“It takes but one positive thought when given a chance to survive and thrive to overpower an entire army of negative thoughts. “
– Robert H. Schuller
Neurobiology of Pain:
Surgical Pain – Post-Operative
Aside from concerns regarding impairment or loss of function after surgery, most people’s primary concern for surgery revolves around pain and it’s effective management. This is especially true for patients who already suffer from chronic pain. This population has been shown to be hypersensitive to pain and require higher doses of opioids to manage their post-operative pain.
Another common and important concern is the potential for surgery to result in a new or worsened chronic pain. The following is directed at addressing these concerns and what can be done to improve outcomes.
See:
- Considering Spine Surgery?
- Coordinating Post-Operative Pain Management with the Surgeon or Dentist
- Central Sensitization
- Opioid-Induced Hyperalgesia (OIH)
- Neurobiology of Pain
see also:
- Journavx (suzetrigine)
- Gabapentin & Lyrica
- Palmitoylethanolamide (PEA)
- Dextromethorphan
- Ketamine
- Levorphanol
Definitions and Terms Related to Pain
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
Considerations in the Management of Post-Operative Pain
The decision to undergo surgery is clearly a very important one that often has major impact on one’s quality of life post-operatively. Arguably, the importance of this decision is paralleled by the importance of preparing one’s self for managing post-operative pain, not just to avoid the acute pain immediately in the post-operative period but more importantly to reduce the risk and/or severity of chronic post-surgical pain.
Acute Post-Operative Pain
It has been reported that postoperative pain is inadequately managed in greater than 80% of patients in the US, although rates vary depending on type of surgery performed and analgesic and anesthetic used. According to the US Institute of Medicine, 80% of patients who undergo surgery report post-operative pain, with 88% of these patients reporting moderate, severe, or extreme pain levels. In a national US survey of 300 adults who had undergone surgery within the previous 5 years, 86% of patients experienced post-surgical pain overall, and 75% of those who reported pain described its severity as moderate–extreme during the immediate post-operative period.
Pain has an adverse effect on post-operative recovery beyond the simple element of suffering. Poorly controlled acute post-operative pain is associated with increased exposure to additional medications and their potential complications including prolonged duration of opioid use. In addition, it is associated with functional and quality-of-life impairment, delayed recovery time and longer hospital stays with higher health-care costs. Furthermore, the presence and intensity of acute pain during or after surgery increases the risk of the development of chronic pain.
For these reasons, it is important to understand the different variables that contribute to post-operative pain.
Contributing Factors in Acute Post-Operative Pain
Type of Surgery
One variable, of course, is the type of surgery. For example, it has been reported that the pain occurring after total knee arthroplasty (TKA) is more painful than that of any other orthopedic surgery, including total hip arthroplasty. Pain scores on the first postoperative day are highest after obstetric and orthopedic/traumatic procedures, but scores are high after even common minor surgical procedures, such as appendectomy, cholecystectomy, hemorrhoidectomy, tonsillectomy, and some laparoscopic procedures.
Nutritional Status and Oxidative Stress
Other variables that come into play impacting the severity of post-surgical pain include the nutritional status of the patient going into surgery. Obviously, vitamin and other nutritional deficiencies may contribute to poor healing which can enhance pain but additionally patients with increased oxidative stress and systemic inflammation are more at risk for increased post-surgical pain.
See: Oxidative Stress
Pre-Operative Pain
The presence of pain pre-operatively, especially chronic pain, is a factor that contributes to both acute as well as chronic post-surgical pain. Additionally, certain chronic pain conditions associated with neuropathic pain and central sensitization such as chronic migraine headaches, fibromyalgia, chronic regional pain syndrome (CRPS) are more likely to suffer increased post-operative pain. While neuropathic pain is widely considered a chronic pain state, neuropathic pain can occur acutely and can be a component of postoperative pain. Also, there is evidence that the effectiveness of management of pre-operative pain may impact the severity of post-operative pain.
Psychological and Psychiatric States
The importance of a patient’s psychological state prior to surgery is a significant factor in predicting risk for post-surgical pain. Conditions that predispose to increased post-operative pain include depression, anxiety and pain catastrophizing.
Anesthetic Agents
Also, there is evidence that the choice of anesthetic agents during surgery may contribute to risk for chronic post-operative pain (See below).
Ways to Reduce Acute Post-Operative Pain
There are a number of things one may do to reduce acute post-surgical pain. Because there is significant overlap in how to reduce both acute and chronic post-operative pain, the discussion of the methods will be reviewed below. However, what is most important to understand, is that the most significant, consistent factor contributing to the risk of progression of acute to chronic post-surgical pain is the duration of severe acute postoperative pain which can lead to central sensitization.
Vitamin C
There is growing research that suggests that Vitamin C is effective in reducing post-operative pain. The mechanism of Vitamin C for reducing pain intensity is not yet fully understood. Based on a review of literature, one factor in the generation of pain, especially persistent, recurrent, or neuropathic pain, is presence of reactive oxygen species (ROS) such as superoxide and certain free radicals. These compounds can be neutralized or reduced by antioxidants, including Vitamic C which has established neuroprotective and antioxidant effects.
In a recently study published in 2017, a 1-year prospective, randomized, placebo-controlled, double-blind study evaluated the impact of Vitamin C on post-operative outcomes after lumbar fusion surgery. In this study Vitamin C treatment was initiated on the first postoperative day each following morning for 45 days. Remarkably, the dosage of Vitamin C was not revealed but was “chosen to be consistent with 2 previous studies of vitamin C,” which used either 500 mg or 1000 mg doses. The study concluded that Vitamin C was associated with improvement of functional status after lumbar fusion surgery, especially during the first 3 post-operative months, although it was not significantly different at 1 year after surgery. However, other studies have been published regarding the use of Vitamin C that are supportive of benefit.
Additional research has shown that supplementation with Vitamin C significantly reduces post-operative pain and decreases morphine consumption after laparoscopic cholecystectomy (gall bladder removal). In addition, the blood concentration of Vitamin C decreases after surgery, suggesting the requirement for Vitamin C increases in surgical patients. Other clinical and/or experimental reports have suggested that Vitamin C leads to functional improvements of damaged nerves. These observations can be explained by a greater demand for Vitamin C caused by increased oxidative stress. Therefore there is reasonable expection of benefit and lack of significant risk for side effects to recommend supplementation with Vitamin C, 500 mg – 1000 mg/day in the pre-operative as well as post-operative period for possibility that Vitamin C may reduce the intensity of postoperative pain and improve functional outcomes.
See: Oxidative Stress
Vitamin D
A 2019 study of the use of perioperative supplementation with Vitamin D in low back pain patients undergoing lumbar spinal fusion surgery suggested that it may decrease the intensity of acute postopeative pain. The authors theorized that supplementation with vitamin D may reduce systemic inflammation and recommended that LBP patients undergoing spine surgery should use vitamin D perioperatively as a supplement. The dose of Vitamin D employed in the study was 3200 IU/day but no correlation was reported regarding baseline serum levels of the patients Vitamin D.
The authors did indicate that their findings were consistent with another study demonstrating that patients with Vitamin D deficiency before spinal fusion experienced greater pain and had higher disability scores. Another study on Vitamin D blood level normalization showed decreased pain intensity and improved muscular strength in Vitamin D deficient women were achieved after 3 months of vitamin D and calcium supplementation.
Buprenorphine
Postoperative is often exacerbated by the development of secondary hyperalgesia (exaggerated sensation of pain) , especially around the surgical wound site. Secondary hyperalgesia arises from central sensitization and/ or acute peri-operative opioid exposure, especially with fentanyl analogues and is also known as opioid-induced hyperalgesia (OIH). Remifentanil, a potent opioid used in the operative setting, has been reported to induce postoperative hyperalgesia and increase postoperative pain scores and opioid use.
The mechanism underlying secondary hyperalgesia is thought to involve N-methyl-D-aspartate (NMDA)-mediated pain pathways. A 2017 study evaluated the perioperative infusion of low-dose buprenorphine (25 mcg/hr), an opioid with anti-NMDA activity, in patients receiving remifentanil infusion. The study concluded that low-dose buprenorphine infusion prevents the development of secondary hyperalgesia around the surgical incision up to three months after surgery.
Chronic Post-Operative Pain
The Transition of Acute, Post-Operative Pain to Chronic Pain
While the occurence of acute pain in the post-operative period is to be expected by most patients, the transition of acute post-operative pain to become a chronic, possibly life-long source of pain is generally not expected. Unfortunately, surgically-induced chronic pain is a significant clinical problem, with persistent pain estimated to occur in 10–50% of individuals after common operations. Specific surgeries have been associated with higher incidences of CPSP, such as mastectomy, thoracotomy and inguinal hernia repair. By definition, chronic pain is ‘pain lasting for more than 3 months’. Some patients develop their chronic post-surgical pain (CPSP) almost immediately after surgery, while in others it starts weeks or months after the surgery.
Chronic post-surgical pain is generally considered to be neuropathic, occuring as a consequence of direct nerve injury, a consequence of transection, contusion, stretching, or inflammation of a nerve or occuring as the result of peripheral and central sensitization of the nervous system as a consequence of surgery.
Incidence of Chronic Post-Surgical Pain (CPSP)
It has been estimated that CPSP occurs in 1 of every 10 surgical procedures and it becomes an unbearable condition in 1 of every 100 surgeries. Chronic post-surgical pain is reported to occur in 60% of patients after limb amputation, in 30%-55% after cardiac surgery, in 20–60% after thoracic surgery, in 20% after hernia repair and in 20–40% after mastectomy with chronic chest wall pain an increasingly recognized common and problematic complication (see Post-Mastectomy Pain). The prevalence of phantom limb pain following surgical amputation is high, occuring in 79% of cases. The incidence of post-cesarean chronic pain has been reported as 12.3%, while 19% of patients have chronic pain 6 months following knee replacement.
One reason for the variability in these statistics is the difference in the time reference considered by each researcher for labeling pain as CPSP (varying from 2 months to 1 year postoperatively. Also, the amount of injury to the tissues or nerves and the degree of inflammation differ by operation type and procedure for the same surgery. For example, there is a reduced incidence of moderate to severe CPSP with laparoscopic removal of gall bladder – cholecystectomy (8.8%) compared with open cholecystectomy (28%). Orthopedic surgery is associated with an almost three-fold increased risk of moderate to severe CPSP, compared with all other procedures, at 12 months
Given that tens of millions of surgeries are performed each year, CPSP is epidemic, and even by conservative estimates, the number of patients suffering from it is significant. Severity varies from no or minimal pain to significant pain (> 4/10 on a Visual Analogue Scale), with severe pain reported in 2–10% of patients.
Even when surgery is performed to reduce pain, chronic pain can persist or worsen despite the surgery. With surgery for low back pain, there is a 5%–36% recurrence rate of back or leg pain 2 years after discectomy for disc herniation. In addition, it has been reported that 29% of patients had the same or increased pain 1 year after surgical laminectomy for lumbar stenosis secondary to degenerative changes.
The Transition of Acute, Post-Operative Opioid Use to Chronic Opioid Use
A significant concern in the context of today’s “opioid crisis” is the potential for patients treated with opioids for acute post-operative pain to progress to chronic use of opioids. Is this really the same question explored above, the transition from acute post-operative pain to chronic post-operative pain? Most likely this is probably so for most. The concern of course lies in the potential for patients exposed to opioids as part of their post-operative pain management to develop an abusive or addictive relationship with their opioids.
Studies have been published that evaluate the incidence and risk factors for persistent opioid use after surgery. In 2017 a study evaluated nationwide insurance claims from 2013 to 2014 involving US adults aged 18 to 64 years without opioid use in the year prior to surgery (ie, no opioid prescription prescriptions filled from 12 months to 1 month prior to the procedure).
In this study group of 36,177 patients, the incidence of persistent opioid use for more than 90 days and up to 180 days after both minor and major surgical procedures was identified. Minor surgeries included: varicose vein removal, laparoscopic gall bladder removal, laparoscopic appendectomy, hemorrhoidectomy, thyroidectomy, transurethral prostate surgery, parathyroidectomy, and carpal tunnel surgery. Major surgical procedures included: ventral incisional hernia repair, colectomy, reflux surgery, bariatric surgery, and hysterectomy. The study identified 29,068 (80.3%) patients who had minor surgical procedures and 7109 (19.7%) who had major procedures.
The rates of new persistent opioid use were unexpectedly similar between both the minor and major surgical procedure groups, ranging from 5.9% to 6.5%, indicating that patients likely continue opioids for reasons other than solely the intensity of surgical pain. By comparison, as would be expected, the incidence in the non-operative control group was less: only 0.4%. Of note, these results are also comparable with the 5% incidence of new long-term opioids use after the first opioid exposure using data from the Oregon prescription drug monitoring program, which includes non-operative opioid prescriptions.
This study further assessed the data for predictors of persistent opioid use. Risk factors included pre-operative tobacco use, alcohol and substance abuse disorders, mood disorders including depression and bipolar disorder, anxiety and preoperative pain disorders (back pain, neck pain, arthritis and centralized pain/central sensitization.
A 2017 study of 1,294,247 patients published by the Center for Disease Control (CDC) evaluated the characteristics of initial opioid prescriptions and the likelihood of long-term opioid use in the United States from 2006–2015. This study found that 33,548 (2.6%) of patients continued opioid therapy for ≥1 year and were more likely to be older, female, have a pain diagnosis before opioid initiation, have been initiated on higher doses of opioids, and were publicly or self-insured. Among patients prescribed at least 1 day of opioids, the probability of continued opioid use at 1 year was 6.0% and at 3 years was 2.9%.
The probability of long-term opioid use increases most sharply in the first days of therapy, particularly after 5 days or 1 month of opioids have been prescribed, and levels off after approximately 12 weeks of therapy. While the rate of long-term use was relatively low (6.0% on opioids 1 year later) for patients with at least 1 day of opioid therapy, it increased to 13.5% for patients whose first episode of use was for ≥8 days and to 29.9% when the first episode of use was for ≥31 days.
It was also found that the largest increases in probability of continued opioid use were observed after the fifth and thirty-first days on therapy; the risk for persistent opioid use at one year doubled when a second prescription was provided; 700 morphine milligram equivalents (ME) or more as a cumulative dose; and when first prescriptions provided 10- and 30-day supplies.
The highest probabilities of continued opioid use at 1 and 3 years were observed among patients who initiated treatment with a long-acting opioid (27.3% at 1 year; 20.5% at 3 years), followed by those whose initial treatment was with tramadol (13.7% at 1 year; 6.8% at 3 years) or a Schedule II short-acting opioid other than hydrocodone or oxycodone (8.9% at 1 year; 5.3% at 3 years). The probabilities of continued opioid use at 1 and 3 years for patients starting on hydrocodone short-acting (5.1% at 1 year; 2.4% at 3 years), oxycodone short-acting (4.7% at 1 year; 2.3% at 3 years), or Schedule III–IV (5.0% at 1 year; 2.2% at 3 years) opioids were similar.
It is important to remember that these statistic represent associations and do not establish cause and effect. However, the CDC concluded that the transition from acute to long-term opioid use can begin quickly: the chances of chronic use begin to increase after the third day and rise rapidly thereafter. Based on these results, CDC guidelines recommend that treatment of acute pain with opioids should be for the shortest duration possible. Prescribing <7 days (ideally ≤3 days) of medication when initiating opioids may reduce the chances of unintentional chronic use. When initiating opioids, CDC recommends caution when prescribing >1 week of opioids or when providing a refill or a second opioid prescription because these actions approximately double the chances of opioid use 1 year later.
As addressed above and emphasized throughout this web site, pain perception is complex, with multiple variables that are contributive to the severity and persistence of pain and, most importantly, the degree to which people suffer and/or are compromised by their pain. It requires diligence on the part of both surgical patients and their clinicians to take steps to reduce the incidence of preventable chronification of post-operative pain and opioid use.
Opioid-Free Surgery
Clearly, one way to possibly reduce persistent opioid use post-operatively is to perform opioid-free surgery. The concept of opioid-free surgery has been introduced and trialed at select institutions, although its application has been slow and inconsistent. Some proposed indications for opioid-free surgery include those patients with higher risk for opioid-related complications such as obesity, obstructive sleep apnea (OSA), chronic obstructive pulmonary disease (COPD), complex regional pain syndrome (CRPS), and cancer. Although conceptually it appears logical that opioid-free surgery would reduce opioid-related complications and improve the peri-operative patient experience, few studies have been published. Furthermore, it appears that opioid-free surgery does not significantly reduce opioid prescribing patterns at discharge, even when pain scores and opioid use are low prior to discharge.
Other, Possibly Related Post-Operative Complications
There are other post-operative complications that may be mechanistically related to the evolution of CPSP including depression, fatigue and postoperative cognitive dysfunction. The underlying basis for overlapping mechanisms of causation in these conditions is the process of neuroinflammation which may, in turn, be related at least in part to changes in the microbiome (the microbial population of the intestines) and dysruption of the blood brain barrier. These topics are reviewed elsewhere on this web site.
See: Neuroinflammation
Postoperative Cognitive Dysfunction (PCD)
Postoperative cognitive dysfunction (PCD), or impaired thought processing, is often seen in the elderly after surgery and hospitalization. Not unlike circumstances surrounding traumatic brain injury (TBI), a state of neuroinflammation can be initiated by surgical trauma even outside of the brain and central nervous system. Inflammatory mediators released in the surgical site can enter the nervous system and damage synapses and neurons. This has been proposed as a critical component of surgery-induced PCD. As with TBI, cerebral mast cells have been suggested to contribute to postoperative cognitive dysfunction and pain after surgical procedure-mediated neuroinflammation by promoting breakdown of the integrity of the blood-brain barrier (BBB). In addition, astrocyte participate in surgery-induced cognitive dysfunction and neuroinflammation via evoking microglia activation.
It follows that treatments directed at neuroinflammation for the reduction of post-operative pain may also reduce the incidence and/or severity of postoperative cognitive dysfunction (see below).
See: Traumatic Brain Injury (TBI)
Risks for developing chronic post-surgical pain
There is marked patient variability in the response to identical surgical procedures, so that not all surgical procedures and nerve injury lead to chronic post-surgical pain. A number of factors related to the individual patient may increase the risk of developing chronic post-surgical pain include age, gender, genetics, preexisting pain, and behavior.
Duration and Severity of Acute Post-Operative Pain
As noted above, one of the most significant, consistent factors that contribute to the progression of acute to chronic post-surgical pain is the duration of severe acute postoperative pain. This is why it is so important to treat acute post-operative pain aggressively in hopes of avoiding the central sensitization. that leads to the chronification of pain.
Age, Gender and Obesity
Adult nervous systems are less adaptive and more likely to give rise to chronic pain while chronic post-surgical pain is relatively uncommon in children. However, surgeries at an early age may still have long-lasting consequences on subsequent sensitivity to pain. Gender studies suggest women are more likely to develop chronic post-operative pain while elder people tend to be less likely. Obesity also contributes to increased likelihood of postoperative pain.
Genetics
Data from research clearly suggest a genetic predisposition for those who develop chronic pain following a precipitating incident. Twins studies show a heritable component to the risk of developing persistent pain of up to 60%. Part of this risk is very likely to be epigenetic as well (see below). Polymorphisms of catechol-O-methyltransferase (COMT) have been shown to influence pain sensitivity.
Use of Opioids
The use of opioids during surgery may effect post-operative pain and post-operative pain management can result in adverse effects, such as sedation, nausea and vomiting, urinary retention, ileus (interference with bowel function), and respiratory depression. In an effort to reduce these complications, multimodal analgesia, i.e., the use of more than one analgesic modality to achieve effective pain control while reducing opioid-related side effects, has become the cornerstone of enhanced recovery.
Pre-Surgical Chronic Pain
The presence of preoperative pain, regardless of the relationship to surgical site, significantly increases the risk of developing chronic post-surgical pain. A pre-surgical chronic pain condition is believed to sensitize the brain and may exaggerate the process of developing chronic post-surgical pain. Multiple spinal and brain regions have been found to be modified by chronic pain including dorsal horn neurons in the spinal cord and regions not only involved in sensory and pain processing (S1, thalamus, and posterior insula) but also regions involved in emotional processing and subjective magnitude assessment of pain (cingulate cortex, insula, periaqueductal grey, ACC, prefrontal cortex).
In other words, the changes in the brain associated with pre-surgical chronic pain establishes a contextual setting in which the pain associated with new surgical pain may be magnified and chronified.
Behavioral Variables
The importance of a patient’s psychological state prior to surgery is a significant factor in predicting risk for post-surgical pain. Predictors include depression, anxiety and pain catastrophizing. Pain catastrophizing is associated with greater levels of acute postoperative and chronic pain. Adequate preoperative counseling regarding the surgery and expected outcomes can reduce stress and help prevent CPSP.
Reducing Post-Operative Pain, Acute and Chronic
A great deal of research is being perfomed in an effort to better understand more about how acute pain becomes chronic. That being said, due to the overlapping goals of reducing both acute post-surgical pain and the transitioning to CPSP, the approach to achieving these goals are the same. The following is a review of recent research in exploring ways to reduce the post-operative pain associated with surgical procedures, including orthopedic and abdominal surgeries as well as others.
Clearly the less invasive and the less extensive the surgery, the less likely the procedure will lead to CPSP. While the patient may have little to say in directing these variables, understanding the surgical options presented can sometimes provide opportunity for safer choices.
Additionally, the method of anesthesia is a variable for modifying post-operative pain. Studies suggest that regional analgesia techniques such as epidural anesthesia, wound infiltration and intercostal nerve blocks, as compared with general anesthesia may reduce the incidence of post-operative pain. Unfortunately, the research is not as consistent for the prevention of chronic post-operative pain as they are for the prevention of acute pain.
Multi-modal Approach
Because uncontrolled pre-operative and/or post-operative pain contributes to increased risk for post-op pain and CPSP, it is important to treat pain aggressively in the peri-operative period. Similarly, depression presents the same risks and should be treated aggressively as part of perioperative pain management. Reearch has taught us that the preferred means of reducing post-operative pain is to engage a multi-modal approach. A multi-modal approach can be defined as the use of more than one pharmacological class of analgesic medication targeting different receptors along the pain pathway with the goal of improving analgesia while reducing individual class-related side effects. It has been said that “a good multi-modal protocol is a checklist rather than a recipe,” one that allows for flexibility in the individual components based on the patient’s comorbidities, allergies, medications, and previous surgical experience.
Surgical pain can be nociceptive, neuropathic, mixed or psychogenic, depending on the patient and the surgery. As such, medications from different classes may be required for successful pain reduction. It has been shown that treating pain using different forms of treatment including multiple medictions with different mechanisms of action offers the most effective means of controlling pain while at the same time reducing the need for opioids and limiting the evolution of chronic pain.
In an effort to reduce both acute post-operative pain and the development of chronic post-operative pain, studies are ongoing to identify both pharmacologic and non-pharmacologic means of doing so. Pharmacologic agents that are being explored include gabapentin and pregabalin, tramadol, NSAIDs, clonidine, ketamine, orphenadrine and nefopam (a non-opioid analgesic not available in the U.S.). Non-pharmacologic methods include acupuncture, relaxation therapy, music therapy, hypnosis and transcutaneous nerve stimulation (TENS) as part of multi-modal approaches of reducing post-operative pain.
Recent research that looks at the transitioning of acute pain to chronic pain has identified neuroinflammation as a likely major contributor to the process. Neuroinflammation is an inflammatory condition within nerve tissue both peripherally and centrally, in the spinal cord and brain. Inflammatory cells, called glial cells are found within the tissue matrix adjacent to and surrounding nerves. These glial cells respond to nerve injury as may occur with trauma such as surgery and normally contribute to the healing process. Cells called mast cells play a role in the activation of glial cells. However, for reasons not entirely understood, the inflammatory response of glial cells may become poorly regulated leading to pathologic inflammation around the nerve which leads to chronification of pain that persists beyond the normal healing process.
A growing body of evidence suggests that regulation of mast cells and glial cells may facilitate the healing process and at the same time reduce chronic neuroinflammation thereby reducing the development of chronic pain. Unfortunately, at this point in time much of the research is preclinical and definitive answers to the prevention and treatment of chronic pain related to neuroinflammation is still in the early phases. The good news, however, is that some agents have been identified that research indicates are safe and effective in the management of glial cell regulation and very effective for neuroinflammatory pain.
See: Neuroinflammation
Diet and Post-Operative Pain
Diet plays multiple roles in post-operative pain. To start with the obvious, it provides nutritional support for the healing process and as such should include nutrients favorable to repairing damaged tissues. It also plays a role in inflammation including, importantly, the resolution of the acute inflammatory process that is a normal and vital part of the healing process.
Anti-Inflammatory Diet
A significant contributing factor in the evolution of chronic pain is the failure of the acute pain and inflammation associated with a tissue injury to resolve as part of the healing process. Instead, when the inflammatory process fails to resolve, the chronification of pain ensues. Recent research has identified some of the variables in this process of inflammation resolution and the role post-operative diet may have. Preliminary research suggests that omega-3 fatty acids may play a role in resolving inflammation. As such, a diet rich in omega-3 including fish may be helpful. The oxidative stress associated with the trauma of tissue destruction calls for a diet rich in antioxidants to aid in recovery and reduce inflammation. Fruits and vegetables are essential sources of antioxidants, especially vitamin C (see above). Supplementing with antioxidants such as curcumin and resveratrol may offer benefit in reducing post-operative oxidative stress and inflammation.
See
Anabolic Diet
An anabolic diet is one that supports healing processes involved in tissure repair and regeneration. Protein is an essential component in these healing process and is thus it is important to maintain a diet high in protein to facilitate recovery after surgery. Additionally, essential nutrients for healing are increased in demand by healing tissues including the B-vitamins and vitamin C. Minerals including calcium, magnesium and zinc are also important. Supplementing with a quality multi-vitamin, especially one with antioxidants such as PhytoMulti by Metagenics would be advised. Better yet, make an appointment with our registered dietitian for a focused session on dietary preparing for surgery.
Nutriceutical Supplements
A nutriceutical is a pharmaceutical nutrient used for medicinal purposes. There are a multitude of supplements on the market with a multitude of associated health claims so it is important to identify those with good evidence for safety and therapeutic benefit. With respect to their use in the setting of preventing post-operative pain, nutriceuticals with potential effectiveness in tissure healing or regeneration and reducing pain, tissue inflammation, neuroinflammation and central sensitization offer potential benefit. The following nutriceuticals have good evidence for safety and therapeutic benefit and offer potential usefulness in the setting of post-operative pain, although specific research evidence for effectiveness in preventing post-operative pain, acute or chronic, is lacking. Their proposed benefit is based largely on preclinical laboratory and animal research along with theoretical mechanistic activity.
Palmitoylethanolamide (PEA)
Perhaps the best agent currently recommended for neuroinflammatory pain is palmitoylethanolamide (PEA), a natural substance manufactured by glial cells and also found in foods such as milk and egg yolks. PEA has good evidence to support its benefit in regulating neuroinflammation through its stabilization of mast cells and glial cells. Another safe and potentially effective natural substance that may be effective in glial cell neuroinflammation is resveratrol.
See: Palmitoylethanolamide (PEA) & Resveratrol
Curcumin
Curcumin is a naturally occuring antioxidant and powerful anti-inflammatory with potency equivalent or superior to ibuprofen and other NSAIDs but it is not associated with the toxicity and safety concerns associated with NSAIDs. Futhermore, it is a NRF2 activator and as such is believed to stimulate cellular production of endogenous antioxidants. It offers definite potential benefit in the setting of post-operative pain.
See: Curcumin and NRF2 activators
N-Acetyl Cysteine (NAC)
(More info coming)
Prescription Medications
There are a number of prescription medications that offer potential benefit in reducing post-operative pain although their use in this setting would be considered “off-label.” Medications directed at reducing neuropathic pain, the basis of central sensitization and the development of CPSP, include the gabapentenoid drugs, gabapentin (Neurontin) & pregabalin (Lyrica), venlafaxine ER, an extended release antidepressant, NMDA antagonists such as ketamine, and glial cell inhibitors including minocycline and low-dose naltrexone.
Gabapentin (Neurontin) & Pregabalin (Lyrica) in Acute Post-Operative Pain
Gabapentin (Neurontin)
In multiple reviews of studies evaluating post-operative pain after total knee and total hip arthroplasties (replacements), surgical procedures in which parts of the joints are replaced with artificial parts (prostheses), it was shown that the need for opioids for post-operative pain was reduced when gabapentin was used. The pruritis (itching) associated with the post-operative opioids was also lessened. Gabapentin trials show a moderate to large reduction in the occurrence of CPSP.
A 2011 study evaluating post-operative pain after lumbars discectomies and laminectomies revealed similar results with reductions in post-operative pain, use of opioids and pruritis when gabapentin (1200 mg) and Lyrica (300 mg) were provided in the 24 hours preoperatively. Additional studies evaluating post-operative pain with abdominal and vaginal hysterectiomies, gall bladder surgery, tonsillectomies and breast surgery also described similar benefts of gabapentin.
It should be noted that gabapentin is not without side effects including cognitive impairment, dizziness, memory impairment, nausea and diarrhea. Recently it has also been demonstrated that gabapentin may also contribute to respiratory depression. It is has not clear how freauent or clinically significant this is but should be monitored and used in caution with those at high risk for central or obstructive sleep apnea.
Pregabalin (Lyrica)
Similarly, pregabalin (150 or 300 mg) has been studied pre-operatively and then continued postoperatively – in some studies, for only 2 more doses, but in others, for up to 2 weeks. Asystematic review and meta-analysis found that pregabalin significantly reduces the incidence of pain at 6 months and 12 months (4% vs 15%).
See: Gabapenetnoids
Dosing
The optimal dosages of the two drugs for postoperative pain are still controversial. The dose of gabapentin in studies range from a single pre-operative dose 300 mg to 1200 mg of gabapentin before surgery to continuing gabapentin for 8 to 10 days post-operatively, although an optimal dose was not identified. Despite the reduction in need for opioids for pain, the pain scores were not significantly different. In postoperative pain studies, gabapentin doses ranged from 300 mg to 1,200 mg, and those for pregabalin ranged from 50 mg to 300 mg. Regardless of their dosages, the adverse effects of both drugs were found to be similar. Pregabalin 300 mg day−1 and gabapentin 1,200 mg day−1 showed equivalent analgesic, opioid- sparing and adverse effects as well as patient satisfaction.
Gabapentin (Neurontin) & Pregabalin (Lyrica) in Chronic Post-Operative Pain
While fewer studies are available, a 2012 review of the literature concluded that perioperative treatment with gabapentin and pregabalin are effective in reducing the incidence of chronic postsurgical pain (CPSP), defined as pain lasting more than 2 months. More recent studies however have not identified conclusive benefit in preventing CPSP.
Antidepressants
Current understanding of how acute pain becomes chronic involves nerve pathways that descend from pain centers in the brain (locus coeruleus) to the spinal cord (dorsal horn) which suppress pain signal coming from the spinal cord to the brain thus reducing the perception of pain. These descending pathways involve two neurotransmitters, serotonin and noradrenaline, the neurotransmitters enhanced by antidepressants and certain other medications including clonidine and tapentadol (Nucynta).
The mechanisms by which the descending pathways, particularly noradrenaline and not serotonin, involve both suppressing nerve activity as well as reducing neuroinflammation by their action on glial cells in the spinal cord. Reduced noradrenaline activity in these areas is believed to contribute to the development of chronic pain.
Antidepressants therefore may play a role in reducing neuropathic pain and therefore potentially could reduce post-operative pain, especially CPSP. However, while studies of their use in the prevention of CPSP are inadequate to provide a definite recommendation for their benefit to be made, there is limited evidence for benefit with venlafaxine (Effexor).
One study evaluating venlafaxine for post-mastectomy pain found that venlafaxine extended-release (37.5 mg/d) significantly reduced chronic pain at 6 months compared to gabapentin (300 mg/day); both were started on the night before surgery and continued for 10 days postoperatively. A review study evaluated the use of antidepressants for the prevention of CPSP but examined only three trials, using venlafaxine, duloxetine (Cymbalta), and escitalopram (Lexapro) but a benafit was seen only with venlafaxine.
Alpha-2 Adrenergic Agonists
Noradrenaline, an important neurotransmitter in the pain centers of the brain and descending pain pathways from the brain to the spinal cord, has specific action mainly on alpha receptors. As noted above, reduced noradrenaline activity in these areas contribute to the development of chronic pain. The a-2 adrenergic agonists (drugs that stimulate receptors that adrenaline and noradrenaline stimulate) are a class of drugs used to treat multiple, distinctively different, conditions including high blood pressure, anxiety, opioid and other drug withdrawal and, importantly, pain. Common a-2 adrenergic receptor agonists include clonidine (Catapres) and lofexidine (Lucemyra) and also tizanidine (Zanaflex), a medication commonly used as a muscle relaxer.
Clonidine
Systemic clonidine used in the peri-operative period has been shown to decrease pain intensity and nausea post-operatively for up to 24 hours or longer as well as having a sparing effect for the use of opioids for acute post-operative pain. Unfortunately at this time there are no studies evaluating the benefit of clonidine for prevention of chronic post-surgical pain.
In other studies, oral clonidine doses between 0.1 to 0.3 mg have been used as a pre-medication to reduce post-surgical pain. Oral clonidine haas been shown to reduce anxiety and pain for up to 72 hours after surgery.
A 2017 study evaluated pre-operative use of clonidine in preventing or reducing post-surgical right shoulder tip pain, a common problem after laparoscopic cholecystectomy (removal of gall bladder). The finding of this study was that premedicating with 0.2 mg oral clonidine while not effective in preventing PLSP, it is however safe and effective for reducing PLSP intensity in the first postoperative hours.
Of unusual interest, the placebo group in this study received a “placebo” dose of 100 mg of Vitamin C with outcme of the study comparing this placebo group with the clonidine group. In fact, there is growing research that suggests that Vitamin C is in itself therapeutic in reducing post-operative pain (See above).
See Alpha-2 Adrenergic Agonists
NMDA Antagonists
An important mechanism in hyperalgesia involves the N-methyl-D-aspartate (NMDA) receptor, known for its major role in nerve plasticity (modification), and glutamate, the neurotransmitter that activates it. Spinal nerves experimentally exposed to remifentanil (a potent, short-acting synthetic opioid given to patients during surgery to relieve pain and as an adjunct to an anaesthesia.) show increased NMDA receptor activity. NMDA activity has been shown to contribute to central sensitivity and the development of chronic pain, suggesting a role for the use of NMDA antagonists for potentially reducing both immediate post-operative pain as well as for reducing the risk of the chronification of post-operative pain.
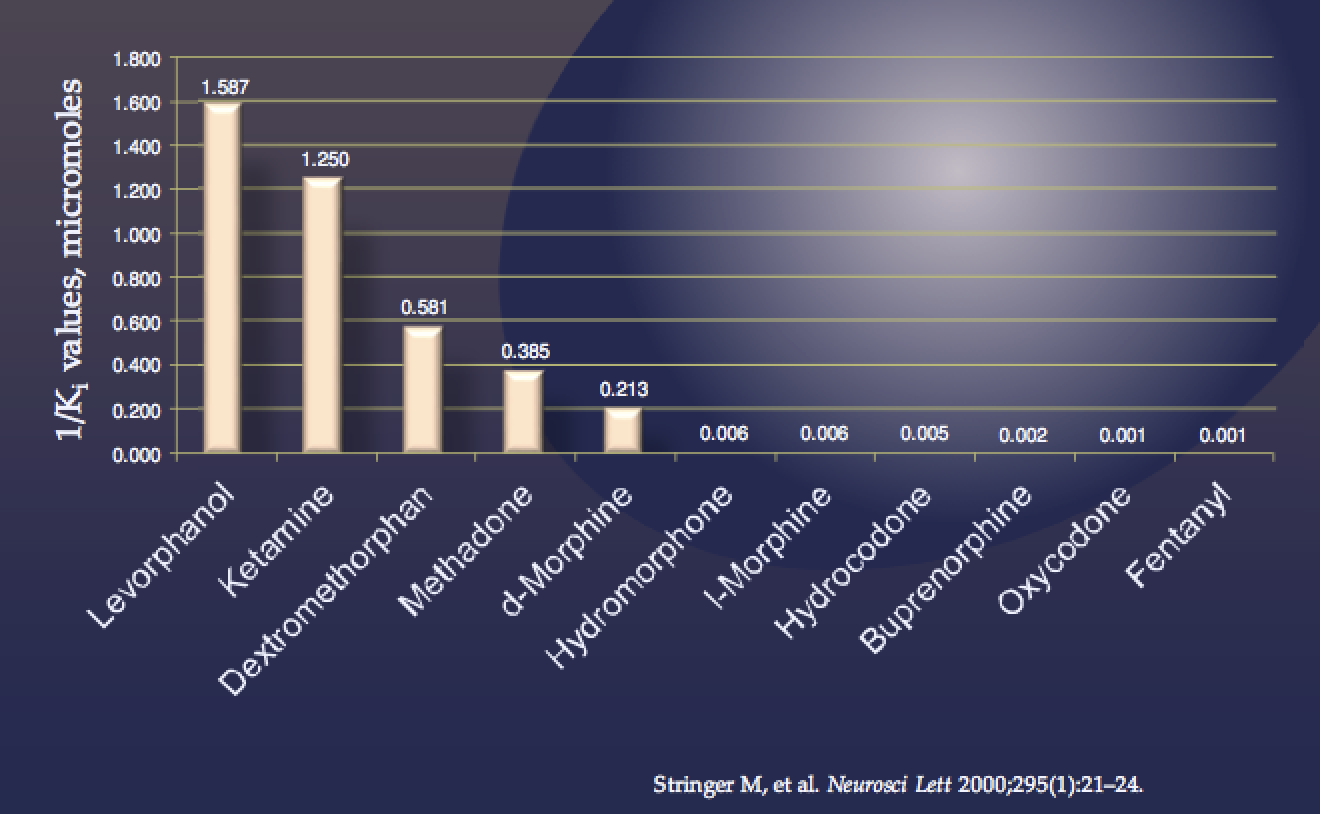
While the clinical data on the use of NMDA antagonists is growing, no definitive regimens have been defined for their use in the post-operative setting despite increasing evidence for their benefits. So far, the only studies apparently available for the use of NMDA antagonists in the peri-operative setting focus on ketamine. In principle, however, other medications with excellent safety profiles and NMDA antagonist activity are available, prescription and non-prescription. While the NMDA activity of some of these medications may be low, it is often the case in the field of medicine that the amount of a medication used to prevent a condition is less than that required to reverse a condition. While studies are lacking for efficacy, generally speaking the safety of these medications is well established.
NMDA antagonist activity of useful medications
Choice of Opioids for Perioperative Pain
Opioids remain the analgesics of choice for intraoperative and postoperative pain control for moderate to severe pain. Since severe postoperative pain is a CPSP risk factor, opioids may help in preventing CPSP. While strong opioids may be associated with opioid-induced hyperalgesia, likely transient, good pain control with opioids is important for CPSP prevention, despite their hyperalgesia risk. Interestingly, patients with negative beliefs about opioids have been shown to have a higher risk for CPSP.
Buprenorphine
Buprenorphine is considered the safest opioid for use in pain management, largely due to its ceiling effect on respiratory depression and its lower risk for abuse. While there is limited research evaluating the use of buprenorphine for post-operative pain, the use of Butrans patches have been demonstrated to be effective for mild to moderate pain.
Aside from safety benefits, however, buprenorphine may represent a superior choice for post-operative pain due to its proposed benefit for neuropathic pain and central sensitization. Furthermore, due to its low mu receptor occupancy at the low doses used with buprenorphine for pain (100 mcg-1800 mcg/day), as compared to the high doses used with opioid use disorder (up to 36 mg/day), it is feasible to use supplemental doses of traditional short acting opioids including morphine, hydrocodone and oxycodone as “breakthrough” pain agents.
For the patient with absence or a minimal baseline level of opioid tolerance, the starting dose for Butrans patches would the 5 or 10 mcg/hr. For patients with established levels of opioid tolerance up to 220 morphine equivalence, Belbuca can be started at doses up to 450 mcb BID.
Levorphanol
Levorphanol is an opioid with special characteristics including potent NMDA antagonism that makes it a particularly attractive choice for perioperative pain management. While appropriate for use on an as-needed basis, it offers a longer half-life compared with usual short-acting opioids including hydrocodone, oxycodone and hydromorphone. The use of levorphanol as a suggested approach to perioperative pain management would have strong merit. While methadone also offers some degree of NMDA antagonism, the multiple complexities of methadone management likely outweigh this benefit for most patients. Tramadol (Ultram) has weak NMDA antagonist activity and may offer some benefit.
See: Levorphanol
Tapentadol (Nucynta)
Tapentadol has proven benefit in the management of both acute and chronic pain and is effective in treating acute post-operative pain. It may, however, have additional advantage for reducing chronic postsurgical pain (CPSP) because of its action on the descending pain pathways, noradrenaline transmission and alpha-2 adrenoceptors activation which has been shown to reduce neuroinflammation.
A recent study found that a single preemptive oral dose of tapentadol (75 mg) is effective in reducing perioperative analgesic requirements and acute postoperative pain, without added side effects. Additionally, another study has demonstrated a synergistic effect with combining palmitoylethanolamide (PEA) with tapentadol in reducing chronic back pain.
Adjunctive NMDA Antagonists for Pain
(NMDA) antagonists, especially ketamine and magnesium, have been shown to reduce post-operative pain. Ketamine has a clear opioid-sparing effect in the perioperative period and may even reduce long-term opioid consumption in opioid-tolerant patients. Magnesium has produced mixed results as a postoperative analgesic when used alone but has demonstrated synergism when combined with morphine or ketamine (See below).
Ketamine
Animal studies show that NMDA antagonists that block NMDA can abolish hyperalgesia, supporting the rationale of using ketamine in the management of post-operative pain especially when remifentanil is used during anesthesia. A large study published in 2015 reviewing post-operative pain in adults confirmed the benefits of both ketamine and magnesium in reducing post-operative pain intensity and improved patient satisfaction. The benefits of the perioperative use of a subanesthetic dose of ketamine for the prevention of various types of CPSP, including phantom limb pain, has been supported by multiple studies. Significant reduction in pain for up to 6 months postoperatively has been seen with intravenous ketamine in patients undergoing colon resection.
Intra-operative use of intravenous ketamine has been shown to reduce opiate needs in the 48-hour post-operative period in opiate-dependent patients with chronic pain. Ketamine also likely reduces opioid consumption and pain intensity throughout the post-operative period in this same patient population. This benefit has been demonstrated without significant side effects.
Post-operative use of intravenous ketamine has been shown to be effective for reducing pain in a number of clinical studies published in the last few years. While the use of ketamine intravenously is limited to in-hospital treatment by physicians, prescription topical ketamine can be prescribed and may be useful in post-op pain.
A 2014 systematic review and meta-analysis evaluated the safety and effectiveness of ketamine in reducing the prevalence and severity of CPSP. Analysis of intravenous ketamine showed a statistically significant reduction in the risk at 3 (25%) and 6 months (30%), in particular if ketamine is administered for more than 24 hours perioperatively. Intravenous bolus doses for the prevention of CPSP were recommended in the range of 0.2-0.75 mg/kg, and infusions of 2-7 mcg/kg/min. Other routes of ketamine use did not show any significant difference from a placebo.
No significant difference beteen ketamine and placebo were identified in the incidence of side effects (hallucinations, nightmares, excessive sedation, nausea and vomiting) except for transient visual disturbances (nystagmus and double vision) .
See Ketamine
Dextromethophan (DXM)
Dextromethorphan (DXM) is a common ingredient in cough and cold remedies, including Delsym, Robitussin DM and many others. Structurally, DXM is structurally related to the opioid, levorphanol, although it is not itself considered an opioid. As an NMDA antagonist, dextromethorphan when used as an adjunctive to opioids for perioperative pain may useful in reducing pain, especially neuropathic pain, as well as preventing nerve damage and hyperalgesia. While research remains conflicting and still falls short of confirming definitive benefits and doses for supplementing with DXM, there are evidence-based arguments to consider the trial use of dextromethorphan in the management of peri-operative pain.
Orphenadrine (Norflex), a medication used for muscle spasm, also has weak NMDA activity and may offer benefit in reducing the development of hyperalgesia. When there are indications for the use of a muscle relaxer in the perioperative period, orphenadrine may offer an advantage.
Memantine (Namenda)
Memantine (Namenda), a medication used for Alzheimer dementia, has NMDA activity and there is growing evidence suggesting that memantine may be useful in reducing neuropathic (nerve) pain. Memantine has been studied in certain subgroups of pain patients including a trial showing the benefit of a combination of morphine and memantine in patients with complex regional pain syndrome (CRPS).
Magnesium Sulfate (MgSO4), given intravenously, has been shown in multiple recent studies to reduce post-operative pain and allow for reduced dosing of opioids. In a March 2017 study, investigators concluded that MgSO4 appeared to increase the analgesic potency of morphine. While the mechanism of this action has not been clearly defined, it is consistent with NMDA antagonist activity. A 2013 meta-analysis concluded that peri-operative intravenous magnesium reduced opioid needs and pain scores in the first 24 hours postoperatively, without any reported serious adverse effects.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
As noted above, peripheral sensitisation of nociceptors leading to primary hyperalgesia is an important contributor to post-operative pain. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) which reduce peripheral prostaglandin concentration and leads to reduced peripheral sensitisation are a useful component of multimodal analgesia. In randomized controlled trials and their meta-analyses, NSAIDs improve analgesia, reduce opioid requirements, and reduce adverse effects of opioids, including reducing postoperative nausea and vomiting associated with opioids in the early postoperative period.
Caution should be exercised with use of all NSAIDs in patients with kidney disease and those with increased risk of heart disease or stroke. One of the most important concerns with use of NSAIDs is the increased risk of postoperative bleeding with NSAIDs. However, a meta-analysis has revealed that ketorolac (Toradol) does not increase the risk of perioperative bleeding. Additionally, celecoxib (Celebrex), a COX-2 selective NSAID, provides similar effectiveness to nonselective NSAIDs, but is superior in the postoperative setting because of reduced adverse events.
Celecoxib lack platelet inhibition and therefore causes less postoperative blood loss than nonselective NSAIDs and are comparable to placebo. Additionally, Celecoxib shows a gastric ulceration rate similar to placebo and significantly lower than nonselective NSAIDs in high-risk patients, even for short-term use. Celecoxib does not cause bronchospasm in patients with NSAID-exacerbated respiratory disease. Concerns about cardiovascular complications of COX-2 selective NSAIDs has not been demonstrated with Celecoxib with either short-term or long-term use.
One note regarding celecoxib:
Concerns have been raised that there may be cross-reactivity between allergies to sulfa antibiotics and celecoxib, due to a structural sulfonamide element of the celecoxib shared with sulfa antibiotics. Because of this, it is often advised to avoid celecoxib if one has an allergy to sulfa antibiotics because a history of sulfa allergy may be associated with an increased risk of adverse reactions to a wide range of nonantibacterial sulfonamides, including celecoxib, loop and thiazide diuretics, certain antivirals, carbonic anhydrase inhibitors, and sulfonylureas. Concerns have also been raised that patients who have experienced an allergic reaction to one nonantibacterial sulfonamide may be at risk for an adverse reaction to others. However, there is good evidence that none of the nonantibiotic sulfonamides exhibit both of the features shown to be responsible for sulfonamide allergic reactions. The weight of evidence suggests that withholding nonantibacterial sulfonamides such as celecoxib from patients with prior reactions to antibacterial sulfonamides or other nonantibacterial sulfonamides is not clinically justified.
See: NSAIDs
Minocyline
Minocycline (Minocin) is an antibiotic sometimes used to treat rheumatoid arthritis (RA). It is part of the group of antibiotics known as tetracyclines. Although RA is not thought to be caused by an infection, minocycline may improve the signs and symptoms of this disease. Aside from its antibiotic property, minocycline has been show in inhibit the activation of glial cells and consequently reduce the process of neuroinflammation. For this reason minocycline has been proposed to offer benefit in the post-operative period to reduce the development of central sensitization and chronic pain. Studies investigating this proposed benefit is lacking however and it would likely be premature to suggest minocycline as a means of reducing the transition of acute to chronic post-operative pain at this time.
See: Minocycline
The Final Word on Reducing Post-Operative Pain
It is evident that there is much to learn about reducing post-operative pain and preventing the development of chronic pain. The medications described above remain in experimental phases but do offer potential benefit. It is also expected that future studies of epigenetic mechanisms may produce novel and effective analgesic drugs.
One underlying principle should be emphasized:
Pain is magnified by stress. There are many measures one can embrace to reduce stress both during the pre-operative and the post-operative time frame. These measures include nutritional and behavioral options. It is strongly advised to explore these areas on other pages of this web site:
See:
Mechanisms of Pain Associated with Surgery
Understanding the mechanisms of surgery-related pain is the first step in reducing it and potentially avoiding the transition from acute, post-operative pain to becoming chronic.
Central and Peripheral Nerve Sensitization: Related to Surgery
Following surgery, the intense influx of acute pain signals from peripheral nerves related to tissue trauma can trigger a magnification of pain through peripheral and central nerve sensitization, in which the excitability and responsiveness of nerves is increased. Contrary to common belief, central sensitisation can occur within a very short time span and can significantly contribute to the overall picture of a postoperative pain state. After damage to the nociceptive receptors during the surgery, a hyperalgesic state occurs. This is divided into primary hyperalgesia, resulting from the sensitisation of the peripheral nociceptors, and secondary hyperalgesia, which is associated with sensitisation of the spinal cord and the central nervous system.This is especially true in the dorsal horn of the spinal cord where peripheral nerves synapse (interact) with central nerves and pain transmission is enhanced.
Central and Peripheral Nerve Sensitization: Related to Chronic Pain
It has been well established that when people experience chronic pain, whether it be related to chronic headaches, injuries such as neck and low back pain, or medical conditions including fibromyalgia, menstrual pain or irritable bowel syndrome, they develop peripheral and, especially, central sensitization in the spinal cord and brain. This contributes to a magnified experience of pain (hyperalgesia), including acute pain unrelated to their chronic pain condition. The result of central sensitization contributes to other abnormal pain responses such as experiencing pain with non-painful stimuli (allodynia) and spread of hypersensitivity beyond the injured tissue. Patients with chronic pain frequently experience post-operative pain more severely and require higher doses of opioids to control that pain compared with patients without chronic pain.
Magnified Pain (Hyperalgesia): Related to Use of Opioids (OIH)
There is a growing body of research demonstrating that both acute and chronic use of opioids may contribute to a heightened or magnified experience of pain termed opioid-induced hyperalgesia (OIH). The incidence of OIH with acute, post-operative pain has been well demonstrated with the use of remifentanil, an opioid used during anesthesia for surgery. Post-operatively, patients receiving remifentanil experience magnified pain related to their surgery, subsequently requiring higher doses of opioids to control pain.
There is limited research that also suggests that long-term use of opioids for chronic pain can also lead to hyperalgesia. This has been demonstrated mostly related to experimental pain models evaluating pain from exposure to cold or heat. Whether these findings are clinically relevant remains to be established.
See Opioid-Induced Hyperalgesia (OIH)
Epigenetics
One of the worst outcomes of acute, post-operative pain is having that pain evolve into chronic pain. Understanding the mechanisms of how acute pain becomes chronic rather than healing and resolving is an important riddle that eludes full understanding.
Under persistent pain conditions cells processing pain signaling, i.e., nociceptors (pain receptors) in the peripheral nervous system and neurons/glia in the central nervous system, become sensitized in response to various stimuli. This increased sensitivity is accompanied by functional and structural changes (plasticity). Multiple mechanisms are likely responsible for these changes.
One area of study that is beginning to shed light on this process is the study of “epigenetics,” which refers to changes in a chromosome (DNA) that affect gene activity and expression. People inherit genes that determine personal characteristics including such as eye color and height or physiologic processes such as how medications are metabolized or how effective they are. The expression of these genes can be modified, for example by being amplified, suppressed or turned on or off. It is believed that epigenetic modification of genes may at least be in part responsible for transitioning acute pain, such as post-operative pain, to becoming chronic and persisting beyond apparent tissue healing. Understanding this process may lead to avoiding the evolution of chronic pain.
Medications can impact epigenetic change, including opioids. Both the developmental expression of the μ opioid receptor, and pathological hyperalgesia are mediated, at least in part, by epigenetic mechanisms. In general, opiates seem to increase global DNA methylation levels, a mechanism associated with hyperalgesia. This is in contrast to another group of drugs used in surgery – local anaesthetics. Local anaesthetics such as lidocaine appear to induce DNA demethylation, and may thereby protect against the development of hyperalgesia. Clinically, some studies have demonstrated a reduction of hyperalgesia and inflammation post-operatively vis epigenetic mechanisms with local anaesthetics.
Of major significance is that epigenetic modification can be inherited, passed on to the next and future generations. In other words, an environmentally-induced change in DNA expression can affect not just the person but their children and grandchildren. In animal studies of stress-induced intestinal pain hypersensitivity, epigenetic changes associated with experimental irritable bowel disease could still be detected in offspring two generations later. It is believed also that during pregnancy exposure to certain medications or drugs can precipitate epigenetic changes that are then passed on to the fetus.
References:
Preventing Pain Related to Surgery – Overviews
- perioperative-pain-management- 2007 pubmed-ncbi
- Pharmacotherapy for the prevention of chronic pain after surgery in adults (Review) – 2013
- optimizing-pain-management-to-facilitate-enhanced-recovery-after-surgery-pathways 2015 -pubmed-ncbi
- development-of-a-management-algorithm-for-post-operative-pain-mapp-after-total-knee-and-total-hip-replacement-2014
- Post-operative Opioid-Induced Hyperalgesia – ICM Case Summaries – 2016
- The Complexity Model – A Novel Approach to Improve Chronic Pain Care – 2014
- Postoperative_pain_from_mechanisms_to_treatment.
- Mechanisms of acute and chronic pain after surgery: update from findings in experimental animal models. – PubMed – NCBI – 2018
- Short-term pre- and post-operative stress prolongs incision-induced pain hypersensitivity without changing basal pain perception – 2015
- Age and preoperative pain are major confounders for sex differences in postoperative pain outcome – A prospective database analysis – 2017
- Optimizing pain management to facilitate Enhanced Recovery After Surgery pathways. – PubMed – NCBI – 2015
- Reward Circuitry Plasticity in Pain Perception and Modulation – 2017
- Surgically-Induced Neuropathic Pain (SNPP) – Understanding the Perioperative Process – 2013
- Preventing Chronic Pain following Acute Pain – Risk Factors, Preventive Strategies, and their Efficacy – 2011
- Regular physical activity prevents development of chronic pain and activation of central neurons – 2013
- Regional anaesthesia to prevent chronic pain after surgery – a Cochrane systematic review and meta-analysis – 2013
- Pharmacotherapy for the prevention of chronic pain after surgery in adults – 2017
- A systematic review of therapeutic interventions to reduce acute and chronic post-surgical pain after amputation, thoracotomy or mastectomy. – 2015
- Analysis of perioperative pain management in vascular surgery indicates that practice does not adhere with guidelines – a retrospective cross-sectional study – 2017
- Efficacy and safety of multimodal analgesic techniques for preventing chronic postsurgery pain under different surgical categories – a meta-analysis – 2017
- Postoperative pain—from mechanisms to treatment – 2017
- Local anaesthetics and regional anaesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children – 2018
- Chronic postsurgical pain – current evidence for prevention and management – 2018
- Preventive analgesia and novel strategies for the prevention of chronic post-surgical pain. – (2015)
- Poorly controlled postoperative pain – prevalence, consequences, and prevention – 2017
- Designing the ideal perioperative pain management plan starts with multimodal analgesia – 2018
- Special indications for Opioid Free Anaesthesia and Analgesia, patient and procedure related: Including obesity, sleep apnoea, chronic obstructive … – PubMed – NCBI – 2017
- Chronic pain patient and anaesthesia – 2019
- New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults – 2017
- Multimodal Analgesia, Current Concepts, and Acute Pain Considerations. – PubMed – NCBI -2017
- Recent Advances in Postoperative Pain Management – 2010
- Effect of perioperative systemic alpha2-agonists on postoperative morphine consumption and pain intensity – systematic review of randomized controlled trials- 2011
- Cannabinoids for Postoperative Pain – 2007
- A systematic review of therapeutic interventions to reduce acute and chronic post-surgical pain after amputation, thoracotomy or mastectomy – 2014
- Incidence of and Risk Factors for Chronic Opioid Use Among Opioid-Naive Patients in the Postoperative Period – 2016
- Educating-Patients-Regarding-Pain-Management-and-Safe-Opioid-Use-After-Surgery-2020
- Rate and Risk Factors Associated With Prolonged Opioid Use After Surgery – 2020
Preventing Pain Related to Surgery – Phantom Limb Pain
- Strategies for prevention of lower limb post-amputation pain: A clinical narrative review – 2018
- Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: a prospective, randomized, clinical trial. – PubMed – NCBI – 2011
- Chronic post-amputation pain – peri-operative management – Review 0- 2017
Preventing Pain Related to Surgery – Enhanced Recovery After Surgery (ERAS)
- Enhanced Recovery After Surgery: A Review. – PubMed – NCBI – 2017
- Pain management within an enhanced recovery program after thoracic surgery – 2018
- Optimizing pain management to facilitate Enhanced Recovery After Surgery pathways. – PubMed – NCBI – 2015
Preventing Pain Related to Surgery – Neuroinflammation, Glial Cells & Mast Cells
- Involvement of mast cells in a mouse model of postoperative pain. – PubMed – NCBI – 2011
- An Inflammation-Centric View of Neurological Disease – Beyond the Neuron – 2018
- Rescue of Noradrenergic System as a Novel Pharmacological Strategy in the Treatment of Chronic Pain – Focus on Microglia Activation – 2019
Preventing Pain Related to Surgery – Resolving Inflammation
- Vagus nerve controls resolution and pro-resolving mediators of inflammation – 2014
- The Resolution Code of Acute Inflammation – Novel Pro-Resolving Lipid Mediators in Resolution – 2015
- Resolvins in inflammation: emergence of the pro-resolving superfamily of mediators. – PubMed – NCBI – 2018
- Resolvins and protectins – mediating solutions to inflammation – 2009
- Resolvins and inflammatory pain – 2011
- Resolution of inflammation – an integrated view – 2013
- Protectins and maresins – New pro-resolving families of mediators in acute inflammation and resolution bioactive metabolome – 2014
- Proresolving lipid mediators and mechanisms in the resolution of acute inflammation – 2014
- Novel Pro-Resolving Lipid Mediators in Inflammation Are Leads for Resolution Physiology – 2014
- Novel Anti-Inflammatory — Pro-Resolving Mediators and Their Receptors – 2011
- Lipid Mediators in the Resolution of Inflammation – 2015
- PPARγ activation ameliorates postoperative cognitive decline probably through suppressing hippocampal neuroinflammation in aged mice. – PubMed – NCBI – 2017
- Postoperative cognitive dysfunction in the aged: the collision of neuroinflammaging with perioperative neuroinflammation. – PubMed – NCBI – 2018
- The Role of Neuroinflammation in Postoperative Cognitive Dysfunction – Moving From Hypothesis to Treatment – 2018
- Treating inflammation and infection in the 21st century: new hints from decoding resolution mediators and mechanisms – 2017
- Structural Elucidation and Physiologic Functions of Specialized Pro-Resolving Mediators and Their Receptors – 2017
- LPS is a Switch for Inflammation in the Gut and Beyond
- Identification of specialized pro-resolving mediator clusters from healthy adults after intravenous low-dose endotoxin and omega-3 supplementation – a methodological validation – 2018
- The Protectin Family of Specialized Pro-resolving Mediators – Potent Immunoresolvents Enabling Innovative Approaches to Target Obesity and Diabetes – 2018
- Protectins and Maresins – New Pro-Resolving Families of Mediators in Acute Inflammation and Resolution Bioactive Metabolome – 2014
- Functional Metabolomics Reveals Novel Active Products in the DHA Metabolome – 2012
Preventing Pain Related to Surgery – Alpha-2 Agonists
Preventing Pain Related to Surgery – Buprenorphine
- Role of buprenorphine in acute postoperative pain – 2016
- Efficacy and Safety of Transdermal Buprenorphine versus Oral Tramadol:Acetaminophen in Patients with Persistent Postoperative Pain after Spinal Surgery – 2017
- Low-dose buprenorphine infusion to prevent postoperative hyperalgesia in patients undergoing major lung surgery and remifentanil infusion a double-blind, randomized, active-controlled trial – 2017
Preventing Pain Related to Surgery – Diet
Preventing Pain Related to Surgery – Genetics
- genotyping-test-with-clinical-factors-better-management-of-acute-postoperative-pain-2015
- the-impact-of-genetic-variation-on-sensitivity-to-opioid-analgesics-in-patients-with-postoperative-pain-a-systematic-review-and-meta-analysis-2015
- Chronic postsurgical pain – is there a possible genetic link? – 2017
Preventing Pain Related to Surgery – Epigenetics
- Epigenetic-regulation-of-spinal-cord-gene-expression-controls-opioid-induced-hyperalgesia-2014
- Epigenetic-regulation-of-opioid-induced-hyperalgesia-dependence-and-tolerance-in-mice-2013
- Epigenetic-regulation-of-persistent-pain-2015
- Chronic-opioid-use-is-associated-with-increased-dna-methylation-correlating-with-increased-clinical-pain-pubmed-ncbi
- Could targeting epigenetic processes relieve chronic pain states? – PubMed – NCBI
- Epigenetic-mechanisms-of-chronic-pain-2015
- Telomeres and epigenetics – Potential relevance to chronic pain – 2012
- Epigenetics of chronic pain after thoracic surgery. – PubMed – NCBI
- Epigenetics-in-the-perioperative-period-2015
Preventing Pain Related to Surgery – Gabapentin & Pregabalin
- Do surgical patients benefit from perioperative gabapentin:pregabalin? A systematic review of efficacy and safety. – PubMed – NCBI
- Perioperative administration of gabapentin 1,200 mg day−1 and pregabalin 300 mg day−1 for pain following lumbar laminectomy and discectomy – 2011
- Preemptive use of gabapentin in abdominal hysterectomy: a systematic review and meta-analysis. – PubMed – NCBI
- The Effect of Gabapentin on Acute Postoperative Pain in Patients Undergoing Total Knee Arthroplasty – 2016
- The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. – PubMed – NCBI
- The use of gabapentin in the management of postoperative pain after total hip arthroplasty – 2016
- The use of gabapentin in the management of postoperative pain after total knee arthroplasty – 2016
- Use of gabapentin for perioperative pain control – A meta-analysis – 2007
- The efficacy of gabapentin:pregabalin in improving pain after tonsillectomy: A meta-analysis. – PubMed – NCBI
- Effects of gabapentin on postoperative pain, nausea and vomiting after abdominal hysterectomy: a double blind randomized clinical trial. – PubMed – NCBI
- Gabapentin and postoperative pain – a systematic review of randomized controlled trials 2006 – PubMed Health
- Preoperative Preemptive Drug Administration for Acute Postoperative Pain – A Systematic Review And Meta-Analysis – 2016
- the-effects-of-preoperative-oral-pregabalin-and-perioperative-intravenous-lidocaine-infusion-on-postoperative-morphine-requirement-in-patients-undergoing-laparatomy-2015
- perioperative-pain-management- 2007 pubmed-ncbi
- optimizing-pain-management-to-facilitate-enhanced-recovery-after-surgery-pathways 2015 -pubmed-ncbi
- Treatment_of_Neuropathic_Pain_The_Role_of_Unique_Opioid_Agents_-_2016
- The Anti-Allodynic Gabapentinoids – Myths, Paradoxes, and Acute Effects – 2016
- Gabapentinoids as a Part of Multi-modal Drug Regime for Pain Relief following Laproscopic Cholecystectomy: A Randomized Study – 2017
- Effects of pregabalin and gabapentin on postoperative pain and opioid consumption after laparoscopic cholecystectomy – 2017
- Do surgical patients benefit from perioperative gabapentin:pregabalin? A systematic review of efficacy and safety. – PubMed – NCBI
- Impact of pregabalin on acute and persistent postoperative pain: a systematic review and meta-analysis. – PubMed – NCBI
- Effects of pregabalin and gabapentin on postoperative pain and opioid consumption after laparoscopic cholecystectomy – 2017
- Effect of Perioperative Gabapentin on Postoperative Pain Resolution and Opioid Cessation in a Mixed Surgical Cohort – 2018
Preventing Pain Related to Surgery – Ketamine & NMDA Antagonists
- Role of Ketamine in Acute Postoperative Pain Management – A Narrative Review – 2015
- Perioperative ketamine for acute postoperative pain. – PubMed – NCBI
- Ketamine decreases postoperative pain scores in patients taking opioids for chronic pain: results of a prospective, randomized, double-blind study. – PubMed – NCBI
- Intraoperative ketamine reduces perioperative opiate consumption in opiate-dependent patients with chronic back pain undergoing back surgery. – PubMed – NCBI
- Ketamine as an Adjunct to Postoperative Pain Management in Opioid Tolerant Patients After Spinal Fusions – A Prospective Randomized Trial – 2007
- The efficacy of N-methyl-D-aspartate receptor antagonists on improving the postoperative pain intensity and satisfaction after remifentanil-based a… – PubMed – NCBI
- The clinical role of NMDA receptor antagonists for the treatment of postoperative pain. – PubMed – NCBI
- Ketamine – an old drug revitalized in pain medicine – 2017
- Effect of ketamine combined with magnesium sulfate in neuropathic pain patients (KETAPAIN) – study protocol for a randomized controlled trial – 2017
- A systematic review and meta-analysis of ketamine for the prevention of persistent post-surgical pain. – PubMed – NCBI – 2014
- Ketamine for pain – 2017
- Ketamine for pain management – 2018
- Butorphanol and Ketamine Combined in Infusion Solutions for Patient-Controlled Analgesia Administration – A Long-Term Stability Study – 2015
- Multimodal Analgesia, Current Concepts, and Acute Pain Considerations. – PubMed – NCBI -2017
Preventing Pain Related to Surgery – Magnesium
- Perioperative systemic magnesium to minimize postoperative pain: a meta-analysis of randomized controlled trials. – PubMed – NCBI
- Peri-operative intravenous administration of magnesium sulphate and postoperative pain – a meta-analysis – 2013
- Effect of magnesium sulfate on morphine activity retention to control pain after herniorrhaphy. – PubMed – NCBI
- Effect of ketamine combined with magnesium sulfate in neuropathic pain patients (KETAPAIN) – study protocol for a randomized controlled trial – 2017
Preventing Pain Related to Surgery – NSAIDs
See: NSAIDs
- Sulfonamide cross-reactivity: is there evidence to support broad cross-allergenicity? – PubMed – NCBI – 2013
- Should celecoxib be contraindicated in patients who are allergic to sulfonamides? Revisiting the meaning of ‘sulfa’ allergy. – PubMed – NCBI 2001
Preventing Pain Related to Surgery – Nefopam
- nefopam-after-total-hip-arthroplasty-role-in-multimodal-analgesia-pubmed-ncbi
- nefopam-analgesia-and-its-role-in-multimodal-analgesia-a-review-of-preclinical-and-clinical-studies-pubmed-ncbi
- preventive-analgesic-efficacy-of-nefopam-in-acute-and-chronic-pain-after-breast-cancer-surgery-2016
- neuronal-sensitization-and-its-behavioral-correlates-in-a-rat-model-of-neuropathy-are-prevented-by-a-cyclic-analog-of-orphenadrine-pubmed-ncbi
Preventing Pain Related to Surgery – Tapentadol (Nucynta)
Preventing Pain Related to Surgery – Vitamin C
Chronic Regional Pain Syndrome (CRPS)/Reflex Sympathetic Dystrophy (RSD)
- Efficacy of vitamin C in preventing complex regional pain syndrome after wrist fracture – A systematic review and meta-analysis – 2017
- [Vitamin C and prevention of reflex sympathetic dystrophy following surgical management of distal radius fractures]. – PubMed – NCBI
- Complex regional pain syndrome – recent updates – 2013
- Give vitamin C to avert lingering pain after fracture – 2008
- Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures – a randomised trial – 1999
- Effect of vitamin C on prevention of complex regional pain syndrome type I in foot and ankle surgery. – PubMed – NCBI – 2009
Preventing Pain Related to Surgery – Vitamin C
Lumbar Surgery
Preventing Pain Related to Surgery – Vitamin D
Opioids – Transitioning from Short Term to Long Term Use
- How acute pain leads to chronic opioid use – 2018
- Characteristics of initial prescription episodes and likelihood of long-term opioid use – United States, 2006-2015
- New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults – 2017
Opioids – Effects on the Immune System
- A Review of the Effects of Pain and Analgesia on Immune System Function and Inflammation: Relevance for Preclinical Studies – 2019
- The Role of Opioid Receptors in Immune System Function – 2019
- How I treat pain in hematologic malignancies safely with opioid therapy – 2020
- Do All Opioid Drugs Share the Same Immunomodulatory Properties? A Review From Animal and Human Studies – 2019
- Effects of systemic and neuraxial morphine on the immune system – 2019
- Long-acting Opioid Use and the Risk of Serious Infections: A Retrospective Cohort Study – 2018
- Immune function after major surgical interventions: the effect of postoperative pain treatment – 2018
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Please note also, that many of the benefits for medications described on this web site include “off-label” use for a medication. Off-label prescribing refers to the use of medication for a condition not named in its FDA approval. Physicians are free to prescribe any medication they want, as long as there is some evidence for usefulness. And remember that the lack of an FDA indication does not necessarily mean lack of efficacy—it sometimes means that no drug company has deemed the investment in clinical trials worth the eventual pay off.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices