Acute Pain, Journavx (suzetrigine):
Synergism Possibilities
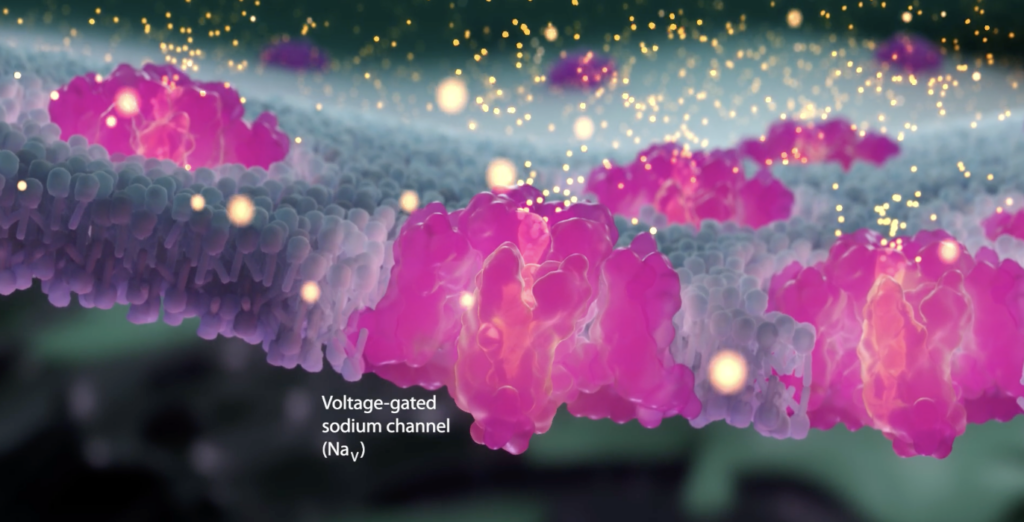
Vertex artist’s rendition of a sodium channel
Journavx is the first of a new class of pain medications {Selective Nav1.8 inhibitors).
This section explores the potential synergistic benefits of combining Journavx with other medications.
See:
- Journavx (suzetrigine)
See also:
- Acute Pain – Avoiding Transition to Chronic Pain
- The Transition of Acute Post-Injury Opioid Use to Chronic Opioid Use
- Omega 3 Fatty Acids
- Central Sensitization
- Neurobiology of Pain
- Gabapentin & Lyrica
- Palmitoylethanolamide (PEA)
- Dextromethorphan
- Ketamine
- Levorphanol
see also:
Definitions and Terms Related to Pain
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
What is Journavx (suzetrigine)?
Journavx (suzetrigine) is a first-in-its-class, new medication that relieves moderate to severe pain by a mechanism that is different from how other analgesic pain medications work, including acetaminophen (Tylenol), NSAIDs (ibuprofen, Aleve, Mobic etc.) and opioids. It works by inhibiting pain signals generated by pain receptors, for example when triggered by acute tissue damage, from being transmitted to the central nervous system and brain so as to reduce the perception of pain.
Since Journavx works via a unique mechanism, it can be taken along with other pain medications for added analgesic benefit. Because Journavx works on nerves in the peripheral nervous system and never enters the central nervous system or brain, it has no potential for addiction or contribution to accidental overdose if combined with opioids. Whether off-label use for chronic pain is effective has not been fully studied and it has not been approved for chronic pain at this time.
Although Journavx is currently FDA approved only for acute pain, is important to point out that it may actually have multiple benefits with respect to pain that as of yet have not been fully explored:
- Possible reduction of acute pain and acute exacerbation of chronic pain
- Possible suppression of transitioning of acute pain to becoming chronic
- Possible suppression of Peripheral and Central Sensitization
- Possible synergies with other medications with similar mechanisms of action
Synergistic Benefits of Journavx with Other Medications
Introduction
Based on the mechanism of action as to how Journavx (suzetrigine) relieves pain there is a potential for combining it with other medications with similar mechanisms that could potentially provide synergistic benefits. This section explores the possibility of combining Journavx with other sodium channel blockers, such as topical lidocaine or oral topiramate and calcium channel blockers. This analysis evaluates the mechanisms of action, evidence for synergy, quality of evidence, and clinical implications.
Synergistic Benefits of Journavx with Sodium Channel Blockers
Mechanisms of Action
Journavx (Suzetrigine)
- Mechanism: Suzetrigine is a selective voltage-gated sodium channel (NaV1.8) inhibitor, targeting peripheral pain-sensing neurons (nociceptors). NaV1.8 channels are critical for action potential propagation in pain signaling. By blocking NaV1.8, suzetrigine inhibits pain signal transmission to the spinal cord and brain, avoiding central nervous system (CNS) effects and reducing addiction potential [1, 2]. It is FDA-approved (January 30, 2025) for moderate-to-severe acute pain in adults [3, 4].
- Pharmacokinetics: Administered orally (100 mg loading dose, then 50 mg every 12 hours), suzetrigine is a CYP3A substrate and inducer, with contraindications for strong CYP3A inhibitors and interactions with certain hormonal contraceptives [5].
Topical Lidocaine
- Mechanism: Lidocaine is a non-selective sodium channel blocker, inhibiting multiple NaV subtypes (NaV1.7, NaV1.8, NaV1.9) in peripheral nerves. It stabilizes neuronal membranes, reducing ectopic discharges and hyperexcitability, particularly in neuropathic pain [6]. Topical formulations (e.g., ZT Lido, lidocaine 5% patches and topical lidocaine creams or gels) act locally in the skin (epidermis)[7]. Lidocaine also suppresses inflammatory mediators (e.g., cytokines) and modulates excitatory neurotransmission, enhancing its analgesic benefits [8].
- Relevance: Its local action complements suzetrigine’s systemic NaV1.8 blockade, potentially broadening peripheral pain inhibition.
Oral Topiramate
- Mechanism: Topiramate is an anticonvulsant with multiple mechanisms: weak blockade of voltage-gated sodium channels (NaV1.7, NaV1.8), enhancement of GABA neurotransmission, inhibition of glutamate receptors (AMPA/kainate), and carbonic anhydrase inhibition [9]. It reduces neuronal hyperexcitability in the peripheral nervous system (PNS) and CNS, making it potentially effective for neuropathic pain and migraine [10]. Its sodium channel blockade is less potent than lidocaine or suzetrigine but it can contribute to analgesia [11].
- Relevance: Topiramate’s CNS and PNS effects may complement suzetrigine’s peripheral specificity, addressing central sensitization in complex pain cases.
Minor Cannabinoids
- A recent 2025 pre-clinical study reports three minor, nonpsychotomimetic cannabinoids-cannabidiol (CBD), cannabigerol (CBG), and cannabinol (CBN)-effectively inhibit Nav1.8, suggesting their potential as analgesic compounds. In particular, CBG shows significant promise due to its ability to effectively inhibit excitability of peripheral sensory neurons. These findings highlight the therapeutic potential of cannabinoids, particularly CBG, as agents that may attenuate pain via block of Nav1.8, warranting further in vivo studies. Another 2025 study proposes that Nav channels are likely an important part of the pharmacology of CBD.
Potential Synergistic Mechanisms
- Complementary Sodium Channel Blockade: Suzetrigine’s selective NaV1.8 inhibition targets a specific pain pathway, while lidocaine’s non-selective blockade affects multiple NaV subtypes, potentially enhancing peripheral inhibition [6, 12]. Topiramate’s weaker NaV blockade may add CNS-level modulation [9].
- Anti-Inflammatory and Neuroplastic Effects: Lidocaine’s suppression of inflammatory mediators and ectopic discharges may enhance suzetrigine’s pain signal inhibition by reducing peripheral sensitization [8]. Topiramate’s modulation of GABA and glutamate pathways may mitigate central neuroplasticity, relevant for persistent opioid tolerance [11].
- Multimodal Pain Modulation: Combining peripheral (suzetrigine, lidocaine) and CNS (topiramate) mechanisms may target nociceptive and neuropathic pain components, particularly in patients with opioid-induced hyperalgesia (OIH) [13].
Evidence for Synergistic Benefits
General Evidence on Sodium Channel Blocker Combinations
- Preclinical Data: Studies suggest that combining sodium channel blockers with different NaV subtype specificities or additional mechanisms (e.g., GABA modulation) enhances analgesia. A 2019 review noted that lidocaine’s non-selective NaV blockade synergizes with opioids via inward rectifier potassium (Kir) channels, suggesting potential for synergy with other NaV blockers like suzetrigine [8]. No direct studies combine suzetrigine with lidocaine or topiramate, but complementary NaV targeting supports theoretical synergy [12].
- Clinical Data: Evidence for combining sodium channel blockers is limited, especially for suzetrigine due to its recent approval. Studies on other NaV blockers (e.g., lidocaine, carbamazepine) show enhanced efficacy when combined with agents targeting different pain pathways [14]. For example, topical lidocaine combined with gabapentinoids improves neuropathic pain control, suggesting potential for multi-mechanism approaches [15].
Specific Combinations
- Journavx + Topical Lidocaine:
- Evidence: No clinical trials directly evaluate suzetrigine with topical lidocaine. A 2018 study on topical phenytoin (a non-selective NaV blocker) for neuropathic pain noted that its intra-epidermal action, similar to lidocaine’s, enhances analgesia without systemic effects [16]. This suggests that lidocaine’s local NaV blockade could complement suzetrigine’s systemic NaV1.8 inhibition, reducing pain signals at multiple peripheral sites. A 2019 review of systemic lidocaine highlighted synergy with opioids via modulation of inflammatory pathways and ectopic discharges, which may extend to topical lidocaine with suzetrigine [8].
- Quality of Evidence: Low to moderate. Synergy is inferred from mechanistic overlap and studies on other NaV blockers. Suzetrigine’s NaV1.8 specificity may limit synergy if NaV1.7 or NaV1.9 are dominant in specific pain conditions.
- Relevance: For patients with persistent opioid tolerance, this combination may address peripheral sensitization without exacerbating OIH, suitable for localized postoperative or neuropathic pain.
- Journavx + Oral Topiramate:
-
- Evidence: No direct studies assess suzetrigine with topiramate. Topiramate’s efficacy in neuropathic pain and migraine is well-documented, with sodium channel blockade as a contributing mechanism [9, 10]. A 2007 study noted that topiramate’s multi-mechanism action reduces neuronal hyperexcitability, potentially complementing suzetrigine’s peripheral effects [11]. A 2015 review suggested that combining NaV blockers with CNS-acting agents (e.g., gabapentinoids) enhances analgesia in neuropathic pain, supporting a role for topiramate [15].
- Quality of Evidence: Low. Synergy is theoretical, based on complementary mechanisms. Topiramate’s weaker NaV blockade and CNS focus may limit direct synergy, but its role in central sensitization is relevant for chronic pain or OIH.
- Relevance: Topiramate could address central neuroplasticity in patients with persistent tolerance, complementing suzetrigine’s peripheral effects, especially in mixed pain states or during opioid tapering.
Quality of Evidence
- Preclinical: Moderate. Animal studies on NaV blockers demonstrate synergistic potential, but specific data on suzetrigine combinations are lacking [8, 16]. Mechanistic studies support complementary NaV subtype targeting [12].
- Clinical: Low. No trials evaluate suzetrigine with lidocaine or topiramate. Indirect evidence from lidocaine, topiramate, and other NaV blockers suggests synergy, particularly for neuropathic pain [6, 9, 15]. Suzetrigine’s Phase 3 trials focused on acute pain, with limited data on chronic pain or combinations [3, 4].
- Limitations: Suzetrigine’s recent approval (2025) limits combination studies. Chronic pain with central sensitization may benefit more from topiramate’s CNS effects than suzetrigine’s peripheral action [18]. Drug interactions (e.g., suzetrigine’s CYP3A induction) require monitoring [5].
Clinical Implications
- Synergistic Potential: Combining suzetrigine with topical lidocaine may enhance peripheral pain control in acute or localized neuropathic pain. Topiramate could address central sensitization in patients with persistent tolerance or OIH, complementing suzetrigine’s peripheral action. This multimodal approach aligns with managing complex pain in patients transitioning off high-dose opioids (e.g., morphine, hydrocodone, oxycodone).
- Practical Considerations:
- Dosing: Suzetrigine (100 mg loading, 50 mg q12h), lidocaine 5% patch (up to 3 patches daily), topiramate (titrated to 100–400 mg/day) [5, 6, 9].
- Drug Interactions: Avoid strong CYP3A inhibitors with suzetrigine; monitor topiramate levels due to CYP3A induction [5].
- Patient Selection: Suitable for patients with acute pain or mixed pain states, especially those with OIH or persistent tolerance [13].
- Monitoring: Assess for side effects (suzetrigine: pruritus, rash; lidocaine: local irritation; topiramate: cognitive impairment, paresthesia) and efficacy in acute vs. chronic pain [3, 6, 9].
Conclusion
Evidence for synergistic benefits of combining Journavx (suzetrigine) with topical lidocaine or oral topiramate is limited but supported by complementary mechanisms. Suzetrigine’s selective NaV1.8 blockade, lidocaine’s non-selective NaV inhibition, and topiramate’s multi-mechanism action could enhance peripheral and central pain modulation, particularly in patients with persistent opioid tolerance or OIH. Preclinical data suggest synergy among NaV blockers, but clinical trials are needed [8, 16]. This combination may be a viable non-opioid strategy for acute or mixed pain states, reducing reliance on opioids like hydrocodone or oxycodone.
Synergistic Benefits of Journavx with Calcium Channel Blockers
Calcium Channel Blockers
- Gabapentin (Topical and Oral):
- Mechanism: Gabapentin binds to the α2δ-1 subunit of voltage-gated calcium channels (VGCCs), primarily N-type (CaV2.2), reducing calcium influx and excitatory neurotransmitter release (e.g., glutamate) in the dorsal root ganglion (DRG) and spinal cord [5, 6]. This decreases neuronal hyperexcitability in neuropathic pain and central sensitization [7]. Topical gabapentin (e.g., 6–10% cream) acts locally on peripheral nerves, reducing ectopic firing with minimal systemic absorption [8]. Oral gabapentin (300–3600 mg/day) has broader CNS effects but lower bioavailability at higher doses (27–60%) [9].
- Relevance: Gabapentin’s inhibition of VGCCs may complement suzetrigine’s NaV1.8 blockade by reducing neurotransmitter release, potentially enhancing analgesia in peripheral and central pain pathways.
- Pregabalin (Lyrica, Oral):
-
- Mechanism: Pregabalin, a gabapentinoid, also binds α2δ-1 subunits of VGCCs (N-type, CaV2.2), with higher potency and linear pharmacokinetics compared to gabapentin (bioavailability ~90%) [10, 11]. It reduces calcium-mediated neurotransmitter release, suppressing neuronal excitability in neuropathic pain, fibromyalgia, and postherpetic neuralgia [12]. Dosing ranges from 150–600 mg/day, with faster onset (1 hour) than gabapentin [13].
- Relevance: Pregabalin’s CNS action may address central sensitization, complementing suzetrigine’s peripheral effects, especially in chronic pain or OIH.
Topical Alternatives
- Capsaicin:
- Mechanism: Capsaicin (0.025–8% patch) activates TRPV1 channels on nociceptive fibers, causing initial depolarization followed by desensitization, reducing pain signaling. It is effective for neuropathic pain (e.g., postherpetic neuralgia) [18].
- Relevance: Capsaicin’s peripheral desensitization may complement suzetrigine’s NaV1.8 blockade by targeting different nociceptive pathways.
- Topical NSAIDs (e.g., Diclofenac):
-
- Mechanism: Topical diclofenac (1–3% gel) inhibits cyclooxygenase (COX), reducing prostaglandin-mediated pain and inflammation in peripheral tissues [19]. It has minimal systemic absorption, making it suitable for localized pain.
- Relevance: Its anti-inflammatory action may enhance suzetrigine’s pain signal inhibition by reducing peripheral sensitization.
- Menthol/Camphor:
-
- Mechanism: Menthol (e.g., 1–10% cream) activates TRPM8 channels, producing a cooling sensation and counterirritant effect, while camphor modulates TRPV1 and TRPA1 channels, reducing pain perception [20].
- Relevance: These agents provide sensory modulation, potentially complementing suzetrigine’s NaV1.8 inhibition for localized pain relief.
Potential Synergistic Mechanisms
- Complementary Ion Channel Modulation: Suzetrigine’s NaV1.8 blockade reduces action potential propagation, while gabapentinoids (gabapentin, pregabalin) and ziconotide inhibit VGCC-mediated neurotransmitter release, potentially enhancing analgesia by targeting both sodium and calcium-dependent pain pathways [5, 14].
- Peripheral and Central Effects: Topical gabapentin and capsaicin act peripherally, complementing suzetrigine’s systemic NaV1.8 inhibition, while oral gabapentin, pregabalin, and ziconotide address central sensitization, relevant for OIH and chronic pain [7, 12].
- Anti-Inflammatory and Neuroplastic Modulation: Topical NSAIDs reduce peripheral inflammation, enhancing suzetrigine’s pain signal suppression [19]. Gabapentinoids mitigate central neuroplasticity, potentially reversing opioid tolerance effects [21].
- Multimodal Pain Control: Combining suzetrigine with VGCC blockers and topical agents targets nociceptive, neuropathic, and inflammatory pain components, aligning with your goal of managing complex pain in patients with high-dose opioid history [22].
Evidence for Synergistic Benefits
General Evidence on Calcium Channel Blocker Combinations
- Preclinical Data: Studies show synergy between VGCC blockers and other analgesics. For example, gabapentin enhances morphine analgesia in rat models of neuropathic pain by reducing CaV2.2-mediated neurotransmitter release [23]. Ziconotide demonstrates synergy with morphine in bone cancer pain models, suggesting potential for NaV and CaV blocker combinations [24]. No direct studies combine suzetrigine with gabapentinoids or ziconotide, but mechanistic overlap supports theoretical synergy [25].
- Clinical Data: Limited evidence exists for suzetrigine combinations due to its recent approval (2025). However, gabapentinoids combined with opioids or other analgesics (e.g., duloxetine) show enhanced efficacy in neuropathic pain, suggesting potential for suzetrigine synergy [26]. Topical agents like capsaicin and NSAIDs show additive effects with systemic analgesics, supporting multimodal approaches [18, 19].
Specific Combinations
- Journavx + Gabapentin (Topical and Oral):
- Evidence: No trials directly evaluate suzetrigine with gabapentin. A 2019 study showed topical gabapentin (6–10%) reduces neuropathic pain (e.g., postherpetic neuralgia) by inhibiting peripheral VGCCs, suggesting potential synergy with suzetrigine’s NaV1.8 blockade [8]. Oral gabapentin (300–3600 mg/day) enhances analgesia when combined with opioids (e.g., morphine, hydrocodone) in neuropathic pain, attributed to reduced glutamate release [27]. A 2016 review noted gabapentin’s efficacy in opioid induced hyperalgesia (OIH), which may complement suzetrigine in patients with persistent tolerance [21].
- Quality of Evidence: Moderate for oral gabapentin (based on neuropathic pain studies); low for topical gabapentin (limited trials). Synergy with suzetrigine is theoretical, based on complementary ion channel modulation [5, 8].
- Relevance: Topical gabapentin could enhance suzetrigine’s peripheral effects for localized pain, while oral gabapentin may address central sensitization in chronic pain or OIH.
- Journavx + Pregabalin (Lyrica):
-
- Evidence: No direct studies combine suzetrigine with pregabalin. Pregabalin (150–600 mg/day) is effective for neuropathic pain and fibromyalgia, with higher potency than gabapentin due to greater α2δ-1 affinity [10, 11]. A 2020 review noted pregabalin’s role in reducing spinal neuronal hyperexcitability in OIH, suggesting potential synergy with suzetrigine’s peripheral action [12]. Pregabalin’s synergy with opioids (e.g., oxycodone) in neuropathic pain supports a multimodal approach [26].
- Quality of Evidence: Moderate. Pregabalin’s efficacy is well-documented, but synergy with suzetrigine is inferred from mechanistic overlap and opioid combination studies [10, 12].
- Relevance: Pregabalin’s CNS effects may complement suzetrigine in patients with persistent tolerance, particularly for neuropathic or mixed pain states.
- Journavx + Topical Alternatives:
-
- Capsaicin: A 2017 Cochrane review found capsaicin (8% patch) effective for postherpetic neuralgia, with additive effects when combined with systemic analgesics [18]. Its TRPV1 desensitization may enhance suzetrigine’s NaV1.8 blockade. Quality of evidence: moderate (based on capsaicin trials; no suzetrigine data).
- Topical NSAIDs (Diclofenac): A 2015 Cochrane review showed diclofenac gel’s efficacy in localized pain, with potential additive effects with systemic analgesics [19]. Quality of evidence: moderate.
- Menthol/Camphor: Limited studies show efficacy in musculoskeletal pain, with counterirritant effects potentially complementing suzetrigine [20]. Quality of evidence: low.
- Comparison with Opioids (Hydrocodone, Oxycodone):
-
- Evidence: Suzetrigine’s Phase 3 trials (NAVIGATE 1 and 2) showed efficacy over placebo but not hydrocodone/acetaminophen in acute pain [3]. Gabapentinoids enhance opioid analgesia (e.g., hydrocodone, oxycodone) in neuropathic pain, suggesting suzetrigine could benefit from similar combinations with gabapentin or pregabalin [27]. Topical alternatives (capsaicin, NSAIDs) reduce opioid requirements in multimodal regimens [18, 19].
- Relevance: Combining suzetrigine with gabapentinoids or topical agents may reduce reliance on high-dose opioids, addressing tolerance and OIH in patients [21].
Quality of Evidence
- Preclinical: Moderate. Studies show synergy between VGCC blockers (e.g., gabapentin, ziconotide) and opioids, supporting potential for suzetrigine combinations [23, 24]. No direct suzetrigine studies exist.
- Clinical: Low to moderate. Gabapentin and pregabalin have robust evidence for neuropathic pain, with synergy data for opioids but not suzetrigine [26, 27]. Topical gabapentin and alternatives (capsaicin, NSAIDs) show efficacy, but synergy with suzetrigine is theoretical [8, 18, 19]. Ziconotide’s synergy is limited by delivery constraints [15].
- Limitations: Suzetrigine’s recent approval (2025) limits combination studies. Gabapentinoids’ CNS side effects (e.g., sedation, dizziness) and potential for misuse in opioid-tolerant patients require caution [28]. Drug interactions (e.g., suzetrigine’s CYP3A induction affecting pregabalin) must be monitored [4].
Clinical Implications
- Synergistic Potential: Combining suzetrigine with gabapentin (topical/oral) or pregabalin may enhance analgesia by targeting NaV1.8 and VGCCs, addressing peripheral and central pain components. Topical alternatives (capsaicin, NSAIDs) could further reduce peripheral sensitization, while menthol/camphor offers sensory modulation. Ziconotide is less practical due to administration challenges [15].
- Practical Considerations:
- Dosing: Suzetrigine (100 mg loading, 50 mg q12h), gabapentin (topical: 6–10% cream; oral: 300–3600 mg/day), pregabalin (150–600 mg/day), capsaicin (8% patch), diclofenac (1–3% gel) [3, 8, 10, 18, 19].
- Drug Interactions: Monitor suzetrigine’s CYP3A induction with pregabalin; avoid strong CYP3A inhibitors [4]. Gabapentinoids increase sedation risk with opioids [28].
- Patient Selection: Ideal for patients with acute, neuropathic, or mixed pain, especially those with persistent opioid tolerance or OIH transitioning off high-dose opioids (e.g., morphine, hydrocodone, oxycodone) [21].
- Monitoring: One should monitor for side effects (suzetrigine: pruritus, rash; gabapentinoids: sedation, dizziness; capsaicin: burning sensation; ziconotide: CNS effects) and efficacy [3, 10, 15, 18].
Conclusion
The combination of Journavx (suzetrigine) with calcium channel blockers (gabapentin, pregabalin, ziconotide) and topical alternatives (capsaicin, NSAIDs, menthol/camphor) offers theoretical synergy based on complementary ion channel modulation and pain pathway targeting. Gabapentinoids and topical agents are most promising, with moderate evidence for neuropathic pain but limited direct data with suzetrigine. These combinations may reduce reliance on opioids like hydrocodone and oxycodone, addressing persistent tolerance and OIH in your patients. Clinical trials are needed to confirm synergy, and careful monitoring for side effects and interactions is essential.
References
- Osteen JD, et al. Pharmacology and mechanism of action of suzetrigine, a potent and selective NaV1.8 pain signal inhibitor for the treatment of moderate to severe pain. Pain Ther. 2025; Published online January 8. doi:10.1007/s40122-024-00697-0
- Vertex Pharmaceuticals. JOURNAVX (suzetrigine) [prescribing information]. Boston, MA; January 2025.
- Vertex Pharmaceuticals. Efficacy & Clinical Trials | JOURNAVX™ (suzetrigine). www.journavxhcp.com
- Drugs.com. Journavx: Uses, Dosage, Side Effects, Warnings. February 2, 2025. www.drugs.com
- Sutton KG, et al. Gabapentin inhibits high-threshold calcium channel currents in cultured rat dorsal root ganglion neurones. Br J Pharmacol. 2002;135:257–65. doi:10.1038/sj.bjp.0704439
- Field MJ, et al. Pregabalin as a pain therapeutic: Beyond calcium channels. Front Cell Neurosci. 2020;14:83. doi:10.3389/fncel.2020.00083
- Kukkar A, et al. Implications and mechanism of action of gabapentin in neuropathic pain. Arch Pharm Res. 2013;36:237–51. doi:10.1007/s12272-013-0057-y
- Hiom S, et al. Topical gabapentin gel for neuropathic pain: A review. J Pain Res. 2019;12:2341–50. doi:10.2147/JPR.S202143
- Bockbrader HN, et al. A comparison of the pharmacokinetics and pharmacodynamics of pregabalin and gabapentin. Clin Pharmacokinet. 2010;49:661–9. doi:10.2165/11536200-000000000-00000
- Goodman CW, et al. A clinical overview of off-label use of gabapentinoid drugs. JAMA Intern Med. 2019;179:695–701. doi:10.1001/jamainternmed.2019.0086
- Finnerup NB, et al. Pharmacotherapy for neuropathic pain in adults: A systematic review and meta-analysis. Lancet Neurol. 2015;14:162–73. doi:10.1016/S1474-4422(14)70251-0
- Bannister K, et al. Pregabalin suppresses spinal neuronal hyperexcitability in opioid-induced hyperalgesia. Anesth Analg. 2011;113:1093–100. doi:10.1213/ANE.0b013e31822c67b2
- Lyrica (pregabalin) [prescribing information]. Pfizer; 2023. www.accessdata.fda.gov
- Patel R, et al. Calcium channel modulation as a target in chronic pain control. Br J Pharmacol. 2018;175:2173–84. doi:10.1111/bph.13789
- McGivern JG. Ziconotide: A review of its pharmacology and use in the treatment of pain. Neuropsychiatr Dis Treat. 2007;3:69–85. doi:10.2147/nedt.2007.3.1.69
- McDonough SI. Calcium channel blocker challenges and successes in drug discovery. Wiley Interdiscip Rev Membr Transp Signal. 2013;2:85–97. doi:10.1002/wmts.65
- Flatters SJL, et al. Ethosuximide reverses paclitaxel- and vincristine-induced painful peripheral neuropathy. Pain. 2004;109:150–61. doi:10.1016/j.pain.2004.01.029
- Derry S, et al. Topical capsaicin (high concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2017;1:CD007393. doi:10.1002/14651858.CD007393.pub4
- Derry S, et al. Topical NSAIDs for acute musculoskeletal pain in adults. Cochrane Database Syst Rev. 2015;6:CD007402. doi:10.1002/14651858.CD007402.pub3
- Pergolizzi JV, et al. The role and mechanism of action of menthol in topical analgesic products. J Clin Pharm Ther. 2018;43:313–9. doi:10.1111/jcpt.12679
- Lee M, et al. A comprehensive review of opioid-induced hyperalgesia. Pain Physician. 2016;19:145–54.
- Roeckel LA, et al. Opioid-induced hyperalgesia: Cellular and molecular mechanisms. Neuropharmacology. 2019;151:104–11. doi:10.1016/j.neuropharm.2019.03.029
- Matthews EA, et al. Synergistic effects of gabapentin and morphine in animal models of neuropathic pain. Pain. 2002;95:1–9. doi:10.1016/S0304-3959(01)00363-9
- Kolosov A, et al. Intravenous injection of leconotide, an omega conotoxin: Synergistic antihyperalgesic effects with morphine in a rat model of bone cancer pain. Pain Med. 2011;12:923–31. doi:10.1111/j.1526-4637.2011.01127.x
- Dib-Hajj SD, et al. Voltage-gated sodium channels in pain states: Role in pathophysiology and targets for analgesic development. Pflugers Arch. 2010;460:1–17. doi:10.1007/s00424-009-0772-4
- Gilron I, et al. Nortriptyline and gabapentin, alone and in combination for neuropathic pain: A double-blind, randomised controlled crossover trial. Lancet. 2009;374:1252–61. doi:10.1016/S0140-6736(09)61081-3
- Hayashida K, et al. Gabapentin activates spinal noradrenergic activity in rats and humans and reduces hypersensitivity after surgery. Anesthesiology. 2007;106:557–62. doi:10.1097/01.anes.0000267597.30481.76
- Peckham AM, et al. Gabapentinoid misuse, abuse, and diversion: A systematic review. Pharmacotherapy. 2018;38:1114–23. doi:10.1002/phar.2182
References
- FDA. FDA approves novel non-opioid treatment for moderate to severe acute pain. January 30, 2025. www.fda.gov
- Drugs.com. Journavx: Uses, Dosage, Side Effects, Warnings. February 2, 2025. www.drugs.com
- Cummins TR, et al. The roles of sodium channels in nociception: Implications for mechanisms of pain. Pain. 2007;131:243–57. doi:10.1016/j.pain.2007.07.026
- Argoff CE. New analgesics for neuropathic pain: The lidocaine patch. Clin J Pain. 2000;16:S62–S65.
- van der Wal SE, et al. Molecular mechanisms of action of systemic lidocaine in acute and chronic pain: A narrative review. Br J Anaesth. 2019;123:335–49. doi:10.1016/j.bja.2019.06.014
- White HS. Molecular pharmacology of topiramate: Managing seizures and preventing migraine. CNS Drug Rev. 2005;11:191–208. doi:10.1111/j.1527-3458.2005.tb00270.x
- Silberstein SD. Topiramate in migraine prevention: A 2010 perspective. Headache. 2010;50:973–82. doi:10.1111/j.1526-4610.2010.01676.x
- Chong MS, Libretto SE. Topiramate in chronic pain management: A review of clinical efficacy. Pain Pract. 2003;3:111–20. doi:10.1046/j.1533-2500.2003.03016.x
- Dib-Hajj SD, et al. Voltage-gated sodium channels in pain states: Role in pathophysiology and targets for analgesic development. Pflugers Arch. 2010;460:1–17. doi:10.1007/s00424-009-0772-4
- Roeckel LA, et al. Opioid-induced hyperalgesia: Cellular and molecular mechanisms. Neuropharmacology. 2019;151:104–11. doi:10.1016/j.neuropharm.2019.03.029
- Attal N, et al. EFNS guidelines on pharmacological treatment of neuropathic pain. Eur J Neurol. 2006;13:1153–69. doi:10.1111/j.1468-1331.2006.01511.x
- Sawynok J. Topical analgesics in neuropathic pain. Curr Pharm Des. 2005;11:2995–3004. doi:10.2174/1381612054865091
- Keppel Hesselink JM. Topical phenytoin in painful diabetic neuropathy: Rationale to select a non-selective sodium channel blocker. Clin Res Neurol. 2018;1:1–5.
- Volpe DA, et al. Long-term opioid therapy: Assessment of consequences and risks. J Pain. 2018;19:685–94. doi:10.1016/j.jpain.2018.01.007
- Lee M, et al. A comprehensive review of opioid-induced hyperalgesia. Pain Physician. 2016;19:145–54.
References:
Suzetrigine
- Vertex Announces FDA Acceptance of New Drug Application for Suzetrigine for the Treatment of Moderate-to-Severe Acute Pain – 2024
- Selective Inhibition of NaV1.8 with VX-548 for Acute Pain – PubMed – 2023
- Sodium Channels in Pain – 2024
- www.sodiumchannels.com
- Nav1.7 and Nav1.8- Role in the pathophysiology of pain – 2019
- A Phase 3, Single-Arm Study of Suzetrigine, a Non-Opioid, Pain Signal Inhibitor For Treatment of Acute Pain From Surgical and Non-surgical Conditions 2024
Suzetrigine – Synergy
- Nav1.8, an analgesic target for nonpsychotomimetic phytocannabinoids – PubMed – 2025
- Non-psychotropic phytocannabinoid interactions with voltage-gated sodium channels- An update on cannabidiol and cannabigerol – 2022
- Sensory neuron sodium channels as pain targets; from cocaine to Journavx (VX-548, suzetrigine) – 2025
- Cannabidiol Inhibition of Murine Primary Nociceptors- Tight Binding to Slow Inactivated States of Nav1.8 Channels – 2021
Regulation of pain & ion channels
- Peripheral mechanisms of peripheral neuropathic pain – 2023
- Communicating pain – emerging axonal signaling in peripheral neuropathic pain – 2024
- Pain Management Strategies in Osteoarthritis – 2024
- Regulation of pain neurotransmitters and chondrocytes metabolism mediated by voltage-gated ion channels- A narrative review – 2023
- Ion channels involved in inflammation and pain in osteoarthritis and related musculoskeletal disorders – 2023
- Ion channels in osteoarthritis_ emerging roles and potential targets – PubMed – 2024
Acute Post-Injury Pain – Overviews
- Preventing chronic pain following acute pain – risk factors, preventive strategies, and their efficacy – 2011
- Ohio Guideline for the Management of Acute Pain Outside of Emergency Departments – 2016
- Clinical Practice Guidelines for Pain Management in Acute Musculoskeletal Injury – 2019
- Medical Management of Acute Pain – 2019
- Pain Management Best Practices Inter-Agency Task Force Report – 2019
- Medical Management of Acute Pain – 2019
- Treatments for Acute Pain – A Systematic Review – 2020
- Best Practices Guidelines for Acute Pain Management in Trauma Patients – 2020
- chronic post-hernia repair pain-2023
Acute Post-Injury Pain – Acetaminophen (Tylenol)
- AM404, an inhibitor of anandamide uptake, prevents pain behaviour and modulates cytokine and apoptotic pathways in a rat model of neuropathic pain – 2006
- AM404, paracetamol metabolite, prevents prostaglandin synthesis in activated microglia by inhibiting COX activity – 2017
- First evidence of the conversion of paracetamol to AM404 in human cerebrospinal fluid – 2017
- Acetaminophen metabolites p-aminophenol and AM404 inhibit microglial activation – 2018
- Pharmacological Management of Adults with Chronic Non-Cancer Pain in General Practice – 2020
- Analgesic Effect of Acetaminophen – A Review of Known and Novel Mechanisms of Action – 2020
Acute Post-Injury Pain – Oxidative Stress
- Roles of Reactive Oxygen and Nitrogen Species in Pain – 2011
- Clinical Relevance of Biomarkers of Oxidative Stress – 2015
- The Interplay between Oxidative Stress, Exercise, and Pain in Health and Disease – Potential Role of Autonomic Regulation and Epigenetic Mechanisms – 2020
- Neuropathic Pain – Delving into the Oxidative Origin and the Possible Implication of Transient Receptor Potential Channels – 2018
Acute Post-Injury Pain – Massage
Massage for Low Back Pain – 2009
Acute Post-Injury Pain – Ultrasound Therapy
- Overview of Therapeutic Ultrasound Applications and Safety Considerations – 2012
- Randomized controlled study of the antinociceptive effect of ultrasound on trigger point sensitivity novel applications in myofascial therapy? – PubMed – 2007
- Effectiveness of ultrasound therapy for myofascial pain syndrome – a systematic review and meta-analysis – 2017
- Effect of Therapeutic Sequence of Hot Pack and Ultrasound on Physiological Response Over Trigger Point of Upper Trapezius – 2015
- Effectiveness of Ultrasound Therapy on Myofascial Pain Syndrome of the Upper Trapezius – Randomized, Single-Blind, Placebo-Controlled Study – 2018
Acute Post-Injury Pain – Muscle Relaxers
- Randomized-controlled trial of methocarbamol as a novel treatment for muscle cramps in cirrhotic patients – PubMed – 2019
- Randomized placebo-controlled study of baclofen in the treatment of muscle cramps in patients with liver cirrhosis – PubMed – 2016
- Pilot study of orphenadrine as a novel treatment for muscle cramps in patients with liver cirrhosis – 2018
Acute Post-Injury Pain – Myofascial Pain
- Effectiveness of Ultrasound Therapy on Myofascial Pain Syndrome of the Upper Trapezius – Randomized, Single-Blind, Placebo-Controlled Study – 2018
- Myofascial Pain Syndrome in the Elderly and Self-Exercise – A Single-Blind, Randomized, Controlled Trial – 2016
- Effect of Therapeutic Sequence of Hot Pack and Ultrasound on Physiological Response Over Trigger Point of Upper Trapezius – 2015
- Effectiveness of ultrasound therapy for myofascial pain syndrome – a systematic review and meta-analysis – 2017
- Randomized controlled study of the antinociceptive effect of ultrasound on trigger point sensitivity novel applications in myofascial therapy? – PubMed – 2007
Myofascial Pain – Muscle Cramps
- Association Between Long-term Quinine Exposure and All-Cause Mortality – 2017
- Muscle Cramps Do Not Improve With Correction of Vitamin D Insufficiency – 2019
- Criteria in diagnosing nocturnal leg cramps – a systematic review – 2017
- Treatment of nocturnal leg cramps by blockade of the medial branch of the deep peroneal nerve after lumbar spine surgery – 2015
- Nocturnal Cramps in Patients with Lumbar Spinal Canal Stenosis Treated Conservatively – A Prospective Study – 2014
- Magnesium – Biochemistry, Nutrition, Detection, and Social Impact of Diseases Linked to Its Deficiency – 2021
- What is the role of magnesium for skeletal muscle cramps? A Cochrane Review summary with commentary – 2021
- Magnesium for skeletal muscle cramps – PubMed – 2020
- Non‐drug therapies for lower limb muscle cramps – 2012
- Non-drug therapies for the secondary prevention of lower limb muscle cramps – PubMed – 2021
- Nocturnal leg cramps in older people – 2002
- Assessment – symptomatic treatment for muscle cramps (an evidence-based review) report of the therapeutics and technology assessment subcommittee of the American academy of neurology – PubMed – 2010
- A scoping review to identify and map the multidimensional domains of pain in adults with advanced liver disease – 2020
- Randomized-controlled trial of methocarbamol as a novel treatment for muscle cramps in cirrhotic patients – PubMed – 2019
- Randomized placebo-controlled study of baclofen in the treatment of muscle cramps in patients with liver cirrhosis – PubMed – 2016
- Pilot study of orphenadrine as a novel treatment for muscle cramps in patients with liver cirrhosis – 2018
Reducing Acute Post-Injury Pain – Physical Therapy
Preventing Pain Related to Surgery – Overviews
- perioperative-pain-management- 2007 pubmed-ncbi
- Pharmacotherapy for the prevention of chronic pain after surgery in adults (Review) – 2013
- optimizing-pain-management-to-facilitate-enhanced-recovery-after-surgery-pathways 2015 -pubmed-ncbi
- development-of-a-management-algorithm-for-post-operative-pain-mapp-after-total-knee-and-total-hip-replacement-2014
- Post-operative Opioid-Induced Hyperalgesia – ICM Case Summaries – 2016
- The Complexity Model – A Novel Approach to Improve Chronic Pain Care – 2014
- Postoperative_pain_from_mechanisms_to_treatment.
- Mechanisms of acute and chronic pain after surgery: update from findings in experimental animal models. – PubMed – NCBI – 2018
- Short-term pre- and post-operative stress prolongs incision-induced pain hypersensitivity without changing basal pain perception – 2015
- Age and preoperative pain are major confounders for sex differences in postoperative pain outcome – A prospective database analysis – 2017
- Optimizing pain management to facilitate Enhanced Recovery After Surgery pathways. – PubMed – NCBI – 2015
- Reward Circuitry Plasticity in Pain Perception and Modulation – 2017
- Surgically-Induced Neuropathic Pain (SNPP) – Understanding the Perioperative Process – 2013
- Preventing Chronic Pain following Acute Pain – Risk Factors, Preventive Strategies, and their Efficacy – 2011
- Regular physical activity prevents development of chronic pain and activation of central neurons – 2013
- Regional anaesthesia to prevent chronic pain after surgery – a Cochrane systematic review and meta-analysis – 2013
- Pharmacotherapy for the prevention of chronic pain after surgery in adults – 2017
- A systematic review of therapeutic interventions to reduce acute and chronic post-surgical pain after amputation, thoracotomy or mastectomy. – 2015
- Analysis of perioperative pain management in vascular surgery indicates that practice does not adhere with guidelines – a retrospective cross-sectional study – 2017
- Efficacy and safety of multimodal analgesic techniques for preventing chronic postsurgery pain under different surgical categories – a meta-analysis – 2017
- Postoperative pain—from mechanisms to treatment – 2017
- Local anaesthetics and regional anaesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children – 2018
- Chronic postsurgical pain – current evidence for prevention and management – 2018
- Preventive analgesia and novel strategies for the prevention of chronic post-surgical pain. – (2015)
- Poorly controlled postoperative pain – prevalence, consequences, and prevention – 2017
- Designing the ideal perioperative pain management plan starts with multimodal analgesia – 2018
- Special indications for Opioid Free Anaesthesia and Analgesia, patient and procedure related: Including obesity, sleep apnoea, chronic obstructive … – PubMed – NCBI – 2017
- Chronic pain patient and anaesthesia – 2019
- New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults – 2017
- Multimodal Analgesia, Current Concepts, and Acute Pain Considerations. – PubMed – NCBI -2017
- Recent Advances in Postoperative Pain Management – 2010
- Effect of perioperative systemic alpha2-agonists on postoperative morphine consumption and pain intensity – systematic review of randomized controlled trials- 2011
- Cannabinoids for Postoperative Pain – 2007
- Educating Patients Regarding Pain Management and Safe Opioid Use After Surgery – 2020
Preventing Pain Related to Surgery – Phantom Limb Pain
- Strategies for prevention of lower limb post-amputation pain: A clinical narrative review – 2018
- Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: a prospective, randomized, clinical trial. – PubMed – NCBI – 2011
- Chronic post-amputation pain – peri-operative management – Review 0- 2017
Reducing Acute Post-Injury Pain – Physical Therapy
Preventing Pain Related to Surgery – Enhanced Recovery After Surgery (ERAS)
- Enhanced Recovery After Surgery: A Review. – PubMed – NCBI – 2017
- Pain management within an enhanced recovery program after thoracic surgery – 2018
- Optimizing pain management to facilitate Enhanced Recovery After Surgery pathways. – PubMed – NCBI – 2015
Preventing Pain Related to Surgery – Neuroinflammation, Glial Cells & Mast Cells
- Involvement of mast cells in a mouse model of postoperative pain. – PubMed – NCBI – 2011
- An Inflammation-Centric View of Neurological Disease – Beyond the Neuron – 2018
- Rescue of Noradrenergic System as a Novel Pharmacological Strategy in the Treatment of Chronic Pain – Focus on Microglia Activation – 2019
Preventing Pain Related to Surgery – Resolving Inflammation
- Vagus nerve controls resolution and pro-resolving mediators of inflammation – 2014
- The Resolution Code of Acute Inflammation – Novel Pro-Resolving Lipid Mediators in Resolution – 2015
- Resolvins in inflammation: emergence of the pro-resolving superfamily of mediators. – PubMed – NCBI – 2018
- Resolvins and protectins – mediating solutions to inflammation – 2009
- Resolvins and inflammatory pain – 2011
- Resolution of inflammation – an integrated view – 2013
- Protectins and maresins – New pro-resolving families of mediators in acute inflammation and resolution bioactive metabolome – 2014
- Proresolving lipid mediators and mechanisms in the resolution of acute inflammation – 2014
- Novel Pro-Resolving Lipid Mediators in Inflammation Are Leads for Resolution Physiology – 2014
- Novel Anti-Inflammatory — Pro-Resolving Mediators and Their Receptors – 2011
- Lipid Mediators in the Resolution of Inflammation – 2015
- PPARγ activation ameliorates postoperative cognitive decline probably through suppressing hippocampal neuroinflammation in aged mice. – PubMed – NCBI – 2017
- Postoperative cognitive dysfunction in the aged: the collision of neuroinflammaging with perioperative neuroinflammation. – PubMed – NCBI – 2018
- The Role of Neuroinflammation in Postoperative Cognitive Dysfunction – Moving From Hypothesis to Treatment – 2018
- Treating inflammation and infection in the 21st century: new hints from decoding resolution mediators and mechanisms – 2017
- Structural Elucidation and Physiologic Functions of Specialized Pro-Resolving Mediators and Their Receptors – 2017
- LPS is a Switch for Inflammation in the Gut and Beyond
- Identification of specialized pro-resolving mediator clusters from healthy adults after intravenous low-dose endotoxin and omega-3 supplementation – a methodological validation – 2018
- The Protectin Family of Specialized Pro-resolving Mediators – Potent Immunoresolvents Enabling Innovative Approaches to Target Obesity and Diabetes – 2018
- Protectins and Maresins – New Pro-Resolving Families of Mediators in Acute Inflammation and Resolution Bioactive Metabolome – 2014
- Functional Metabolomics Reveals Novel Active Products in the DHA Metabolome – 2012
- Anti-Inflammatory and Pro-Resolving Lipid Mediators – 2009
Preventing Pain Related to Surgery – Alpha-2 Agonists
Preventing Pain Related to Surgery – Buprenorphine
- Role of buprenorphine in acute postoperative pain – 2016
- Efficacy and Safety of Transdermal Buprenorphine versus Oral Tramadol:Acetaminophen in Patients with Persistent Postoperative Pain after Spinal Surgery – 2017
- Low-dose buprenorphine infusion to prevent postoperative hyperalgesia in patients undergoing major lung surgery and remifentanil infusion a double-blind, randomized, active-controlled trial – 2017
Preventing Pain Related to Surgery – Diet
Preventing Pain Related to Surgery – Genetics
- genotyping-test-with-clinical-factors-better-management-of-acute-postoperative-pain-2015
- the-impact-of-genetic-variation-on-sensitivity-to-opioid-analgesics-in-patients-with-postoperative-pain-a-systematic-review-and-meta-analysis-2015
- Chronic postsurgical pain – is there a possible genetic link? – 2017
Preventing Pain Related to Surgery – Epigenetics
- Epigenetic-regulation-of-spinal-cord-gene-expression-controls-opioid-induced-hyperalgesia-2014
- Epigenetic-regulation-of-opioid-induced-hyperalgesia-dependence-and-tolerance-in-mice-2013
- Epigenetic-regulation-of-persistent-pain-2015
- Chronic-opioid-use-is-associated-with-increased-dna-methylation-correlating-with-increased-clinical-pain-pubmed-ncbi
- Could targeting epigenetic processes relieve chronic pain states? – PubMed – NCBI
- Epigenetic-mechanisms-of-chronic-pain-2015
- Telomeres and epigenetics – Potential relevance to chronic pain – 2012
- Epigenetics of chronic pain after thoracic surgery. – PubMed – NCBI
- Epigenetics-in-the-perioperative-period-2015
Preventing Pain Related to Surgery – Gabapentin & Pregabalin
- Do surgical patients benefit from perioperative gabapentin:pregabalin? A systematic review of efficacy and safety. – PubMed – NCBI
- Perioperative administration of gabapentin 1,200 mg day−1 and pregabalin 300 mg day−1 for pain following lumbar laminectomy and discectomy – 2011
- Preemptive use of gabapentin in abdominal hysterectomy: a systematic review and meta-analysis. – PubMed – NCBI
- The Effect of Gabapentin on Acute Postoperative Pain in Patients Undergoing Total Knee Arthroplasty – 2016
- The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. – PubMed – NCBI
- The use of gabapentin in the management of postoperative pain after total hip arthroplasty – 2016
- The use of gabapentin in the management of postoperative pain after total knee arthroplasty – 2016
- Use of gabapentin for perioperative pain control – A meta-analysis – 2007
- The efficacy of gabapentin:pregabalin in improving pain after tonsillectomy: A meta-analysis. – PubMed – NCBI
- Effects of gabapentin on postoperative pain, nausea and vomiting after abdominal hysterectomy: a double blind randomized clinical trial. – PubMed – NCBI
- Gabapentin and postoperative pain – a systematic review of randomized controlled trials 2006 – PubMed Health
- Preoperative Preemptive Drug Administration for Acute Postoperative Pain – A Systematic Review And Meta-Analysis – 2016
- the-effects-of-preoperative-oral-pregabalin-and-perioperative-intravenous-lidocaine-infusion-on-postoperative-morphine-requirement-in-patients-undergoing-laparatomy-2015
- perioperative-pain-management- 2007 pubmed-ncbi
- optimizing-pain-management-to-facilitate-enhanced-recovery-after-surgery-pathways 2015 -pubmed-ncbi
- Treatment_of_Neuropathic_Pain_The_Role_of_Unique_Opioid_Agents_-_2016
- The Anti-Allodynic Gabapentinoids – Myths, Paradoxes, and Acute Effects – 2016
- Gabapentinoids as a Part of Multi-modal Drug Regime for Pain Relief following Laproscopic Cholecystectomy: A Randomized Study – 2017
- Effects of pregabalin and gabapentin on postoperative pain and opioid consumption after laparoscopic cholecystectomy – 2017
- Do surgical patients benefit from perioperative gabapentin:pregabalin? A systematic review of efficacy and safety. – PubMed – NCBI
- Impact of pregabalin on acute and persistent postoperative pain: a systematic review and meta-analysis. – PubMed – NCBI
- Effects of pregabalin and gabapentin on postoperative pain and opioid consumption after laparoscopic cholecystectomy – 2017
- Effect of Perioperative Gabapentin on Postoperative Pain Resolution and Opioid Cessation in a Mixed Surgical Cohort – 2018
Preventing Pain Related to Surgery – Ketamine & NMDA Antagonists
- Role of Ketamine in Acute Postoperative Pain Management – A Narrative Review – 2015
- Perioperative ketamine for acute postoperative pain. – PubMed – NCBI
- Ketamine decreases postoperative pain scores in patients taking opioids for chronic pain: results of a prospective, randomized, double-blind study. – PubMed – NCBI
- Intraoperative ketamine reduces perioperative opiate consumption in opiate-dependent patients with chronic back pain undergoing back surgery. – PubMed – NCBI
- Ketamine as an Adjunct to Postoperative Pain Management in Opioid Tolerant Patients After Spinal Fusions – A Prospective Randomized Trial – 2007
- The efficacy of N-methyl-D-aspartate receptor antagonists on improving the postoperative pain intensity and satisfaction after remifentanil-based a… – PubMed – NCBI
- The clinical role of NMDA receptor antagonists for the treatment of postoperative pain. – PubMed – NCBI
- Ketamine – an old drug revitalized in pain medicine – 2017
- Effect of ketamine combined with magnesium sulfate in neuropathic pain patients (KETAPAIN) – study protocol for a randomized controlled trial – 2017
- A systematic review and meta-analysis of ketamine for the prevention of persistent post-surgical pain. – PubMed – NCBI – 2014
- Ketamine for pain – 2017
- Ketamine for pain management – 2018
- Butorphanol and Ketamine Combined in Infusion Solutions for Patient-Controlled Analgesia Administration – A Long-Term Stability Study – 2015
- Multimodal Analgesia, Current Concepts, and Acute Pain Considerations. – PubMed – NCBI -2017
Preventing Pain Related to Surgery – Magnesium
- Perioperative systemic magnesium to minimize postoperative pain: a meta-analysis of randomized controlled trials. – PubMed – NCBI
- Peri-operative intravenous administration of magnesium sulphate and postoperative pain – a meta-analysis – 2013
- Effect of magnesium sulfate on morphine activity retention to control pain after herniorrhaphy. – PubMed – NCBI
- Effect of ketamine combined with magnesium sulfate in neuropathic pain patients (KETAPAIN) – study protocol for a randomized controlled trial – 2017
Preventing Pain Related to Surgery – NSAIDs
See: NSAIDs
- Sulfonamide cross-reactivity: is there evidence to support broad cross-allergenicity? – PubMed – NCBI – 2013
- Should celecoxib be contraindicated in patients who are allergic to sulfonamides? Revisiting the meaning of ‘sulfa’ allergy. – PubMed – NCBI 2001
Preventing Pain Related to Surgery – Nefopam
- nefopam-after-total-hip-arthroplasty-role-in-multimodal-analgesia-pubmed-ncbi
- nefopam-analgesia-and-its-role-in-multimodal-analgesia-a-review-of-preclinical-and-clinical-studies-pubmed-ncbi
- preventive-analgesic-efficacy-of-nefopam-in-acute-and-chronic-pain-after-breast-cancer-surgery-2016
- neuronal-sensitization-and-its-behavioral-correlates-in-a-rat-model-of-neuropathy-are-prevented-by-a-cyclic-analog-of-orphenadrine-pubmed-ncbi
Preventing Pain Related to Surgery – Tapentadol (Nucynta)
Preventing Pain Related to Surgery – Vitamin C
Chronic Regional Pain Syndrome (CRPS)/Reflex Sympathetic Dystrophy (RSD)
- Efficacy of vitamin C in preventing complex regional pain syndrome after wrist fracture – A systematic review and meta-analysis – 2017
- [Vitamin C and prevention of reflex sympathetic dystrophy following surgical management of distal radius fractures]. – PubMed – NCBI
- Complex regional pain syndrome – recent updates – 2013
- Give vitamin C to avert lingering pain after fracture – 2008
- Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures – a randomised trial – 1999
- Effect of vitamin C on prevention of complex regional pain syndrome type I in foot and ankle surgery. – PubMed – NCBI – 2009
Preventing Pain Related to Surgery – Vitamin C
Lumbar Surgery
Preventing Pain Related to Surgery – Vitamin D
- The Preoperative Supplementation With Vitamin D Attenuated Pain Intensity and Reduced the Level of Pro-inflammatory Markers in Patients After Posterior Lumbar Interbody Fusion – 2019
- Vitamin D and Its Potential Interplay With Pain Signaling Pathways – 2020
- Vitamin D for the treatment of chronic painful conditions in adults – 2014
- Vitamin D in Pain Management – 2017
- Is there a role for vitamin D in the treatment of chronic pain? – 2017
- Vitamin D Deficiency and Pain – Clinical Evidence of Low Levels of Vitamin D and Supplementation in Chronic Pain States- 2015
Opioids – Transitioning from Short Term to Long Term Use
- How acute pain leads to chronic opioid use – 2018
- Characteristics of initial prescription episodes and likelihood of long-term opioid use – United States, 2006-2015
- New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults – 2017
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Please note also, that many of the benefits for medications described on this web site include “off-label” use for a medication. Off-label prescribing refers to the use of medication for a condition not named in its FDA approval. Physicians are free to prescribe any medication they want, as long as there is some evidence for usefulness. And remember that the lack of an FDA indication does not necessarily mean lack of efficacy—it sometimes means that no drug company has deemed the investment in clinical trials worth the eventual pay off.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
