Acupuncture:
Chemotherapy-Induced Peripheral Neuropathy (CIPN)
- See:
- Traditional Chinese Medicine (TCM)
- TCM – Chinese Herbal Medicine (introduction)
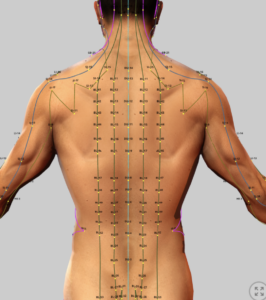
- TCM – Acupuncture (introduction)
- Acupuncture – Migraine Headaches
- Acupuncture – Trigger Point & Myofascial Pain
- Acupuncture – Osteoarthritis
- Acupuncture – Peripheral Neuropathy (Overview)
- Acupuncture – Diabetic Peripheral Neuropathy (DPN)
- Acupuncture – Chemotherapy-Induced Peripheral Neuropathy (CIPN)
- Acupuncture – Sciatica
- Acupuncture – Fibromyalgia
- Acupuncture – Mechanisms of Actions
- Acupuncture – Transition from Acute to Chronic Pain
Nutraceuticals:
Acupuncture:
Chemotherapy-Induced Peripheral Neuropathy (CIPN)
Chemotherapy-induced peripheral neuropathy (CIPN) is a common side effect of cancer treatments, affecting 30–68% of patients receiving drugs like taxanes or platinum agents. It causes numbness, tingling, and burning pain in the hands and feet, often with weakness or digestive issues, significantly reducing quality of life and sometimes leading to reduced chemotherapy doses or treatment cessation.
While duloxetine (Cymbalta) offers moderate pain relief for many, its side effects that sometimes includes fatigue and nausea limits its use for some patients. Other drugs, such as gabapentin, pregabalin (Lyrica0 often show little benefit for CIPN. For this reason, many turn to acupuncture as a means of helping them with their pain and other symptoms associated with CIPN.
Before proceeding to explore acupuncture management of CIPN, a brief review of the syndrome associated with CIPN will be provided here that will explore its pathophysiology, current management and emerging treatments, including a focus on pharmacological, non-pharmacological, and nutraceutical approaches, particularly relevant for neuropathic pain management.
Pathophysiology and Treatment oF CIPN
Objective
Mattar et al. (2024) provide a comprehensive review of The article details CIPN’s pathophysiology, current management, and emerging treatments, with a focus on pharmacological, non-pharmacological, and nutraceutical approaches, particularly relevant for neuropathic pain management.
Key Findings
Introduction
- Epidemiology: CIPN affects 30–40% of chemotherapy patients annually (19–85% prevalence), with 70% of paclitaxel and 90% of oxaliplatin patients affected. Symptoms persist in ~30% at 6 months, sometimes worsening (“coasting phenomenon”).
- Symptoms: Sensory (tingling, numbness, burning pain), motor (weakness, coordination issues), and autonomic (sweating, digestive problems) symptoms in a glove-and-stocking distribution, reducing QOL and causing economic burdens ($15–$1,425 monthly drug costs, job loss).
- Challenges: No FDA-approved agents for CIPN prevention. Duloxetine is the only moderately effective treatment. Non-pharmacological approaches (e.g., acupuncture, exercise) offer relief but lack guidelines.
Pathophysiology
- Mechanisms:
- Cytoskeleton Changes: Paclitaxel/vincristine disrupt microtubule networks, impairing axonal transport and causing sensory neuron damage.
- Oxidative Stress: Platinum agents increase reactive oxygen species (ROS) via mitochondrial DNA damage. Taxanes alter mitochondrial membrane permeability, releasing calcium and causing neuronal dysfunction.
- Ion Channel Dysfunction: Upregulation of NaV/CaV channels and downregulation of Kv channels increase neuronal excitability.
- Immunological Responses: Chemotherapy activates astrocytes/TLR-4, increasing pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) and reducing IL-10.
- Microtubule Disruption: Taxanes/vinca alkaloids impair tubulin polymerization, affecting nerve regeneration.
- Relevance: These mechanisms guide targeted therapies, including nutraceuticals that reduce oxidative stress and inflammation.
Current Management
- Pharmacological: Duloxetine (off-label) reduces pain via serotonin/norepinephrine reuptake inhibition and anti-inflammatory effects (p38, NF-κB).
- Non-Pharmacological: Acupuncture, exercise, mindfulness, yoga, and touch therapies (acupressure, massage) reduce symptoms and improve QOL, with limited evidence.
- Nutraceuticals/Herbs: Nutrients and Chinese herbal medicines show potential but lack clinical guidelines.
Emerging Treatments
- SNRIs: Venlafaxine reduces pain but is less effective than duloxetine. Topical amitriptyline reduces pain; systemic use ineffective.
- Ion Channel Therapies: Lidocaine reduces pain (~23 days). Gabapentin/pregabalin show limited efficacy.
- Anti-Inflammatory: Metformin (500 mg thrice daily) protects against oxaliplatin-induced neuropathy by reducing IL-6, TNF-α, and nociception. Minocycline reduces pain in some studies but not fatigue/numbness.
- Antioxidants: Calmangafodipir delays CIPN onset and reduces cold allodynia. Amifostine protects against oxaliplatin-induced neurotoxicity but not cisplatin/paclitaxel.
- Sigma-1 Receptor Antagonists: MR309 reduces cold allodynia and hyperexcitability.
- Cannabinoids: Oral CBD (300 mg/day) and topical CBD/THC reduce pain and cold sensitivity. Preclinical agonists reduce hypersensitivity.
- Herbal Medicines: Divya-Peedantak-Kwath, Goshajinkigan, ginger, Danshen, and Commiphora myrrha reduce inflammation and allodynia.
- Nutraceuticals (Emphasized):
- Nicotinamide Riboside (NR): Suppresses tactile/cold hypersensitivity in paclitaxel-induced CIPN by increasing NAD+ levels, preventing intraepidermal nerve fiber loss, and normalizing sirtuin Z-mediated tubulin deacetylation, offering a novel approach for neuropathic pain management.
- N-acetylcysteine, α-Lipoic Acid, Vitamin C, Vitamin E: Reduce ROS and neuroinflammation in oxaliplatin-induced CIPN, supporting their role in mitigating oxidative stress-related neuropathy, relevant to central sensitization.
- Magnolin: Reduces cold allodynia by inhibiting ERK activation, providing a targeted nutraceutical option for CIPN symptom relief.
- Other Targets: PPARγ activators, AMPK, and microRNA pathways show preclinical promise.
Discussion
- Key Points: CIPN requires individualized protocols. Nutraceuticals (e.g., NR, α-lipoic acid) show promise for reducing oxidative stress and inflammation, complementing pharmacological and non-pharmacological therapies. Prevention and safer chemotherapy drugs are critical.
- Future Directions: Prioritize prophylaxis, target calcium/magnesium channels, and combine therapies to enhance QOL, with nutraceuticals as key adjuncts.
Implications
CIPN’s impact on QOL necessitates effective management. Duloxetine offers moderate pain relief, while acupuncture and nutraceuticals (e.g., NR, α-lipoic acid) provide safe, complementary options. For physicians at Accurate Clinic, nutraceuticals offer novel mechanisms for neuropathic pain, aligning with central sensitization strategies. Patients can expect reduced symptoms and improved QOL, supporting cancer survivorship.
Limitations
Lack of FDA-approved treatments, insufficient data on emerging therapies, and variable efficacy of complementary approaches. Larger, well-designed trials are needed.
References
- Mattar et al. (2024). Life. DOI: 10.3390/life14080991
Summary of Acupuncture for CIPN
Acupuncture has emerged as a safe and effective option to relieve CIPN symptoms, improve nerve function, and enhance quality of life. This summary reviews three systematic research publication reviews of acupuncture’s role in CIPN treatment.
Key Findings
- Acupuncture Reduces Pain and Symptoms: Across 49 randomized controlled trials (RCTs) involving 3,218 patients, acupuncture significantly reduced pain, severity of CIPN sensory symptoms like numbness and tingling), particularly for mild to moderate cases. It outperforms vitamin B, vitamin B12 and neurotrophic drugs like gabapentin and Lyrica in improving symptoms.
- Improves Nerve Function: Acupuncture enhances nerve conduction velocity (NCV), with stronger effects on motor nerves than sensory nerves and supports recovery of nerve function damaged by chemotherapy.
- Enhances Quality of Life: Acupuncture improved CIPN-specific quality of life with additional benefits for chemotherapy-related symptoms like nausea and fatigue, indicating broader systemic effects.
- Electroacupuncture’s Role: Electroacupuncture (EA) shows superior efficacy in some studies, particularly when combined with glutathione or vitamin B12, but may worsen pain in severe CIPN cases, suggesting traditional acupuncture as a safer option for some patients.
- Safety: Acupuncture and EA reported minimal adverse events, such as mild bruising, making them safe options for patients seeking alternatives to medications with side effects.
Summary
Patients may expect reduced symptoms and improved daily functioning with low-risk acupuncture therapy, especially those with sensory symptoms and those unable to tolerate duloxetine. .
Limitations
Research evidence is limited by small sample sizes, lack of blinding in many studies, and variability in treatment protocols and outcome measures, which complicates comparisons. No studies compared acupuncture directly to duloxetine, and long-term effects remain unstudied, necessitating cautious interpretation.
Recommendations
Acupuncture should be considered a first-line complementary therapy for CIPN, particularly for mild to moderate sensory symptoms.
References
- Li et al. (2024). Frontiers in Neurology. DOI: 10.3389/fneur.2024.1351228
- Jin et al. (2020). DOI not provided.
- Pei et al. (2023). Acupuncture in Medicine. DOI: 10.1177/09645284221076512
References
Acupuncture – Diabetic Peripheral Neuropathy (DPN)
- Acupuncture in Patients with Diabetic Peripheral Neuropathy-Related Complaints- A Randomized Controlled Clinical Trial – 2023
- Research trends of acupuncture therapy for painful peripheral nervous system diseases from 2004 to 2023- a bibliometric and meta-analysis – 2025
Acupuncture – Chemotherapy-Induced Peripheral Neuropathy (CIPN)
- Research trends of acupuncture therapy for painful peripheral nervous system diseases from 2004 to 2023- a bibliometric and meta-analysis – 2025
- Acupuncture in the treatment of chemotherapy-induced peripheral neuropathy- a meta-analysis and data mining – 2024
- Chemotherapy-Induced Peripheral Neuropathy- A Recent Update on Pathophysiology and Treatment – 2024
- Corrigendum- Exercise for reducing chemotherapy-induced peripheral neuropathy- a systematic review and meta-analysis of randomized controlled trials – 2024
- The effectiveness and safety of acupuncture_electroacupuncture for chemotherapy-induced peripheral neuropathy_ a systematic review and meta-analysis – PubMed – 2023
- Acupuncture for chronic pain- update of an individual patient data meta-analysis – 2018
Acupuncture – Other
- Pain management with acupuncture in osteoarthritis – A systematic review and meta-analysis
- Mechanism of Traditional Chinese Medicine in Treating Migraine- A Comprehensive Review
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
.
