“When one door closes another door opens; but we so often look so long and so regretfully upon the closed door, that we do not see the ones which open for us.”
– Alexander Graham Bell
Osteoarthritis:
Conventional & Complementary and Alternative Medicine (CAM)
In treating arthritis pain, the first order of treatment should be the use of topical medications because of their effectivenes and their greater safety compared with oral medications.
See: Topica Medications for Pain
Despite the advances made in modern medicine, conventional medical management of arthritis pain and stiffness is, more often than not, inadequate. With respect to pain medications, the usual first approach is the use of NSAIDs (non-steroid anti-inflammatory drugs like ibuprofen) which have limited benefit and are often associated with significant side effects so that they are frequently not tolerated or unsafe. When NSAIDs fail to control arthritis pain, the next step is usually opioid analgesics. While opioids can often control the pain of arthritis, opioids are also associated with significant risks of side effects. For many, opioids are not available or appropriate due to other concerns.
Furthermore, neither NSAIDs nor opioids actually offer any benefit towards reversing the structural damage to joints associated with arthritis, nor do they slow the progress of arthritis. The medical community is in desperate need of safe and effective alternatives to what is currently available. The CAM field offers a number of supplements that offer potential benefit in the management of arthritis, including not only the pain but also in reducing the progression of the disease. While there are as yet no magic bullets, the substances and research reviewed below suggest possible alternative treatment options for the management of arthritis.
See also:
- CAM – Medications for Pain
- CAM – Fibromyalgia
- CAM – Headaches
- CAM – Interstitial Cystitis
- CAM & Conventional – Neuropathic (nerve) Pain
- CAM & Conventional – Nutrition and Supplements
- CAM – SUD, Addiction Recovery
- Palmitoylethanolamide (PEA)
And:
Naturopathic Medicine – Dr. Lisa Chambers Pate
Definitions and Terms Related to Pain
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
.
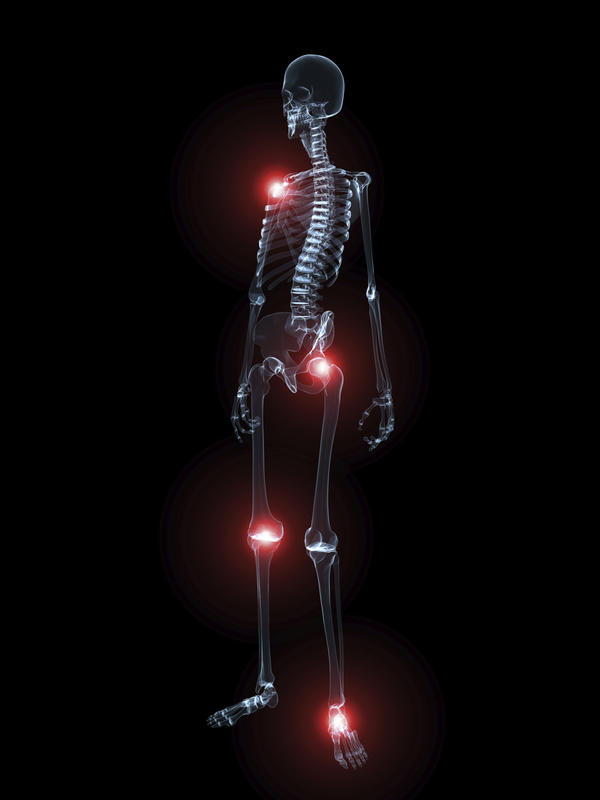
Osteoarthritis
Osteoarthritis (OA) is a condition that affects approximately 15% of the world’s population. It is three times more common in women than in men. It involves progressive destruction of the cartilage on the joint surfaces which results in impaired joint function, swelling, pain, and disability. In addition to the destruction of cartilage, OA involves damage to bone and nerves as well as inflammation. While osteoarthritis commonly affects the knees, hips, hands and shoulders it is also a major contributor to neck and back pain.
Peripheral and Central Pain Sensitization
The pain is a result of all of these conditions and pain severity is largely determined by the forces associated with compressing the arthritic joint. During the last decade there has been greater understanding not only of the inflammatory aspects of OA, including contributions from various inflammatory chemicals like interleukins, cytokines and nerve growth factor, but there is also a growing appreciation of the role of peripheral and central pain sensitization in OA. Manifestations of sensitization include the spread of perceived pain beyond areas of disease, including referred and radiating pain. This role of central sensitization in OA suggests the potential benefits of treatment directed at reducing existing sensitization and taking efforts at suppressing further develepment of sensitization.
A contributing mechanism of central sensitization is the dysregulation of nerve pathways that descend from the brain into the spinal cord to interact with ascending pain pathways. These descending pathways normally function to reduce pain signalling from the nerves in the dorsal horns of the spinal cord that contribute to pain perception. The control of the descending pathways to inhibit pain is referred to as Conditioned Pain Modulation (CPM). Reduced CPM has been shown in OA patients, strongly indicating dysregulated top‐down modulation develops as the pain state progresses. Treatments directed at restoring pain inhibition in these pathways are potentially effective in managing OA pain. These treatments include behavioral mind-based treatments as well as prescription medications such as duloxetine (Cymbalta) and tapentadol (Nucynta).
Neuroinflammation
A growing body of evidence now points to inflammation, locally and more systemically, as a promoter of damage to joints and bones, as well as joint-related functional problems. The disease process underlying joint diseases is currently believed to involve communication between cartilage and the subchondral bone beneath the cartilage in the joint—and a loss of balance between these two structures. Research over the last 5-10 years indicates that chronic pain is largely due to a process called neuroinflammation, a condition characterized by activation of a number of inflammatory cells within the peripheral and central nervous systems.
Neuroinflammation is characterized by migration of immune cells into an area of injury which release inflammatory chemical products that lead to activation and maintenance of chronic pain. These inflammatory cells, mast cells and glial cells, are now targets for development of new medications for treating chronic pain. Evidence indicates that suppression of the activation of these cells may limit or abolish the evolution of acute to chronic pain and may also act to reduce chronic pain.
Dysregulation of the mast cells in joint structures is associated with damage to these structures (cartilage, bone, synovia, matrix, nerve endings, and blood vessels). This process includes neuroinflammation which in turn contributes to the chronic pain associated with arthritis.
Communication between the spinal cord and the joint can cause further neuroinflammatory changes at the spinal level involving the central nervous system and brain. A central sensitization process has also been observed in patients with arthritis, where pain thresholds to pressure and prick stimuli are lower than in healthy subjects,making the person experience pain more easily and severely. This central sensitivity to pain does not correlate with radiological findings, suggesting that central sensitization is the factor that contributes most to arthritis pain.
Unfortunately, current conventional treatment strategies for arthritis are directed only at relieving symptoms and do little to limit progression of the disease process itself.
Assessing Pain in OA
The intensity of pain in OA, especially in knees, correlates poorly with measures of tissue destruction as evidenced by xrays and other imaging studies. For example, 30% – 50% of individuals with moderate-to-severe x-ray changes of OA have no pain, while 10% – 20% of individuals with moderate-to-severe knee pain have normal findings on radiography. Thus one cannot measure or predict the extent of pain simply by obtaining x-rays.
Early research suggests that there may be measurable biomarkers, levels of pain-related chemicals, that can predict to some extent the degree of sensitization and indirectly the levels of pain. These findings require further research for their accuracy and predictive effectiveness before they can be used clinically.
OA and Obesity
Since the pain of arthritis is associated with compressing the joint, weight-bearing joints such as the knees and hips are most severely affected but so are the joints in the spine. The hallmark of treatment therefore is to lose excess weight. Studies have shown that obese individuals without significant knee arthritis who lose 10 lbs will reduce their risk of developing symptoms of knee arthritis by 50%. For those with knee arthritis, a weight loss of only 5-10% of body weight provides significant, easily noticeable improvement in pain and function. So it is not necessary to reach your ideal weight before benefitting from weight loss.
Obesity also contributes to arthritis beyond just placing mechanical stress on your joints. Obesity is associated with an increase in a number of hormones, peptides and other bioactive chemicals manufactured by fat cells that promote inflammation and pain. Because of this it is all the more important to lose excessive weight for those with arthritis.
See Accurate Clinic’s Weight Loss Program, offered at a substantial discount to those patients enrolled in our pain management programs.
OA and Diet
Diet can play a significant role in arthritis and inflammation. Aside from adjusting calories to maintain ideal body weight, it is important to include nutrients that may protect against further joint damage. These nutrients include anti-inflammatories, antioxidants and NRF2 activators which are commonly found in high concentrations in grapes, berries, cherries, pomegranates and peanuts as well as ginger and green tea. Fish and chia seeds are high in omega-3 fatty acids which are powerful anti-inflammatories.
Foods high in fat and sugar are known to promote systemic oxidation and inflammation and should be avoided in those with arthritis.
To learn more about the role of diet and OA, see Accurate Clinic’s Medical Nutrition Services, offered free to those patients enrolled in our pain management programs.
Exercise
Exercise is also very important and most people – though not everyone – will improve their pain and function with modest exercise just a few times a week. Our physical therapist and personal trainer can guide you in a home exercise tailored to your specific needs.
Conventional Treatment of Osteoarthritis (OA)
Anti-inflammatories (NSAIDs)
The medical field unfortunately has nothing to offer in the way of a cure for OA. Surgery has little to offer for most people with arthritis and is generally not recommended. The mainstay of traditional OA treatment has been the use of anti-inflammatories including cortisone (steroids) for severe, acute flair-ups and non-steroid anti-inflammaatory drugs (NSAIDs) such as ibuprofen, naproxen and a handful of prescription NSAIDs. Unfortunately, NSAIDs do nothing to slow the progression of OA or reverse the damages associated with OA. Worse, they have significant safety issues of their own, especially the steroids.
Neuromodulators
Neuromodulators are drugs that modify the function of nerves. Neuromodulator medications such as gabapentin (Neurontin), pregabalin (Lyrica), topiramate (Topamax), duloxetine (Cymbalta) and others may be effective in OA pain by reducing the nerve pain component of OA pain. The neuromodulaters may also be effective in reducing pain associated with central sensitization.
Knee braces, knee sleeves, shoe inserts
Potential benefit may come from use of knee braces, knee sleeves, foot pads, and biomechanical training programs. To learn more about your potential benefits from these options, please talk with our physical therapist or physician. At Accurate Clinic we offer the free services of an orthotics technician to provide assessments of orthotic devices that may fit your needs.
Surgery – Joint Replacements
In addition to the reduction of pain associated with damaged joints when they are replaced with artificial joints, there is evidence that central pain can be reversed after joint replacement as well.
CAM Treatment of Osteoarthritis (OA)
Acupuncture
To find ways to slow the progression of OA and repair the damages it is necessary to look beyond NSAIDs and cortisone and explore CAM treatment options including the use of acupuncture and supplements. Acupuncture may offer some benefits to some but does not provide a cure. A trial of acupuncture is recommended for those who can afford it. While acupuncture is not yet offered at Accurate Clinic, our physician can recommend local acupuncture therapists.
Supplements
Research regarding CAM treatments are limited due to the high costs of performing research studies, especially on substances that cannot be patented. Therefore the following substances are reviewed based on limited research.
Likely to be effective for improving the damage and pain associated with OA:
Glucosamine and Chondroitin (G&C)
Glucosamine promotes cartilage repair by stimulating new growth. There is evidence that glucosamine sulfate may be more effective than glucosamine hydrochloride. Chondroitin helps to maintain the viscosity in joint fluids, stimulates cartilage repair and inhibits enzymes that lead to degeneration of cartilage. They require 3-6 months of use before definitive benefits are seen. If one does not see benefits by 6 months, discontinue use.
Recommended doses: Glucosamine 500 mg 3x/day Chondroitin: 400 mg 3x/day
A recent review article evaluated the combination treatment of knee arthritis with NSAIDs and glucosamine. The 5 studies included in this review all report a significantly greater clinical benefit with a combination of glucosamine plus NSAID compared to either treatment alone. The evidence supports effectiveness in “reducing pain, improving function, and possibly regulating joint damage. However, further randomized trials with larger sample sizes are warranted to confirm these findings.”
Warning:
As a product of lobster, crab, and shrimp shells, glucosamine may cause allergic reactions in patients with seafood allergies. Also, glucosamine can block warfarin (coumadin) so it should be avoided if you are taking this medication. Also, glucosamine may cause an increase blood sugar in diabetics.
Strontium Ranelate
Strontium Ranelate may be able to reduce the damage to bone associated with OA and increase cartilage formation. Incidentally, it has also been reported that Strontium Ranelate may be effective in improving fracuture healing in osteoporotic bones, although not in normal bone.
Recommended dose: 2 gms/day
ASU (Avocado/Soybean Unsaponifiables)
ASU is composed of one third avocado and two thirds soybean unsaponifiables (natural vegetable extracts). ASU inhibits the breakdown of cartilage and promotes cartilage repair by stimulating collagen synthesis and reducing inflammation. It has been shown to reduces pain and stiffness while improving joint function, resulting in decreased dependence on other pain medications.
Recommended dose: (2:1 ratio Avocado:Soy) 300-600 mg/day Suggested brand: Piasclidine®
Vitamin C
Vitamin C is an antioxidants – it may slow damage to the joints and is associated with reduced risk of cartilage loss in OA. Vitamin C may also stimulate collagen synthesis and improve viscosity in joint fluid.
Possibly Effective for improving the pain associated with OA:
SAMe
S-adenosylmethionine (SAMe) has anti-inflammatory and analgesic effects and has been reported to reduce the pain and dysfunction of OA.
Recommended dose: 400 mg 3x/day
Anti-inflammatory Agents
Curcumin is the yellow pigment of turmeric, a popular spice in Indian cuisine and a major ingredient of curry powders. Curcumin reduces inflammation and has been shown to reduce the pain of OA though it is not thought to modify the disease process of OA. Curcumin is poorly absorbed when taken orally but absorption can be markedly improved by the use of a nanoformulation of curcumin, Meriva®.
Recommended dose: 500 mg 2x/day after meals
See: Curcumin (Meriva®)
Boswellia serrata (Frankincense)
Studies show Boswellia relieves joint pain, reduces joint swelling and stiffness, and increases joint flexion and walking distance. It is thought to be an anti-inflammatory.
Cat’s claw:
Relieves pain in OA without any significant side effects
Devil’s claw:
Relieves pain in OA
Ginger:
Ginger has been used for centuries to reduce inflammation and there is evidence that ginger may help reduce pain from osteoarthritis.
Green-Lipped Mussel Extract
Improved knee joint pain, stiffness and mobility. It is thought to be an anti-inflammatory.
Resveratrol (see Polyresveratrol)
Resveratrol is present in grapes, berries, and peanuts and is thought to be an anti-inflammatory, antioxidant and NRF2 activator.
Salicin
Salicin is rapidly metabolised into salicylic acid, which is chemically related to aspirin and offers similar pain benefits but salicin does not affect platelets so it offers no protection against heart attacks or strokes. It is derived from willow bark but can be found in many other plants including meadowsweet, cottonwood, poplar, aspen and wintergreen.
Recommended dose: 240 mg
Contraindications: Should not be used by those allergic to aspirin.
References:
Osteoarthritis – New Articles
- Importance of nociplastic pain in patients with rheumatic diseases – 2023
- Natural medicines of targeted rheumatoid arthritis and its action mechanism – 2022
- Rheumatiod Arthritis- An Updated Overview of Latest Therapy and Drug Delivery – 2019
- Triterpenes as Potential Drug Candidates for Rheumatoid Arthritis Treatment – 2023
CAM Osteoarthritis – Overview
- Osteoarthritis – Diet & CAM Summary
- Managing Osteoarthritis Pain With Medicines – 2012
- Pain Treatment in Arthritis-Related Pain – Beyond NSAIDs – 2012
- New horizons in osteoarthritis – 2013
- Nutraceuticals – Potential for Chondroprotection and Molecular Targeting of Osteoarthritis – 2013
- Osteoarthritis and nutrition. From nutraceuticals to functional foods – a systematic review of the scientific evidence,”
- American College of Rheumatology 2012 recommendations for the use o… – PubMed – NCBI
CAM Osteoarthritis – Acupuncture
CAM Osteoarthritis – Central Sensitization of OA Pain
- Towards a mechanism-based approach to pain management in osteoarthritis – 2013
- Osteoarthritis and Central_Pain – 2016
- Uncovering the Sources of Osteoarthritis Pain – 2016
CAM Osteoarthritis – Curcumin (Meriva®)
- Biological actions of curcumin on articular chondrocytes – 2009
- Efficacy and Safety of Meriva®, a Curcumin-phosphatidylcholine Complex, during Extended Administration in Osteoarthritis Patients
- Product-evaluation registry of Meriva®, a curcumin-phosphatidylcholine complex, for the complementary management of osteoarthritis – 2010
- Anti-inflammatory Properties of Curcumin, a Major Constituent of Curcuma longa_ A Review of Preclinical and Clinical Research
- Therapeutic roles of curcumin – lessons learned from clinical trials. – 2013
- Meriva®+Glucosamine versus Condroitin+Glucosamine in patients with knee osteoarthritis – 2014
CAM Osteoarthritis – Glucosamine and Chondroitin (G&C)
- Efficacy of glucosamine, chondroitin, and methylsulfonylmethane for spinal degenerative joint disease and degenerative disc disease – a systematic review
- Combined chondroitin sulfate and glucosamine for painful knee osteoarthritis 2014
- Meriva®+Glucosamine versus Condroitin+Glucosamine in patients with knee osteoarthritis – 2014
- chondroitin-for-osteoarthritis-2015
- Possible synergic action of non-steroidal anti-inflammatory drugs and glucosamine sulfate for the treatment of knee osteoarthritis- a scoping review – 2022
CAM Osteoarthritis – ASU (Avocado/Soybean Unsaponifiables
- Management of Osteoarthritis with Avocado:Soybean Unsaponifiables
- Oral herbal therapies for treating osteoarthritis. – PubMed – NCBI
- Nutraceuticals – Potential for Chondroprotection and Molecular Targeting of Osteoarthritis – 2013
CAM Osteoarthritis – Boswellia serrata (Frankincense)
- Boswellia Serrata, A Potential Antiinflammatory Agent: An Overview
- Oral herbal therapies for treating osteoarthritis. – PubMed – NCBI
- Nutraceuticals – Potential for Chondroprotection and Molecular Targeting of Osteoarthritis – 2013
CAM Osteoarthritis – Devil’s Claw
CAM Osteoarthritis – Diet
CAM Osteoarthritis – DMSO and methylsulfonylmethane (MSM)
- Meta-Analysis of the Related Nutritional Supplements Dimethyl Sulfoxide and Methylsulfonylmethane in the Treatment of Osteoarthritis of the Knee
- Efficacy of methylsulfonylmethane (MSM) in osteoarthritis pain of the knee
- Efficacy of methylsulfonylmethane supplementation on osteoarthritis of the knee – a randomized controlled study
- Systematic review of the nutritional supplements dimethyl sulfoxide (DMSO) and methylsulfonylmethane (MSM) in the treatment of osteoarthritis – PubMed Health
CAM Osteoarthritis – Green-Lipped Mussel extract
CAM Osteoarthritis – Green Tea
CAM Osteoarthritis – L-Carnitine
CAM Osteoarthritis – Resveratrol (see PolyResveratrol)
CAM Osteoarthritis – Salicin
CAM Osteoarthritis – SAMe
CAM Osteoarthritis – Strontium Ranelate
- Efficacy and safety of strontium ranelate in the treatment of knee osteoarthritis
- Strontium ranelate in the treatment of knee osteoarthritis – new insights and emerging clinical evidence
- What about strontium ranelate in osteoarthritis
- Effect of osteoporosis medications on fracture healing. 2016 – PubMed – NCBI
CAM Osteoarthritis – Tai Chi
- Effects of Tai Chi for Patients with Knee Osteoarthritis – A Systematic Review
- Summary of Findings-Tai Chi – 2011
- Tai chi for osteoarthritis – a systematic review 2008 – PubMed Health
CAM Osteoarthritis – Topical Herbal Therapies
CAM Osteoarthritis – Vitamin C
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.
