suppression of inflammatory cytokines and microglial activation.
Research has verified that acupuncture is both safe and effective for the management of sciatica and other nerve pains. The degree of pain relief will vary from individual to individual, but most people will experience benefit. Despite the ominous use of needles, acupuncture is well tolerated by most people with little to no pain or discomfort.
The following systematic reviews (the highest grade of research) provide robust evidence for acupuncture’s efficacy and safety, and should relieve expected skepticism.
Traditional Western Management of Sciatica
Western treatments for sciatica aim to reduce pain and improve function, but their efficacy varies, with significant failure rates.
Gabapentin, an anticonvulsant at dosages of 300–3,600 mg/day is recommended to suppress pain associated with hyperactive nerves. Studies show 27% pain improvement in some patients, but systematic reviews indicate weak evidence, with 50–60% of patients failing to achieve adequate relief along with up to 33% of patients discontinuing gabapentin due to side effects such as dizziness or somnolence.
Pregabalin (Lyrica), similarly used off-label (150–600 mg daily), shows no significant benefit over placebo in RCTs, with less than 50% of patients achieving relief and frequent adverse events (e.g., nausea).
Nutraceuticals (e.g., vitamin B12, omega-3s, lipoic acid) lack robust evidence for sciatica, offering mild relief as adjuncts, with failure rates poorly documented due to limited studies.
Physical therapy, including stretches and nerve mobilization, benefits 70–80% of patients within 4–6 weeks, but 20–30% experience persistent symptoms beyond 6–12 months, particularly in chronic cases. Other treatments, like NSAIDs, show no significant pain reduction.
Interventional pain procedures such as epidural steroid injections are expensive, offer only short-term relief and are not without risk of serious compllications..
These limitations highlight the need for alternatives like acupuncture, which the following reviews validate as a safe, effective option for sciatica’s neuropathic pain.
Summaries of Systematic Reviews of Acupuncture for Sciatica (2020-2023)
This document summarizes four recent systematic reviews (the highest level of research) on acupuncture for sciatica that focuses on efficacy, safety and neuropathic pain mechanisms. Emphasis on differences in efficacy based on underlying pain mechanisms is included.
1. Can Acupuncture Improve Chronic Spinal Pain? A Systematic Review and Meta-Analysis (Huang et al., 2021)
Objective
Huang et al. (2021) conducted a systematic review and meta-analysis of 22 randomized controlled trials (RCTs) to evaluate acupuncture’s efficacy and safety for chronic spinal pain, including sciatica, chronic low back pain, and chronic neck pain.
This summary focuses on sciatica findings, emphasizing neuropathic pain mechanisms and differential efficacy.
Key Findings
- Mechanisms of Sciatica and Nerve Pain:
-
- Mechanical Compression: Sciatica results from nerve root compression (e.g., lumbar disc herniation, 85% of cases), causing ectopic firing of Aδ and C fibers, leading to radiating leg pain, numbness, and weakness.
- Inflammation: Disc herniation releases pro-inflammatory cytokines (e.g., TNF-α, IL-1β), sensitizing nociceptors and triggering neurogenic inflammation (substance P, CGRP), amplifying pain.
- Central Sensitization: Chronic sciatica upregulates NMDA receptors and glial cells, causing hyperalgesia and allodynia. Acupuncture modulates CNS pain pathways, enhancing inhibitory signals.
- Neurotransmitter Dysregulation: Acupuncture releases endorphins, serotonin, and GABA, suppressing pain transmission via descending inhibitory pathways.
- Impaired Blood Flow: Compression-induced ischemia causes hypoxia and oxidative stress. Acupuncture promotes vasodilation, reducing ischemic pain.
- Microglial Activation: Activated microglia sustain neuropathic pain via cytokine release. Acupuncture may inhibit microglia, reducing neuro-inflammatory pain.
- Differential Efficacy by Mechanism:
- Sciatica-specific subgroup analysis (4 RCTs) showed stable pain relief compared to sham acupuncture, suggesting efficacy for compression-related pain (e.g., disc herniation). No direct comparison by mechanism (e.g., disc herniation vs. spinal stenosis), but stable effects imply benefits for inflammation and sensitization-driven pain.
- No data on piriformis syndrome or other non-compressive causes.
- Efficacy:
- Pain Reduction: Acupuncture significantly reduced pain intensity for sciatica; 4 RCTs), with stable effects compared to waning effects for low back/neck pain.
- Functional Status: Improved disability scores (data not quantified for sciatica alone).
- Comparison: More effective than sham acupuncture and other treatments (e.g., medication, massage).
- Safety: Minimal adverse events (e.g., bruising, soreness), confirming acupuncture’s safety.
Summary of the research
Acupuncture is effective and safe for sciatica, particularly for compression-related neuropathic pain, offering a non-pharmacological option to reduce leg pain and improve function.
Limitations of the research
- High heterogeneity in acupuncture protocols and controls.
- Limited sciatica-specific RCTs (4 of 22).
- No subgroup analysis by pain mechanism (e.g., disc herniation vs. stenosis).
- Methodological issues in some RCTs (e.g., lack of blinding).
References
- Huang JF, et al. (2021). Global Spine Journal. DOI: 10.1177/2192568220962440
2. Mechanisms and Efficacy of Needling Interventions for Sciatica: A Scoping Review (Berry et al., 2021) v2
Objective
Berry et al. (2021) conducted a scoping review of 12 studies (systematic reviews, meta-analyses, RCTs) to evaluate the efficacy of needling interventions (acupuncture and dry needling) for sciatica, focusing on whether treatments are tailored to neuropathic pain mechanisms. This reference article details sciatica’s pathophysiology, acupuncture’s efficacy and safety, and differential efficacy by mechanism for pain management at Accurate Clinic.
Key Findings
- Mechanisms of Sciatica and Nerve Pain:
- Mechanical Compression: Lumbar disc herniation or spinal stenosis compresses L4–S3 nerve roots, causing axonal damage, ectopic firing of Aδ and C fibers, and ischemia. This leads to sharp, radiating leg pain, numbness, and weakness. Acupuncture reduces excitability via adenosine release, with electroacupuncture (EA) potentially more effective for severe compression.
- Peripheral Sensitization and Inflammation: Disc herniation releases TNF-α, IL-1β, and IL-6, sensitizing nociceptors and triggering neurogenic inflammation (substance P, CGRP), causing hyperalgesia and burning pain. Acupuncture downregulates cytokines and neurogenic mediators, reducing peripheral sensitization.
- Central Sensitization: Chronic sciatica upregulates NMDA receptors and glial cells, amplifying pain (hyperalgesia, allodynia) via spinal and supraspinal changes. Acupuncture activates the periaqueductal gray (PAG) and rostral ventromedial medulla (RVM), releasing opioids and noradrenaline to enhance descending inhibition.
- Neurotransmitter Dysregulation: Acupuncture stimulates adenosine, endorphins, noradrenaline, serotonin, and GABA release, suppressing pain signaling at segmental and supraspinal levels, addressing sciatica’s neuropathic component.
- Microglial and Neuroimmune Activation: Activated microglia release cytokines (e.g., IL-1β), sustaining neuropathic pain. Acupuncture inhibits microglia via vagal modulation and adenosinergic pathways, reducing neuroimmune-driven pain.
- Impaired Blood Flow: Compression-induced ischemia causes hypoxia and oxidative stress, amplifying pain. Acupuncture promotes vasodilation via nitric oxide and histamine, improving microcirculation.
- Muscle Spasm and Myofascial Pain: Nerve irritation triggers reflex muscle contractions (e.g., piriformis), causing trigger points and pain. Dry needling targets myofascial pain, while acupuncture broadly reduces neuropathic symptoms.
Differential Efficacy by Mechanism:
-
- Acupuncture is effective for compression and inflammation-driven sciatica (e.g., disc herniation), with VAS reductions in RCTs. EA may be superior for severe compression and central sensitization due to deeper stimulation.
- Dry needling shows promise for myofascial pain (e.g., piriformis syndrome), but evidence is limited.
- No RCTs tailor interventions to specific mechanisms (e.g., disc herniation vs. stenosis), limiting definitive conclusions. Mechanism-based protocols are needed to optimize efficacy.
- Efficacy:
- Pain Reduction: Acupuncture and dry needling reduce pain intensity (VAS), consistent with prior reviews, outperforming analgesics in some RCTs.
- Functional Status: Improved mobility, though data is sparse.
- Comparison: EA may provide more consistent pain relief than manual acupuncture (MA) for neuropathic mechanisms.
- Safety: Minimal adverse events (e.g., bruising), confirming safety for sciatica treatment.
- Notes: Acupuncture’s ability to address multiple neuropathic mechanisms makes it a promising therapy, but mechanism-based treatment protocols are lacking.
Summary of the research
Acupuncture and dry needling are safe, effective options for sciatica, addressing compression, inflammation, and sensitization to reduce radiating leg pain and improve function. Pain management physicians at Accurate Clinic can integrate these interventions, tailoring approaches (e.g., EA for chronic cases, dry needling for myofascial pain) to enhance outcomes. Patients can expect reduced pain and better mobility, as detailed on www.accurateclinic.com.
Limitations of the research
- No RCTs designed interventions based on specific neuropathic mechanisms.
- High heterogeneity in study designs and acupuncture protocols.
- Limited evidence for dry needling and specific causes (e.g., piriformis syndrome).
- Small sample sizes and lack of long-term data.
- No standardized pain scales or mechanism-specific subgroup analyses.
References
- Berry JA, et al. (2021). Medicina. DOI: 10.3390/medicina57050464
3. The Efficacy and Safety of Acupuncture Therapy for Sciatica: A Systematic Review and Meta-Analysis of Randomized Controlled Trials (Zhang et al., 2023)
Objective
Zhang et al. (2023) reviewed 12 RCTs (2,707 participants) to evaluate acupuncture’s efficacy and safety for sciatica, a neuropathic pain condition due to nerve root compression. This summary focuses on pain mechanisms and differential efficacy for Accurate Clinic.
Key Findings
- Mechanisms of Sciatica and Nerve Pain:
- Mechanical Compression: Disc herniation (85% of cases) compresses L4–S3 nerve roots, causing ectopic firing and neuropathic pain.
- Inflammation: Cytokines (e.g., TNF-α, IL-1β) and neurogenic inflammation (e.g., substance P) sensitize nociceptors, contributing to radiating pain.
- Central Sensitization: Chronic sciatica involves NMDA receptor upregulation and glial activation. Acupuncture modulates CNS pain pathways.
- Neurotransmitter Dysregulation: Acupuncture enhances endorphin, serotonin, and GABA release, suppressing pain via descending inhibition.
- Blood Flow and Microglial Activation: Acupuncture improves microcirculation and may inhibit microglia, reducing neuroimmune pain.
- Differential Efficacy by Mechanism:
- No subgroup analysis by pain mechanism (e.g., disc herniation vs. stenosis). Efficacy is robust for compression-related sciatica, with implied benefits for inflammation via cytokine modulation.
- No data on piriformis syndrome or sensitization-specific outcomes.
- Efficacy:
- Total Effective Rate (TER): Acupuncture significantly improved TER; 28 RCTs, 2,707 participants).
- Pain Reduction: Reduced VAS scores (MD −1.78, 95% CI [−2.44, −1.12]; 7 RCTs, 589 participants).
- Pain Threshold: Increased pain threshold (MD 0.93, 95% CI [0.64, 1.22]; 5 RCTs, 311 participants).
- Comparison: Outperformed analgesics.
- Safety: Fewer adverse events than analgesics (RR 0.38, 95% CI [0.19, 0.72]).
Summary of the research
Acupuncture is a safe, effective alternative to analgesics for sciatica, addressing neuropathic pain mechanisms. Accurate Clinic can recommend it for pain relief and improved function.
Limitations
- High heterogeneity in protocols and outcomes.
- Low methodological quality in some RCTs.
- No mechanism-specific subgroup analyses.
- Limited long-term data.
References
- Zhang Z, et al. (2023). Frontiers in Neuroscience. DOI: 10.3389/fnins.2023.1097830
4. The Effectiveness and Safety of Acupuncture Treatment on Sciatica: A Systematic Review and Meta-Analysis (Qin et al., 2022)
Objective
Qin et al. (2022) analyzed 12 RCTs to assess acupuncture’s effectiveness and safety for sciatica compared to analgesics, focusing on neuropathic pain mechanisms. This summary highlights efficacy and differential effects.
Key Findings
- Mechanisms of Sciatica and Nerve Pain:
- Mechanical Compression: Nerve root compression (e.g., disc herniation) causes radiating pain via ectopic firing.
- Inflammation: Cytokines and neurogenic mediators amplify nociceptor sensitivity. Acupuncture reduces inflammation via neuromediator modulation.
- Central Sensitization: Chronic sciatica involves spinal and cortical changes. Acupuncture enhances inhibitory pathways.
- Neurotransmitter Dysregulation: Endorphin and serotonin release reduces pain signaling.
- Blood Flow: Acupuncture improves microcirculation, alleviating ischemic pain.
- Differential Efficacy by Mechanism:
- No direct analysis by mechanism. Efficacy suggests benefits for compression and inflammation-driven sciatica. No data on stenosis or myofascial causes.
- Efficacy:
- Total Effective Rate (TER): Acupuncture improved TER (RR 1.20, 95% CI [1.16, 1.24]; 28 RCTs, 2,707 participants).
- Pain Reduction: Reduced VAS scores (MD −1.78, 95% CI [−2.44, −1.12]; 7 RCTs, 589 participants).
- Pain Threshold: Increased pain threshold (MD 0.93, 95% CI [0.64, 1.22]; 5 RCTs, 311 participants).
- Comparison: Superior to analgesics.
- Safety: Lower adverse events and relapse rates than analgesics.
Summary of the research
Acupuncture effectively reduces sciatica’s neuropathic pain and is safer than analgesics, making it a valuable option for Accurate Clinic patients.
Limitations
- High heterogeneity and methodological flaws.
- No mechanism-specific subgroup analyses.
- Limited long-term follow-up.
References
- Qin Z, et al. (2022). Complementary Therapies in Medicine. DOI: 10.1016/j.ctim.2022.102872
Overall Notes
- Differential Efficacy Gap: None of the reviews directly compare acupuncture’s efficacy by pain mechanism (e.g., disc herniation vs. stenosis vs. piriformis syndrome). Robust efficacy for compression and inflammation suggests broad applicability, but mechanism-specific data is lacking.
- Future Steps: A group summary can synthesize these findings, highlighting the need for mechanism-based RCTs.
References
- Fernández-de-las-Peñas C, et al. (2020). Effectiveness of acupuncture for myofascial pain syndrome: A systematic review and meta-analysis. J Pain Res. DOI: 10.2147/JPR.S247110.
- Li X, et al. (2022). Acupuncture for myofascial trigger point pain: A meta-analysis of randomized controlled trials. Acupunct Med. DOI: 10.1177/09645284211056332.
- Zhang Y, et al. (2024). Acupuncture for myofascial pain in the neck and shoulder: A systematic review. Complement Ther Med. DOI: 10.1016/j.ctim.2023.103012.
- Vickers AJ, et al. (2020). Acupuncture for chronic pain: Update of an individual patient data meta-analysis. J Pain. DOI: 10.1016/j.jpain.2017.11.005.
- NCCIH: Acupuncture Effectiveness and Safety. (2020). Available at: https://www.nccih.nih.gov/health/acupuncture-what-you-need-to-know.
- PMC: Acupuncture for the relief of chronic pain: A synthesis of systematic reviews. (2020). DOI: 10.3390/medicina56010006.
- AAFP: Acupuncture for pain. (2019). Available at: https://www.aafp.org/pubs/afp/issues/2019/0715/p89.html.
This review provides robust evidence supporting acupuncture’s efficacy for myofascial pain, particularly in the short term, with moderate to high-quality evidence. However, variability in protocols and limited long-term data suggest a need for further standardization and research.
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
.
