‘‘Freedom from pain should be a basic human right, limited only by our knowledge to achieve it”
– Melzack R.
Buprenorphine for Pain
It is recommended to first read the following sections to become familiarized with some of the terms and concepts related here:
Also see:
Buprenorphine – Rotating from other opioids to buprenorphine for pain
Buprenorphine Treatment – Emergency and Surgery Pain Management
Buprenorphine in Pregnancy & Breast Feeding
Naloxone (Opioid Blocker)
See also: Buprenorphine for Opioid Substance Use Disorder (SUD)
Definitions and Terms Related to Pain
Key to Links:
Grey text – handout
Red text – another page on this website
Blue text – Journal publication
.
Opioids – Buprenorphine for Pain
Buprenorphine for Pain – A Brief Overview
Buprenorphine is an opioid medication commonly used for treating pain and, because of it’s special characteristics, it is also offers significant potential advantages for pain management over other opioids. While buprenorphine is also commonly used for treating opiate addiction, many people have the mistaken belief that it is used only for addiction which is not the case at all. Buprenorphine also appears to have the advantage of being less likely to develop tolerance to it’s pain benefits compared to many other opioids. Because buprenorphine is different, even those patients with high tolerance that require high doses of opioids such as oxycodone to control their pain usually respond well to buprenorphine for pain control.
Buprenorphine has an extensive set of unique properties that include:
(1) High potency: more potent than morphine, hydrocodone and oxycodone;
(2) Long half-life and slow dissociation from the mu-receptor, providing advantages over other opioids;
(3) Safety advantages over other opioids, including a “ceiling response” to respiratory depressive effects, a benefit that makes buprenorphine potentially the safest opioid with respect to unintentional overdose;
(4) Buprenorphine binds tightly to the mu-receptor (the opioid receptor where all commonly prescribed opioids act to reduce pain);
(5) Buprenorpine offers greater analgesic benefits than some of the other commomly prescribed opioids for certain types of pain including neuropathic pain, deep bone pain and certain cancer-related pains. This may, at least in part, be due to agonist action at the ORL-1 reeceptor;
(6) Buprenorphine reduces depression, probably by blocking the kappa-receptor (another opioid receptor), a property that makes buprenorphine also effective as a mood elevator;
(7) Buprenorphine displays a limited degree of analgesic tolerance that likely stabilizes over time and is often effective for patients who have developed analgesic tolerance to other opioids. This reduced tolerance is thought to, at least in part, be due to it’s agonist action at the ORL-1 reeceptor. This same agonist action at the ORL-1 reeceptor may also be responsible for buprenorphine’s reduced reward effects and likelihood for abuse;
(8) Buprenorpine does not reduce testosterone levels in men or women as can occur with other opioids;
(9) Buprenorpine does not appear to reduce the immune response, a finding of still undetermined significance that appears to occur with some other opioids;
(10) Buprenorpine can be used more safely with those with pancreatitis;
(11) Buprenorphine has less affect on the sphincter of Oddi than many other opioids;
(12) Withdrawal symptoms with buprenorphine are less severe than many other opioids;
(13) Buprenorphine is one of the safest opioids for use in renal failure and dialysis and doses do not have to be altered in mild to moderate liver impairment (Child–Pugh class A and B);
(14) Buprenorphine is better tolerated in the elderly than many other opioids;
(15) Buprenorphine may be given with other opioids and may improve safety in the combination
(16) Buprenorphine appears to reduce the process of central sensitization. Central sensitization often develops with chronic pain, causing magnification of pain perception and reduced tolerance of unpleasant sensory stimulation.
(17) Unlike many other opioids, buprenorphine has not been associated with triggering serotonin syndrome, a condition resulting from excessive levels of serotonin in the nervous system characterized by a flu-like syndrome that is usually mild but can be fatal in severe cases.
Buprenorphine for Pain – the Details
(1) Buprenorphine is a very potent opioid for pain – it is estimated to be approximated 40-135 times as potent, milligram per milligram, when compared to oral morphine, depending on the way it is taken (IV vs sublingual or transbuccal vs transdermal). This is why the dosing of buprenorphine is provided in low doses, starting with fractions of a milligram for patients who have not built significant tolerance to the use of opioids. Buprenorphine produces analgesia with only 5–10% of receptors occupied;
(2) Buprenorphine has a long half-life, meaning that it stays in the body for a long time before it is broken down (metabolized) and/or eliminated, so its effects can last a long time. The analgesic effects of buprenorphine can control pain up to 8-12 hours after a single dose. When a person is physically dependent on opioids, buprenorphine can suppress withdrawal symptoms for up to 48-72 hours after the last dose. Buprenorphine slowly dissociates/detaches from the mu-receptor, a property that also makes the withdrawal symptoms from buprenorphine milder than other opioids.
(3) Buprenorphine also has safety advantages compared with other opioids. All opioids share the property of respiratory depression, in which at higher doses an opioid will suppress the brain’s drive to breathe, resulting in an overdose that can be fatal. A unique beneficial property of buprenorphine is it’s “ceiling effect” with respect to respiratory depression, where there is a limit to the extent in which buprenorphine will suppress the drive to breathe. This property makes it much less likely to result in an accidental overdose, a benefit that may also apply to those with other risks for respiratory depression or reduced oxygenation such as those with sleep apnea, COPD, congestive heart failure or history of stroke. That being said, one is still susceptible to overdose from buprenorphine if taken with high doses of other opioids, alcohol, benzodiazepines or other sedatives such as Soma or barbiturates like Fioricet or Fiorinal.
Buprenorphine is likely safer in the elderly and those with kidney or liver impairment. Only 10-30% of buprenorphine is eliminated via the liver and kidney, the rest is eliminated in the stool. No dosing adjustments are required for those on dialysis (it is not dialyzed) or those who have kidney or liver disease.
(4) Buprenorphine has a strong affinity to the mu-receptor, meaning that it binds tightly to the receptor. Because its binding affinity is stronger than many other currently prescribed opioids, it may displace another opioid already attached to that receptor. When a person who has been on opioids long enough to establish physical dependency, such a displacement of other opioids can precipitate a withdrawal reaction if buprenorphine is given at a high enough dose to displace a significant percentage of another opioid present. This is referred to as a “precipitated opioid withdrawal response” and can complicate the process of rotating from taking another opioid to buprenorphine. For this reason it is important to follow the guidelines established by the prescribing physician to avoid this.
(See: Rotating from other opioids to buprenorphine).
This property of strong affinity of buprenorphine has led to the erroneous belief that taking another opioid for pain while taking buprenorphine will be ineffective. This is not true. Depending on the dose of buprenorphine one is taking, and the percentage of mu-opioid receptors occupied by the buprenorphine, the additional opioid will react with unoccupied receptors for an additive effect. Other variables contributing to the ultimate response of the second opioid include the dose, potency and affinity of the second opioid. Morphine, oxycodone and hydromorphone have all been demonstrated to be effective when added to buprenorpine for pain.
(5) Buprenorphine is more effective for certain types of pain than some other opioids. It is particularly effective in controlling neuropathic (nerve) pain in cancer and non-cancer conditions to a greater extent than many other opioids. Common examples of neuropathic pain include diabetic peripheral neuropathy, shingles, post-radiation pain and sciatica. There is also evidence that buprenorphine may reverse hyperalgesia, a hypersensitivity to pain that may occur with chronic opioid use, a benefit possibly related to buprenorphine blocking kappa-opioid receptors. Buprenorphine also reduces allodynia, the condition in which stimuli such as soft touch or light pressure are inappropriatedly perceived as painful. Both hyperalgesia and allodynia are pain conditions noted to occur in chronic pain patients, especially fibromyalgia patients.
(See Neuropathic Pain)
Buprenorphine is also noted to block central sensitization by multiple mechanisms, thus reducing not only the centrally-induced increased pain associated with long-term chronic pain but also the other sensory sensitivities that may evolve with various chronic pain syndromes.
A study published in 2011 evaluated buprenorphine as compared to fentanyl in the management of deep, bone pain, the type associated with bone trauma and metastatic cancer. This type of pain is often difficult to manage with conventional opioids such as fentanyl. The study revealed buprenorphine to be effective in this type of pain, where fentanyl was not, due to unique characteristics of buprenorphine and its metabolism.
(6) Recent studies indicate that buprenorphine is beneficial for depression, likely by blocking the kappa-receptor (another opioid receptor).
(7) Buprenorphine has multiple mechanisms for reducing pain that often makes it especially effective for patients who have developed analgesic tolerance to other opioids. Aside from its action on the mu-opioid receptors in common with other opioids, it appears to also activate another receptor in the spinal cord that reduces pain, the ORL1 receptor. Buprenorphine also may have another mechanism for reducing pain by direct action in the brain which is not blocked by naloxone, thus it is a mechanism independent of the mu-opioid receptor. Buprenorphine, like other opioids, does display analgesic tolerance but it appears to be limited and it likely stabilizes over time.
(8) Unlike other opioids, buprenorpine does not reduce testosterone levels in men or women. Testosterone is a hormone that plays a role in pain physiology that is not yet well understood. However, it appears to be associated with a greater tolerance for pain and may be a contributing factor to the higher prevalence of chronic pain in women. Some pain conditions such as cluster headaches may also be associated with low levels of testosterone.
(9) Buprenorpine does not appear to impair the immune system, as has been found with some other opioids. Opioids binding to mu-opioid receptors in the brain can activate the descending pathways of the hypothalamo-pituitary-adrenal (HPA) axis, increasing the production of immunosuppressive glucocorticoids (steroids like cortisol) whch have been found to reduce the immune response to stress and may possibly contribute to an increased risk for infection. However, the clinical significance of this reduced immune response is as yet unclear. While not all opioids have demonstrated this effect (tramadol does not, morphine and fentanyl do), buprenorphine may have an advantage over certain other opioids in conditions of reduced immune function.
(10) Buprenorpine can be used more safely with those with acute or chronic pancreatitis. Most opioids are known to cause spasm of the sphincter of Oddi, a muscular valve that controls the flow of digestive juices (bile and pancreatic juice) through ducts from the liver and pancreas into the first part of the small intestine (duodenum). Spasm of the sphincter of Oddi causes back-up of these digestive juices into the gall bladder and pancreas which causes severe abdominal pain, especially in those with pancreatitis. Buprenorphine does not cause spasm of the sphincter of Oddi.
(17) Synthetic opioids such as tramadol, tapentadol (Nucynta), methadone, meperidine (demerol), levorphanol (and dextromethorphan) block serotonin and norepinephrine reuptake. These opioids may be associated with the serotonin syndrome when combined with antidepressants. Fentanyl and oxycodone are also associated with the serotonin syndrome, likely by a mechanism independent of serotonin and norepinephrine reuptake inhibition. Buprenorphine does not block serotonin and norepinephrine reuptake nor is it associated with the serotonin syndrome.
For those interested in learning more about buprenorphine and how it works, based on current research, please see end of document and reference articles below.
Prescribing Information for Safe Use of Buprenorphine
Buprenorphine with other opioids
Buprenorphine has a special characteristic compared with other opioids: it has a very strong binding affinity to the receptors in the nervous system that provide pain control. This means that it may displace other opioids in a patient’s system and this displacement may trigger withdrawal symptoms dependent on a person’s level of physical dependence to their opioids. For this reason it is important that one discuss with their physician how to make the transition from another opioid to buprenorphine before doing so. This strong binding characteristic of buprenorphine also means that when a patient is taking buprenorphine for pain, the addition of other opioids may be less likely to provide significant additional pain benefit. Again, there are a number of variables that come into play here including the dose of buprenorpine one is taking and which additional opioid. However, at lower doses such as those associated with Belbuca (a buccal strip) and Butrans patches, it has been clearly demonstrated that the addition of other commonly prescribed opioids will add analgesic benefit without impairment by the buprenorphine.
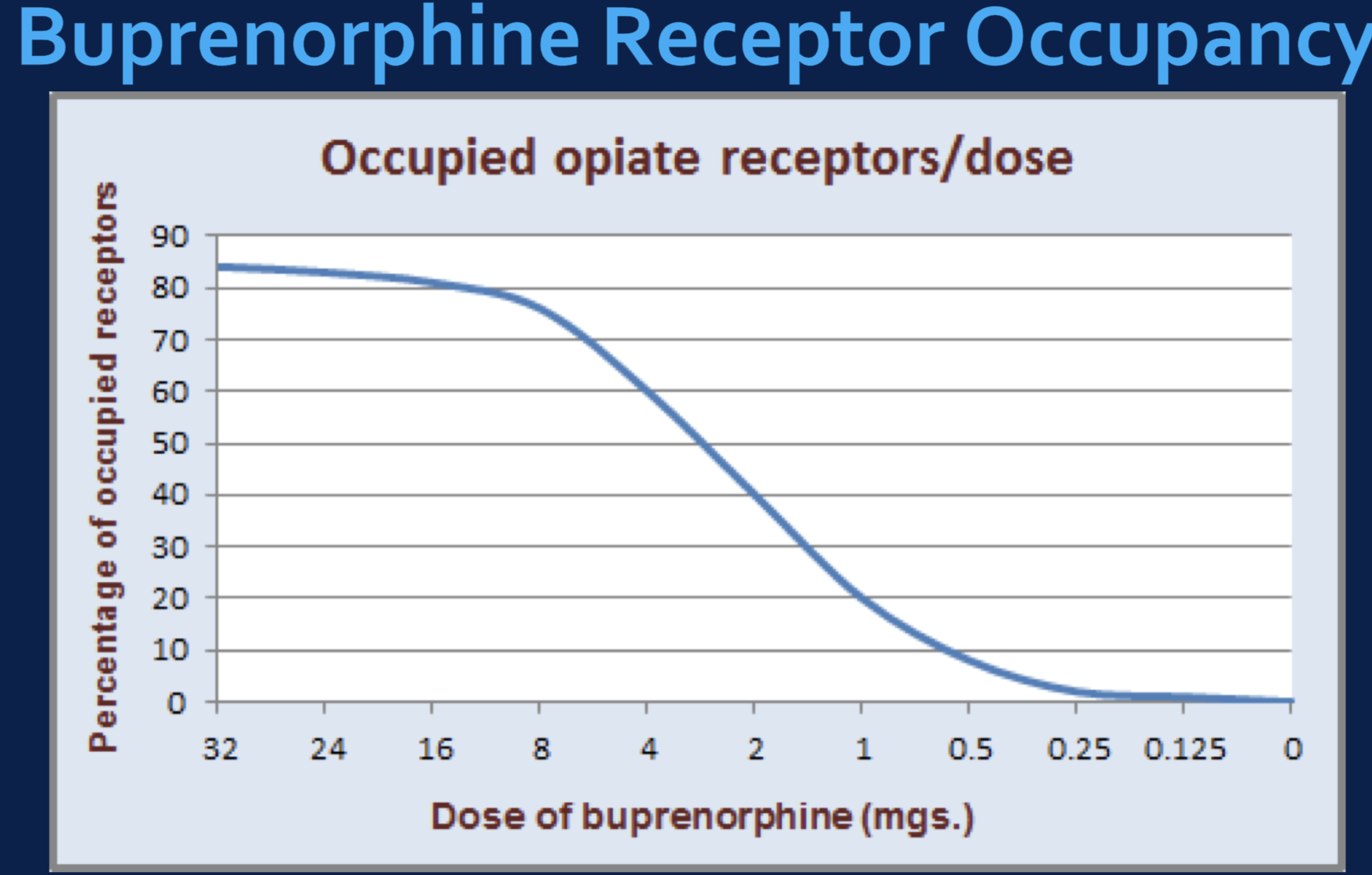
The primary factor determining the potential analgesic benefit of a second opioid added to buprenorphine is the relative degree to which buprenorphine occupies an individual’s mu-opioid receptors. For example, if buprenorphine which binds tightly to the mu-opioid receptors occupies 80-90% of these receptors, the addition of a second opioid is going to have a very limited effect unless that opioid has an even greater binding affinity to the receptors than buprenorphine. This is why high dose buprenorphine (16mg/day) blocks the effects of most opioids because at this dose 80% or more receptors are bound.
In contrast, with dosing with Belbuca even at 900 mcg twice a day, less than 40% of the mu-opioid receptors are occupied, leaving greater than 60% of the receptors available to a second opioid, even one with a weaker binding affinity. See below:
This does not mean, however, that one cannot overdose by adding other opioids while taking buprenorphine. In fact, one can. So it is advised to not take any other opioids while taking buprenorphine for pain unless guided by a physician with special knowledge regarding buprenorphine management. Such circumstances may arise with emergency conditions that are accompanied by severe pain that is not adequately controlled with buprenorphine. If this happens, one must notify the emergency physician that they are taking buprenorphine to facilitate appropriate choices to effectively manage the pain.
See also: Naloxone
Different forms and different brands
Buprenorphine is available as a transdermal skin patch, a tablet designed to dissolve under the tongue or as a film strip designed to dissolve against the side of the cheek. Buprenorphine is available as a stand-alone medication or in combination with naloxone, a non-therapeutic secondary component added only as an abuse deterrent. The stand-alone forms of buprenorphine are FDA-approved for pain while the formulations of buprenorphine with naloxone are FDA-approved only for opioid dependence or addiction. The formulations of buprenorphine with naloxone are sometimes used off label for managing pain in patients with high opioid tolerance.
Due to the popularity of opioid abuse, most opioids coming to market now are accompanied by some form of abuse deterrent and the addition of naloxone, an opioid blocker, is a popular form. The presence of naloxone offers no benefit for pain management but, if the formulation is snorted or injected in an attempt to abuse the medication, the naloxone will trigger an immediate withdrawal syndrome meant to discourage abuse.
Butrans is a transdermal patch form of buprenorphine, designed to be worn for one week then replaced. It is an excellent and convenient means of treating mild to moderate chronic pain. Butrans contains only buprenorphine and comes in five dosage strengths ranging from 5 μg/hr to 20 μg/hr in patches designed to be replaced every 7 days. Butrans is FDA-approved for pain only, not addiction.
Belbuca is a buprenorphine film that is applied to the cheek inside the mouth (buccal area). It contains only buprenorphine and comes in seven dosage strengths ranging from 75 μg to 900 μg, to be dosed every 12 hours. Belbuca provides higher doses than Butrans patches but lower doses than the combination buprenorphine/naloxone tablets and strips (Suboxone, Zubsolv and Bunivail). Belbuca is FDA approved for pain only, not addiction.
Suboxone is the best known form of buprenorphine in combination with naloxone because it is commonly used to manage opioid addiction as a safer alternative to the use of methadone, another opioid used for both pain and addiction. Suboxone, like the other brands of buprenorphine tablets or film strips with naloxone, is FDA approved for addiction treatment and therefore it’s use for pain is considered “off-label.” However, as noted above, buprenorphine as a drug is FDA approved for pain and many medications are commonly used “off-label.” Suboxone is available as a tablet or a film strip in four buprenorphine strengths: 2mg, 4mg, 8mg and 12 mg and is generally dosed every 8-12 hours for pain control.
Subutex is buprenorphine only, in tablet form and like Suboxone it is available in four strengths: 2mg, 4mg, 8mg and 12 mg. Subutex is generally dosed every 8-12 hours for pain control. It is used almost exclusively in pregnancy.
Zubsolv is buprenorphine in combination with naloxone. It is a film strip designed to dissolve under the tongue and comes in two buprenorphine strengths: 1.4mg (a comparable dose to the 2mg Suboxone dose) and 4.2mg (a comparable dose to the 8mg Suboxone dose). The difference in dosing is due to the different bioavailability associated with the different proprietary formulation. Due to the equivavent bioavailable dose with Zubsolv. It ihas been shown that Zubsolv dissolves more quickly than Suboxone and there is less buprenorphine being swallowed where it contributes to risk for constipation.
Bunavail is buprenorphine in combination with naloxone. It is a film strip designed to adhere to the cheek, then dissolve. It comes in three buprenorphine strengths: 2.1 mg (a comparable dose to the 4 mg Suboxone dose), 4.2 mg (a comparable dose to the 8mg Suboxone dose) and 6.3 mg (a comparable dose to the 12mg Suboxone dose. The difference in dosing is due to the different bioavailability associated with the different proprietary formulation.
Advantages of Bunavail
Bunavail is designed differently from Suboxone and Zubsolv. Rather than the single layer design, it is a bilayered film that promotes unidirectional drug flow across the buccal mucosa (lining of the cheek), allowing for less buprenorphine dissolving into saliva and more of it going into the blood through the cheek. Consequently, because less buprenorphine is wasted into saliva and swallowed, a smaller dose strip can be used with equal amounts of buprenorphine entering the blood.
Thus, while an equal amount of buprenorphine enters the blood compared with the other formulations, less buprenorphine enters the stomach and intestines. When buprenorphine enters the stomach and intestine, it is absorbed and transported to the liver which metabolizes the buprenorphine into norbuprenorphine, its primary metabolite. In a recent 2016 study, it was determined that norbuprenorphine blood levels were 40% lower with Bunavail compared with the sublingual preparations.
Norbuprenorphine is bioactive like buprenorphine but with different characteristics. Because it is a full mu-opioid agonist unlike buprenorphine, a partial mu-opioid agonist, norbuprenorphine has greater activity related to the mu-opioid receptor resulting in greater constipation effect. For this reason, the higher norbuprenorphine levels associated with Suboxone and Zubsolv compared with Bunavail are associated with more likelihood of constipation. Therefore, if one experiences constipation with Suboxone or Zubsolv, a trial of Bunavail is warranted.
Another advantage of the buccal adherence to the cheek is the relative immediacy one can proceed to speak without waiting for a tab or strip to dissolve under the tongue.
Disadvantage of Bunavail
Because blood levels of norbuprenorphine are lower at comparable blood levels of buprenorphine with Bunavail compared with Suboxone and Zubsolv, it is likely that Bunavail does not have as much analgesic benefit due to the analgesic contribution of norbuprenorphine. This conclusion is speculative, however, with no definitive studies comparing analgesic benefits between the three versions.
Each proprietary formulation tastes different, with each taste appealing more or less to the individual.
What is the most important information I should know about taking Buprenorphine?
- Buprenorphine can cause death from overdose, especially if you take them with other opioid, alcohol or sedatives such as Xanax, Valium or Klonopin. Use Buprenorphine exactly the way your doctor tells you to with medicines used to treat depression or anxiety.
- Use Buprenorphine only for the condition for which it was prescribed.
- Buprenorphine can cause drug dependence. This means that you can get withdrawal symptoms if you stop using it too quickly. Buprenorphine is not for occasional (“as needed”) use.
- Getting off buprenorphine can be accomplished without serious difficulty. The reason it sometimes has the reputation of being difficult to taper off is that the tapering is often not done correctly. Buprenorphine is a potent opioid that should be tapered slowly; you should not simply stop taking it abruptly when you get down to a 1 or 2mg/day dose. Use of alternative buprenorphine formulations and tapering regimens can be engaged to make the final taper smooth and well tolerated. There is growing research to suggest that the use of gabapentin (Neurontin) may ease opioid withdrawal symptoms (See: Gabapentin). For other ways of managing opioid withdrawal, See Opioid Withdrawal.
- Prevent theft and misuse. Buprenorphine is a narcotic painkiller that can be a target for people who abuse prescription medicines or street drugs. Keep your buprenorphine locked in a safe place, to protect them from theft. Never give them to anyone else. Selling or giving away this medicine is against the law.
- In an emergency, have family members tell emergency room staff that you are being treated with buprenorphine, especially if being treated for a severely painful condition. Buprenorphine binds very tightly to the opioid receptors (see: Neurobiology of Opioids) that provide pain relief, more than most other opioids including hydrocodone, oxycodone and morphine. This means that in the event of an emergency that requires opioids for pain not controlled by currently prescribed buprenorphine, the emergency physician should use the best opioid for pain or the buprenophine may impair the effectiveness of the second opioid. There are multiple variables that will contribute to how effective a second opioid will be for the patient currently taking buprenorphine. Ineffectiveness may be misinterpreted as drug-seeking by a physician not well informed regarding treating pain in patients who take buprenorphine. Perhaps the best opioids for emergency use for managing pain in this emergency circumstance are fentanyl and hydromorphone (Dilaudid), either orally or intravenously. Because only fentanyl has greater affinity for the opioid receptor than buprenorphine, it should be effective for pain and may be the best option under these circumstances. That being said, caution is advised to avoid unintentional overmedication/overdose and careful monitoring should be employed. Whenever possible, always contact Dr. Ehlenberger (24/7) should you need to go to the emergency room for any condition, but especially for a painful condition.
Who Should Not Take Buprenorphine?
Do not take buprenorphine if:
- Your doctor did not prescribe buprenorphine for you.
- You are allergic to buprenorphine, or any of the inactive ingredients in the medicines. See the end of the enclosed prescribing leaflet for a complete list of ingredients.
Your doctor should know about all your medical conditions before deciding if buprenorphine is right for you or what dose is best. Tell your doctor about all of your medical problems, especially the ones listed below:
- Trouble breathing or lung problems
- Head injury or brain problem
- Liver or kidney problems
- Gallbladder problems
- Adrenal gland problems, such as Addison’s disease
- Low thyroid (hypothyroidism
- Enlarged prostate gland (men)
- Problems urinating
- A curve in your spine that affects your breathing
- Severe mental problems or hallucinations (seeing or hearing things that are not really there
- Alcoholism
Tell your doctor:
- if you are pregnant or plan to become pregnant. Buprenorphine may not be right for you. It is not known whether buprenorphine could harm your baby.
- if you are breast feeding, buprenorphine will pass through your milk and may harm your baby.
- Tell your doctor about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. They may cause serious side effects when taken with buprenorphine. Sometimes, the doses of certain medicines and buprenorphine need to be reduced if used together.
- Do not take any other medicine, herbal, or over-the-counter medicine while using buprenorphine unless your doctor has told you it is okay.
How should I take Buprenorphine?
- Follow your doctor’s directions exactly. Your doctor may change your dose after seeing how the medicine affects you. Do not change your dose unless your doctor tells you to change it. Do not take buprenorphine more often than prescribed.
- Put the tablets or film under your tongue or against the cheek as directed and let them melt. This will take 2 to 10 minutes. Do not chew or swallow the tablets. The medicine will not work this way and you may get withdrawal symptoms.
- If your doctor tells you to take more than 1 tablet/film, you will be told to:
- Take all tablet/films at the same time together under your tongue, or
- Take 1 tablet/films, put it under your tongue. After it melts, put the next tablet/film under your tongue right away
- Hold the tablet/film under your tongue until it melts completely. The medicine will not work if swallowed and you may get withdrawal symptoms.
- Do not change the way you are told to take your medicine or you may get too little or too much medicine.
- Do not inject (“shoot-up”) or snort buprenorphine. Shooting-up is dangerous and you may get bad withdrawal symptoms.
- Buprenorphine can cause withdrawal symptoms if you take them too soon after using opiate drugs like morphine, oxycodone, hydrocodone or methadone.
- If you miss a dose of buprenorphine, take it as soon as possible. If it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not take 2 doses at once unless your doctor tells you to.
- Before discontinuing buprenorphine, ask your doctor how to avoid withdrawal symptoms.
- If you take too much buprenorphine or overdose, call your local emergency room or poison control center ASAP.
- If you discontinue taking buprenorphine, flush the unused tablets or strips down the toilet.
What Should I Avoid While Taking Buprenorphine?
- Do not drive, operate heavy machinery, or perform other dangerous activities until you know how this medicine affects you.
- Do not drink alcohol or take benzodiazepine tranquilizers or barbiturate sedatives (including butalbital (Fioricet or Fiorinal) at high doses) while using buprenorphine. Overdose and even death may occur when you use these medications with buprenorphine.
- Do not take other medicines without talking to your doctor. Other medicines include prescription and non-prescription medicines, vitamins, and herbal supplements. Be especially careful about medicines that may make you sleepy.
Potential Drug Interactions
There may also be a potential for buprenorphine interactions with other drugs and compounds that induce or inhibit the cytochrome P-450 3A4 system, the enzyme system in the liver that metabolizes buprenorphine. There are many agents in this category and they include erythromycin, grapefruit juice and starfruit (inhibitors of metabolism), as well as carbamazepine, phenobarbital, phenytoin, and rifampin (inducers that enhance metabolism). In a study of the effects of the selective serotonin reuptake inhibitors (SSRIs), fluoxetine (Prozac) and fluvoxamine (Luvox), were both shown to inhibit buprenorphine metabolism, suggesting they may increase blood levels of buprenorphine if started by someone already taking buprenorphine.
What are the Possible Side Effects of Buprenorphine?
Some of the common side effects of buprenorphine are headache, drowsiness, problems sleeping, nausea, sweating, stomach pain, and constipation.These are not all the possible side effects of buprenorphine, just some of the most common.
Call your doctor or get medical help right away if:
- You feel faint, dizzy, confused, or have any other unusual symptoms.
- Your breathing gets much slower than is normal for you. These can be signs of an overdose or serious problem.
- Buprenorphine can cause your blood pressure to drop, causing dizziness if you get up too fast from sitting or lying down.
- Buprenorphine can cause allergic reactions that can make it hard for you to breathe. Other symptoms of a bad allergic reaction include hives, swelling of your face, asthma (wheezing) or shock (loss of blood pressure and consciousness).
Call a doctor or get emergency help right away if you get any of these symptoms.
Buprenorphine may cause liver problems. Call your doctor right away if:
- Your skin or the white part of your eyes turns yellow (jaundice).
- Your urine turns dark.
- Your bowel movements (stools) turn light in color.
- You don’t feel like eating much food for several days or longer.
- You feel sick to your stomach (nausea).
- You have lower stomach pain.
Your doctor will do blood tests while you are taking buprenorphine to make sure your liver is okay.
Other considerations:
- You may get withdrawal symptoms when you start treatment with buprenorphine. To avoid this, be sure other opiates are out of your system before starting buprenorphine.
- Like with all opiates, you can develop dependence from taking buprenorphine, so you may get withdrawal symptoms when you stop taking buprenorphine. There is also a chance that you may abuse or get addicted to buprenorphine. The risk of addiction to buprenorphine is very low and dependent on many factors related to an individual. If you have any concerns about developing addiction to buprenorphine, please discuss them with your physician.
Genetic Testing
At Accurate Clinic we highly recommend genetic testing for our opioid patients. Through testing our patient’s DNA with a simple oral swab of saliva from the cheek, an individual’s ability to metabolize opioids and other medications by the liver can be evaluated. This information provides important insights as to how a patient may respond to various medications, including buprenorphine, and where side effects or drug interactions may be predicted, allowing for substantial safety benefits in prescribing.
In addition, genetic testing for addiction risk is also recommended and available. Ideally, genetic testing for addiction should be performed on all patients prescribed medications that pose risk for addiction. It is highly recommended for patients with a family history of addiction and thoee individuals with high risk for addiction. The results of these tests may be used to identify specific addiction risks as well as means of reducing these risks. (See Genetic Testing for Addiction Risk).
Neurobiology of Buprenorphine – for those interested in understanding more…
As noted above, buprenorphine has characteristics that make it particularly effective in managing certain types of pain. This is because buprenorphine has different mechanisms of action than conventional opioids (see Neurobiology of Opioids). Buprenorphine has a unique and complex pharmacology, acting as an agonist at μ-opioid receptor (MOR), δ-opioid receptors (DOR), ORL-1 (NOP) receptors and as an antagonist and as an inverse agonist at the κ-opioid receptor (KOR).
The action of buprenorphine as a partial agonist of the MOR provides both an analgesic benefit as well as a ceiling effect on respiratory depression, resulting in a safer opioid with respect to overdose. Its activity as an antagonist of the KOR likely contributes to its benefit with mood and depression. Buprenorphine has also been identified as an inverse agonist at the kappa receptor which may explain buprenorphine-associated antihyperalgesic activity, as hyperalgesia is likely the result of dynorphin upregulation. It is also a reason why there is less sedation and dysphoria with buprenorphine.
Additionally, buprenorphine’s effect on the ORL- 1 opioid receptor dampens the brain reward system and that implies less tolerance and less reward which is responsible for the beneficial effects of buprenorphine in the treatment of opioid abuse.
It was recently discovered that buprenorphine’s affinity for a newly discovered structurally distinct subtype of the mu receptor is involved in buprenorphine’s analgesia that definitively distinguishes buprenorphine. Both morphine and methadone act through traditional full-length mu receptors but, in contrast, buprenorphine analgesia also depends on the arylepoxamide receptor (AEAr) in the brain.
The arylepoxamide receptor has a shortened 6-transmembrane protein from the mu opioid receptor gene (OPRM-1). Studies in mice lacking this protein showed no buprenorphine-induced analgesia, while showing normal responses to morphine. This unique receptor selectivity may account for its incomplete analgesic cross-tolerance. Similar to buprenorphine, both nalbuphine and butorphanol are dependent on the AEA receptor and they also have a ceiling effect on respiratory depression.
When opioids interact with a receptor such as the OPEM-1 receptor on a cell membrane, it triggers a response (signaling) by interacting with that receptor in which subsequent chemical actions such as via G-protein pathways with the cell occur, a process called transduction. Biased signaling, in which opioids differentially activate various transduction systems, is important in understanding opioid pharmacology. Analgesia is associated with G-protein pathways, while arrestin recruitment is associated with many of the opioid-related adverse effects including respiratory depression, analgesic tolerance and constipation. Unlike traditional opioids such as morphine, fentanyl and methadone, buprenorphine does not recruit β-arrestin to the receptor. Additionally, this may account for super-additive effects when combining low-dose buprenorphine with fentanyl, oxycodone, and morphine.
When Buprenorphine Doesn’t Work for Pain
Unfortunately, buprenorphine doesn’t always work for pain in everyone. Research suggests that a genetic variant, the N40D variant, may be responsible for those patients who do not respond to buprenorphine for pain and need rotation to another opioid in order to achieve adequate pain control. The N40D variant is the most common MOR receptor variant, an A > G substitution at nucleotide 118, and is present in 10-50% of the population and the efficacy of buprenorphine associated with this variant may be reduced by >50%.
A decrease in buprenorphine efficacy arising from the N40D variant could be a contributing factor for the lack of response of some individuals to buprenorphine maintenance therapy and may predict a significantly inadequate or inappropriate analgesic response in a large proportion of the population.
References:
Buprenorphine – Patient Information
- Buprenorphine Transdermal Patch: MedlinePlus Drug Information
- Buprenorphine – for Pain, Informed Consent
Buprenorphine – Overviews
- Buprenorphine – StatPearls – NCBI Bookshelf 2019
- Managing Opioid Withdrawal in the Emergency Department With Buprenorphine – 2019
- Buprenorphine – Considerations for Pain Management
- Sublingual Buprenorphine:Naloxone for Chronic Pain in At-Risk Patients – Development and Pilot Test of a Clinical Protocol
- Is Levorphanol a Better Option than Methadone – 2015
- Transdermal buprenorphine in clinical practice: a multicenter, noninterventional postmarketing study in the Czech Republic. – PubMed – NCBI
- clinical-update-on-the-pharmacology-efficacy-and-safety-of-transdermal-buprenorphine-pubmed-ncbi
- opioids-and-the-management-of-chronic-severe-pain-in-the-elderly-consensus-statement-of-an-international-expert-panel-with-focus-on-the-six-clinic-pubmed-ncbi
- buprenorphine-an-attractive-opioid-with-underutilized-potential-in-treatment-of-chronic-pain-2015
- twelve-reasons-for-considering-buprenorphine-as-a-frontline-analgesic-in-the-management-of-pain-pubmed-ncbi
- the-clinical-analgesic-efficacy-of-buprenorphine-pubmed-ncbi
- current-knowledge-of-buprenorphine-and-its-unique-pharmacological-profile-pubmed-ncbi
- equipotent-doses-of-transdermal-fentanyl-and-transdermal-buprenorphine-in-patients-with-cancer-and-noncancer-pain-results-of-a-retrospective-cohor-pubmed-ncbi
- transdermal-buprenorphine-in-cancer-pain-and-palliative-care-pubmed-ncbi
- safety-and-effectiveness-of-intravenous-morphine-for-episodic-breakthrough-pain-in-patients-receiving-transdermal-buprenorphine-pubmed-ncbi
- evaluation-of-the-tolerability-of-switching-patients-on-chronic-full-l-opioid-agonist-therapy-to-buccal-buprenorphine-2016
- buprenorphine-naloxone-therapy-in-pain-management-2014
- efficacy-and-tolerability-of-buccal-buprenorphine-in-opioid-experienced-patients-with-moderate-to-severe-chronic-low-back-pain-2016
- management-of-moderate-to-severe-chronic-low-back-pain-with-buprenorphine-buccal-film-using-novel-bioerodible-mucoadhesive-technology-2016
- the_clinical_analgesic_efficacy_of_buprenorphine
- effect-of-transdermal-opioids-in-experimentally-induced-superficial-deep-and-hyperalgesic-pain-2011
- a-clinical-trial-comparing-tapering-doses-of-buprenorphine-with-steady-doses-for-chronic-pain-and-co-existent-opioid-addiction-2010
- Twelve Reasons for Considering Buprenorphine as a Frontline Analgesicin the Management of Pain – 2012
- The switch from buprenorphine to tapentadol – is it worth? – 2016
- Buprenorphine signalling is compromised at the N40D polymorphism of the human μ opioid receptor in vitro – 2014
- Treating Chronic Pain – An Overview of Clinical Studies Centered on the Buprenorphine Option – 2018
- Understanding Buprenorphine for Use in Chronic Pain – Expert Opinion – 2020
- A Narrative Pharmacological Review of Buprenorphine – A Unique Opioid for the Treatment of Chronic Pain – 2020
Buprenorphine – Constipation
- Opioid-induced constipation_ rationale for the role of norbuprenorphine in buprenorphine-treated individuals – 2016
- Comparison of Pharmacological Activities of Buprenorphine and Norbuprenorphine – Norbuprenorphine Is a Potent Opioid Agonist – 2001
Buprenorphine – Drug Interactions
Buprenorphine – Opioid Tolerance, Hyperalgesia and NMDA Antagonism
- Buprenorphine – a review of its role in neuropathic pain
- Buprenorphine for neuropathic pain–targeting hyperalgesia. – PubMed – NCBI
- Transdermal buprenorphine controls central neuropathic pain. – PubMed – NCBI
- Pharmacologic Treatments for Neuropathic Pain
- Low-dose buprenorphine infusion to prevent postoperative hyperalgesia in patients undergoing major lung surgery and remifentanil infusion a double-blind, randomized, active-controlled trial – 2017
Buprenorphine – Neurobiology
- Buprenorphine signalling is compromised at the N40D polymorphism of the human opioid receptor in vitro – 2014
- Classics In Chemical Neuroscience – Buprenorphine – 2020
Buprenorphine – Kidney Stone Pain
Buprenorphine – Genetics
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.