Acute Pain:
Journavx (suzetrigine)
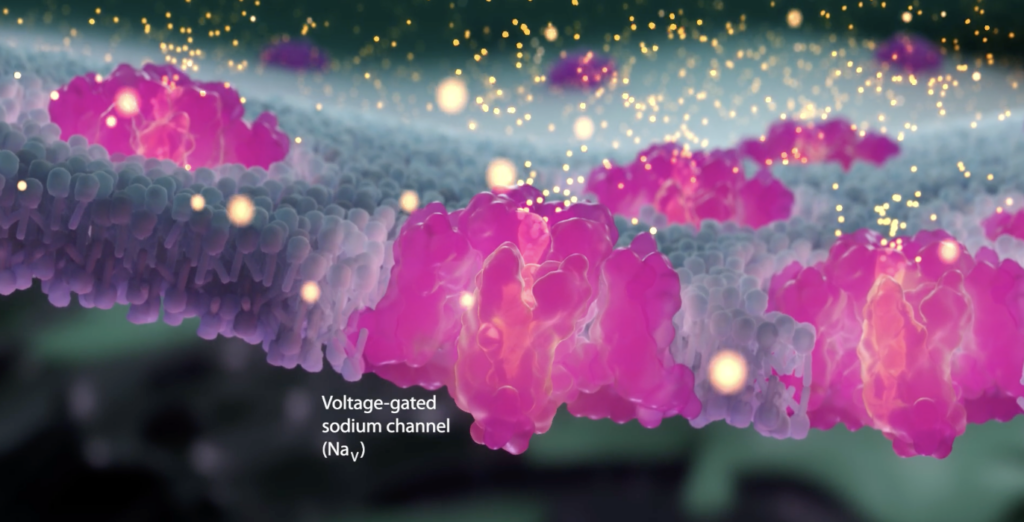
Vertex artist’s rendition of a sodium channel
Released in January 2025, Journavx (suzetrigine) is a new non-opioid medication for the treatment of moderate to severe acute pain, although not yet FDA approved for chronic pain. Journavx is the first of a new class of pain medications {Selective Nav1.8 inhibitors). This is the first new class of medicines to treat acute pain in over twenty years.
Of note, Journavx may also be useful for acute exacerbations of chronic pain. It is hoped that this new pain medication will offer an opportunity to not only lessen the experience of acute pain but also reduce the transition from acute to chronic pain. Additionally, there is is reason to believe that it may also reduce peripheral and central sensitization, two driving forces for chronic pain.
See:
See also:
- Acute Pain – Avoiding Transition to Chronic Pain
- The Transition of Acute Post-Injury Opioid Use to Chronic Opioid Use
- Omega 3 Fatty Acids
- Central Sensitization
- Neurobiology of Pain
- Gabapentin & Lyrica
- Palmitoylethanolamide (PEA)
- Dextromethorphan
- Ketamine
- Levorphanol
see also:
Definitions and Terms Related to Pain
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
What is Journavx (suzetrigine)?
Journavx (suzetrigine) is a first-in-its-class, new medication that relieves moderate to severe pain by a mechanism that is different from how other analgesic pain medications work, including acetaminophen (Tylenol), NSAIDs (ibuprofen, Aleve, Mobic etc.) and opioids. It works by inhibiting pain signals generated by pain receptors, for example when triggered by acute tissue damage, from being transmitted to the central nervous system and brain so as to reduce the perception of pain.
Since Journavx works via a unique mechanism, it can be taken along with other pain medications for added analgesic benefit. Because Journavx works on nerves in the peripheral nervous system and never enters the central nervous system or brain, it has no potential for addiction or contribution to accidental overdose if combined with opioids. Whether off-label use for chronic pain is effective has not been fully studied and it has not been approved for chronic pain at this time.
Although Journavx is currently FDA approved only for acute pain, is important to point out that it may actually have multiple benefits with respect to pain that as of yet have not been fully explored:
- Possible reduction of acute pain and acute exacerbation of chronic pain
- Possible suppression of transitioning of acute pain to becoming chronic
- Possible suppression of Peripheral and Central Sensitization
1. Reduction of Acute Pain and Acute Exacerbation of Chronic Pain
Acute pain is the first response to damaged tissue, followed by inflammation that triggers swelling of the area and promotes tissue repair. However, if the pain persists for more than 3 months, it is defined as chronic and it becomes a pathological condition in itself. This temporal parameter is used to define the distinction between acute and chronic pain because there are no biomarkers or measurable physiological conditions that distinguish acute from chronic pain.
Acute pain is most commonly experienced after surgery and after significant trauma. Therefore, Journavx should be considered as a potential treatment option for these pain conditions. It has been noted, however, that although Journavx has not yet been approved for acute exacerbation of chronic pain it could be considered under those circumstances as well. As a newly approved medication, there is a limited number of clinical studies demonstrating its benefits for pain.
Early Clinical Experience with Journavx for acute pain – The following studies have assessed Journavx treatment of a variety of acute pains:
(1) Acute surgical and 34 nonsurgical pain – A study of 222 surgical and 34 nonsurgical participants aged 18 to 80 who were experiencing moderate to severe acute pain from a broad range of surgical and non-surgical causes. Surgical cases were predominantly orthopedic (41.9%), plastic (37.4%), and ENT (10.8%), while nonsurgical cases included sprains and strains. Participants received suzetrigine (100 mg loading dose, then 50 mg every 12 hours), for up to 14 days or until their pain resolved.
At the end of treatment, 83.2% of participants rated suzetrigine as good, very good, or excellent for pain relief based on the patient global assessment. Suzetrigine was generally safe; most Side effects were mild to moderate – most commonly headache, occurring in 7% of patients.
(2) Ttummy tuck and bunionectomy – Two phase 2 clinical trials of Journavx have’been conducted involving participants with acute pain after abdominoplasty (tummy tuck) or bunionectomy. As compared to placebo, Journavx was found to be effective over 48 hours for the acute pain associated with these conditions. Reported side effects were only mild to moderate in severity but included headache, nausea, diarrhea or constipation, dizziness, and muscle spasms . (ClinicalTrials.gov numbers, NCT04977336 and NCT05034952).
Proposed benefits for acute exacerbations of chronic pain
(1) Acute Exacerbation of Chronic Osteoarthritis Pain – Osteoarthritis (OA) is a currently incurable, chronic, progressive, and debilitating musculoskeletal condition. One of its hallmark symptoms is chronic nociceptive (pain derived from tissue damage) and neuropathic (nerve) pain, which significantly reduces the quality of life of patients with OA. Although research into the mechanisms of OA pain is ongoing and several pain pathways are well understood, the true source of OA pain remains unclear. Voltage-gated sodium ion channels are key mediators of OA pain and are involved in all major synovial joint tissues in the context of pain generation. As such, this new class of medication may have the potential to target pain in patients with OA.
(2) Acute Exacerbation of Chronic Rotator Cuff Pain Chronic pain in biceps tendinopathy, characterized by pain and weakness in the tendon of the long head of biceps brachii muscle, is presumed to arise from neurogenic inflammation, central pain sensitization, excitatory nerve augmentation, inhibitory nerve loss, and/or dysregulation of supraspinal structures. Multiple ion channels are involved in these pain pathways including TRPV1 and 3, TRPA1, TRPM8, Nav1.7, Nav1.8, and Nav1.9, suggesting potential benefit of suzetrigine for acute rotator cuff injury.
Dosing for Acute Pain
The initial dose is two 50 mg tablets on an empty stomach, followed in 12 hours with a 50 mg dose, then 50 mg every 12 hours as needed.
Important Note Regarding Management of Acute Pain (including post-surgical pain)
In all cases, the management of any significant pain should be multimodal. In other words, acute pain should always be treated simultaneously with many different modes of treatment, including different classes of medications, dietary and nutraceutical supplements, and mind-body approaches along with physical therapy when indicated.
One should also bear in mind that there is growing evidence that the use of NSAIDs (ibuprofen, Aleve, Mobic, etc.) in the management of acute pain may be detrimental in the long run by contributing to a greater risk for the acute pain to transition to becoming a chronic pain.
See:
- Surgical Pain – Post-Operative
- Acute Pain: Initial Post-Injury
- Acute Pain – Avoiding Transition to Chronic Pain
2. Possible suppression of transitioning of acute pain to becoming chronic
Management of pain in the days and weeks after an injury is important in itself. But it is also important because how well that acute pain is managed can impact the ultimate duration and severity of that pain. The goal of pain management is not “zero pain” but pain that is tolerable and allows the patient to function. What is most important to understand, however, is that the most significant, consistent factor contributing to the risk of progression of acute to chronic post-injury pain is the duration of severe acute post-injury pain which can lead to peripheral and central sensitization
A major area of interest in the world of pain management is how acute pain transitions to becoming chronic pain. This transition to chronic pain is often associated with both increased sensitivity to pain and a magnified severity of the pain experience, referred to as sensitization. In general, reducing the severity of acute pain reduces the likelihood of it evolving into chronic pain, so it is important to treat acute pain aggressively if necessary to reduce transitioning and potentially committing someone to lifelong pain. Since Journavx offers an additional means of effectively reducing the severity of acute pain, it is likely that Journavx may reduce the transitioning to chronic pain and in doing so, it may suppress the development of sensitization (See “Avoiding The Transition of Acute to Chronic Pain”).
This increased sensitivity (pain receptors react with lower thresholds of painful stimulation) and pain magnification is referred to as peripheral and central sensitization, depending on when it occurs in nerves outside (peripheral) or inside the central nervous system (spinal cord and brain).
Aside from concerns regarding loss or impairment of function after being injured, most people’s primary concern revolves around their new pain, it’s effective management and the concern of how long the pain is going to last. This is especially true for patients who already suffer from chronic pain prior to an acute injury or surgery. It has been shown that patients who already have chronic pain are more vulnerable to the transitioning of new acute pain conditions to be becoming chronic pain conditions, including development of peripheral and central sensitization (See below).
Given the potential for Journavx to offer the possibility of reducing the likelihood of this transition one should strongly consider a trial of Journavx for acute post-operative pain and moderate to severe post-traumatic pain. A trial should be considered for exacerbations of chronic pain conditions as well.
3. Possible suppression of Peripheral and Central Sensitization
To understand how Journavx may possibly contribute to the suppression of peripheral and sensitization, it is necessary to understand some of the details of how Journavx works.
How Journavx Works: NaV1.8 Sodium Channels and Pain Signaling
The experience of pain originates when pain receptors (nociceptors) at the site of injury are triggered and these receptors send signals along peripheral nerves in the form the form of action potentials. These action potentials propagate signals through the nerves in the peripheral nervous system (PNS), where they then enter the spinal cord and into the central nervous system (CNS). In the dorsal horn of the spinal cord these pain signals are then propagated to several brain regions resulting in the perception of pain.
The propagation of nerve signals is driven by voltage-gated sodium channels, or “NaV“s. In nerves, sodium channels are specialized membrane proteins that allow sodium ions to pass through the cell membrane. Sodium channels are primarily voltage-gated channels, meaning they open or close in response to changes in the electrical potential (voltage) across the cell membrane. These channels are crucial for generating and propagating action potentials, the electrical signals that allow nerve cells to communicate. They are found in excitable cells like neurons, muscle cells, and endocrine cells.
Following pain receptor stimulation, these sodium channels in pain-sensing nerves open, allowing an influx of sodium ions which generates action potentials (nerve impulses) that are transmitted to the brain. There are nine NaV subtypes distributed throughout the body and some of them are predominantly found in the CNS, while others are found in the heart or muscle.
Three NaV subtypes that are related to pain and are predominantly found in peripheral pain nerves are:
-
- NaV1.7 which are associated with certain neuropathies. Congenital absence of this channel manifests as lack of pain perception
- NaV1.8 which are associated with the transmission of nerve impulses from damaged or inflamed tissues and plays a crucial role in transmitting pain signals in the peripheral nervous system. It is found primarily in small-diameter sensory neurons in the dorsal root ganglion and trigeminal ganglion, which are involved in pain perception.
- NaV1.9 which are been associated with episodic pain syndromes.
After nerve injury or inflammation, Nav1.8 expression (population) increases in sensory nerves, further exacerbating neuronal hyperactivity and pain.Nav1.8 is responsible for the majority of sodium current during the upstroke of action potentials in nociceptors. Its fast recovery from inactivation allows sustained firing, which drives hyperexcitability and sensitization.
Journavx is highly selective for the inhibition of NaV1.8 relative to other NaV channels. NaV1.8 is a sodium channel that is mostly found in peripheral pain-sensing nerves (nociceptors), whose role is to transmit pain signals (action potentials) along peripheral nerve pathways, transmitting pain signals from the periphery to the spinal cord where the signals are then transmitted to the brain. By inhibiting the NAV 1.8 sodium channel. the transmission of pain signals is reduced by Journavx.
Other available sodium channel blockers are non-specific, meaning they block all sodium channels. For example, Novocain, lidocain or Bupivacaine, are non-specific and block all sodium channels on nerve cells. However, nonspecific sodium channel blockers have a major problem: they affect sodium channels in the brain which can cause loss of balance, double vision, sleepiness, and confusion.
Unlike non-specific sodium channel blockers (e.g., lidocaine), Journavx is is highly selective for Nav1.8 only, peripherally acting only and does not impact the brain. As a result, Journavx avoids CNS side effects such as sedation, respiratory depression and abuse or addiction risk. Who she
How Journavx may suppress the development of peripheral and central sensitization
Research continues in an effort to understand how NaV1.8 inhibitors such as Journavx may reduce the hypersensitivity to pain associated with the development of peripheral and central sensitization, including inflammatory and neuropathic (nerve) pain.
- Inflammatory pain occurs as a result of tissue injury and is linked to inflammation that results from the production and release of inflammatory compounds (mediators) such as cytokines and others. Inflammatory mediators are important for both types of sensitization, particularly peripheral sensitization. Chronic inflammatory changes in nerves leads to the generation and maintenance of peripheral and central sensitization that is associated with chronic inflammatory pain.
- Pain receptor (nociceptor) sensitization is characterized by the presence of spontaneous nerve discharges, decreased activation thresholds and an increase in responsiveness to stimuli. These alterations lead to the development of hypersensitivity to pain (hyperalgesia), perception of pain even when a stimulus is minor and would not appropriately be painful (allodynia) and spontaneous ongoing pain, which are all the hallmarks of abnormal neuropathic pain states. Sodium channels, including Nav1.8 play key roles inflammatory and neuropathic pain states.
- Nav1.8 is responsible for the majority of sodium current during the upstroke of action potentials in nociceptors. Its fast recovery from inactivation allows sustained firing, which drives sensitization and hyperexcitability. When nerves are hyperexcitable, they start to fire spontaneously, which creates pain in inflammatory and neuropathic pain conditions.
- Nav1.8 channels are highly populated in peripheral pain nerves and play a critical role in transmitting and amplifying pain signals. In the presence of acute injury or inflammation associated with severe or persisting triggering of pain receptors, Nav1.8 channels in these pain receptors become upregulated, or hyperexcitable. As a result, repetitive excessive pain impulses are transmitted inducing chronic pain and peripheral sensitization.
- Animal studies have established a role for Nav1.8 in chronic inflammatory pain. Modulation of Nav1.8 channels by inflammatory compounds such as prostaglandin E2 (PGE2) that are associated with tissue injury were found to increase pain receptor excitability and contribute to chronic inflammatory pain and peripheral sensitization.
- In a 2014 study Nav1.8 was shown to regulate sensory nerve excitability and contribute to peripheral sensitization associated with the development of chronic pain. It was determined that with inflammation Nav1.8 is up-regulated and associated with enhanced nerve excitability and Nav1.8 current activity. The study also concluded that ambroxol, an experimental Nav1.8 blocker, significantly reduced Nav1.8 current and blocked mechanical allodynia, a manifestation of peripheral sensitization.
- In primate studies, selective experimental Nav1.8 inhibitors (e.g., MSD199) reduced nerve activity (C-fiber) and heat hyperalgesia by normalizing neuronal excitability.
- In rodent neuropathic pain models, partial inhibition of Nav1.8 (e.g., 25% block) normalized hyperactive nerves and reversed mechanical allodynia. This demonstrates the possibility that there may be a role for Journavx or future Nav1.8 inhibitors for the management of peripheral neuropathies and other neuropathic pain conditions.
- Research has also identified a role of the Nav1.8 channel in the pathophysiology of chronic neuropathic pain. Studies suggests that the channel may be important for the development of abnormal nerve stimulation and hyperexcitability in uninjured nerves nearby injured nerves and these changes may be time-dependent.
These maladaptive changes in the properties of Nav1.8 channels precipitated by traumatic injury may likely be inhibited by NaV1.8 inhibitors such as Journavx. Nav1.8 inhibitors represent a promising strategy to prevent peripheral sensitization by targeting the root cause of neuronal hyperexcitability. See below for evidence supporting this strategy.
The progression of Peripheral to Central Sensitization
It should be noted that hypersensitivity following an injury is an important self-preservation mechanism, which protects an area of injury by continuously warning/reminding the brain to avoid further trauma or injury to this injured area. This facilitates healing of the injured tissue. Peripheral sensitization can therefore be a normal, protective process that should resolve as damaged tissue heals. When this hypersensitivity becomes prolonged, it becomes maladaptive and pathologic.
Peripheral sensation can lead to central sensitization. When the nervous system’s peripheral sensory neurons are repeatedly or intensely stimulated, they become more sensitive, reducing the threshold for activation and increasing their responsiveness to stimulation.
This heightened sensitivity in the peripheral nervous system can lead to changes in the central nervous system, where neurons in the spinal cord and brain become more easily activated and more responsive to both normal and non-noxious (non-painful) stimulation, creating central sensitization.
Enhanced central sensitivity results in increased pain perception, even in the absence of a clear source of pain.
Central sensitization can cause a variety of symptoms, including increased pain sensitivity, pain in areas where there is no tissue damage, and allodynia (pain from normally non-painful stimuli).
Peripheral vs Central Sensitization
Symptoms of peripheral sensitization can overlap with those of central sensitization. One difference between peripheral and central sensitization can be identified easily: peripheral sensitization becomes heat-sensitive whereas central sensitization does not.
Peripheral sensitization can be characterized by:
-
- Increased responsiveness and lowered firing thresholds of peripheral pain receptors
- activation of silent pain receptors (nociceptors) that increases the nociceptive receptor field
Primary hyperaglesia:
-
- Associated redness and swelling
- Heat hyperalgesia
- Pain may be responsive to NSAIDs
Signs that indicate peripheral sensitization is likely:
-
- Distribution of symptoms is within a discreet area of tissue damage
- Hyperalgesia at or close to the site of tissue damage
- Pain described as burning or deep and achy
- Pain worsens with heat
- Pain often present at night
Central sensitization can be characterized by:
Sensitization occurs at the spinal cord level, resulting in increased receptor field size and increased responsiveness/lowered threshold to noxious and non-noxious stimuli
Secondary hyperalgesia:
-
- Allodynia
- Diffuse, widespread pain (non-dermatomal)
- Temporal summation
- Pain is more responsive to anti-epileptic (gabapentin, Lyrica) or anti-depressant (Cymbalta) medications
Evidence that supports the use of NAV 1.8 inhibitors (Journavx) to reduce peripheral and central sensitization
As noted above, the management of acute pain treatment must be directed at avoiding the evolution of acute to chronic pain. Since the driving forces behind this transition include the development of peripheral, followed by central sensitization, factors that can reduce sensitization must be emphasized. These factors need to be multimodal, in other words, multiple different approaches should be engaged and the use of NAV 1.8 inhibitors represents only one possible option. For additional means of doing so, See: Avoiding transition of acute to chronic pain.
The hypothesis that NAV1.8 sodium channel inhibitors reduce both peripheral and central sensitization is supported by growing preclinical and clinical evidence, primarily based on the channel’s critical role in nociceptor excitability and pain signal transmission.
1. Role of NAV1.8 in Peripheral Sensitization:
Location & Function: NAV1.8 is predominantly expressed in small-diameter, unmyelinated (C-fiber) and thinly myelinated (Aδ-fiber) nociceptive sensory neurons (dorsal root ganglia, DRG). It conducts the majority of the depolarizing current during the action potential upstroke in these neurons, especially at depolarized membrane potentials common during inflammation.
Evidence that Journavx, a Nav1.8 inhibitor, may reduce the risk of Peripheral Sensitization:
Genetic Knockout Studies: Nav1.8-null mice show markedly reduced pain behaviors in models of inflammatory pain (e.g., CFA, carrageenan, FCA) and neuropathic pain (e.g., SNI, CCI), but relatively normal responses to acute noxious stimuli. This demonstrates NAV1.8’s necessity for heightened pain sensitivity during sensitization.
Reference: Akopian, A. N., et al. (1999). The tetrodotoxin-resistant sodium channel SNS has a specialized function in pain pathways. Nature Neuroscience, 2(6), 541-548.
Reference: Nassar, M. A., et al. (2004). Nociceptor-specific gene deletion reveals a major role for Nav1.7 (PN1) in acute and inflammatory pain. PNAS, 101(34), 12706-12711.
Pharmacological Blockade (Preclinical): Selective NAV1.8 inhibitors (e.g., VX-150, A-803467, PF-01247324) effectively reduce hyperalgesia and allodynia in rodent models of inflammatory and neuropathic pain. They suppress nociceptor firing evoked by inflammatory mediators or nerve injury.
Note: VX-150:
VX-150 and vixotrigine were early experimental NaV1.8 inhibitors developed by Vertex Pharmaceuticals. While showing promise in early trials, their development was discontinued and Journavx (suzetrigine) is the FDA-approved medication.
Reference: Jarvis, M. F., et al. (2007). A-803467, a potent and selective Nav1.8 sodium channel blocker, attenuates neuropathic and inflammatory pain in the rat. PNAS, 104(20), 8520-8525.
Reference: Payne, C. E., et al. (2015). A novel selective and orally bioavailable Nav1.8 channel blocker, PF-01247324, attenuates nociception and sensory neuron excitability. British Journal of Pharmacology, 172(10), 2654-2670.
Human Pain Models (Experimental): Selective NAV1.8 inhibitors (e.g., VX-150, PF-06305591) have shown efficacy in reducing capsaicin-induced secondary hyperalgesia (a key marker of peripheral sensitization) and UVB burn-induced hyperalgesia in healthy volunteers.
Reference: Kort, M. E., et al. (2010). Efficacy, safety, and tolerability of VX-150, a novel NaV1.8 inhibitor, in a randomized, double-blind, placebo-controlled, crossover study in healthy subjects. Journal of Pain, 11(4), S45.
Reference: Alexandrou, A. J., et al. (2016). Subtype-selective small molecule inhibitors reveal a fundamental role for Nav1.7 in nociceptor electrogenesis, axonal conduction and presynaptic release. PLoS One, 11(4), e0152405. (Includes data on PF-06305591 – Nav1.8 selective).
2. Role of NAV1.8 in Driving Central Sensitization:
Mechanism Link: Central sensitization involves hyperexcitability of spinal cord dorsal horn neurons, leading to amplified pain signaling (wind-up, LTP). It is primarily driven by excessive input from sensitized peripheral nociceptors. By reducing peripheral nociceptor hyperexcitability and firing frequency, NAV1.8 inhibitors reduce the barrage of nociceptive input into the spinal cord that initiates and maintains central sensitization.
Evidence for Reducing Central Sensitization:
Reduced Spinal Cord Neuronal Activity: Studies using selective NAV1.8 blockers show reduced evoked firing of wide dynamic range (WDR) neurons in the spinal dorsal horn in response to noxious stimuli in sensitized states (e.g., inflammatory or neuropathic pain models). This directly demonstrates attenuation of central hyperexcitability driven by peripheral input.
Reference: McGaraughty, S., et al. (2008). Effects of A-803467, a novel and selective NaV1.8 sodium channel blocker, on dorsal horn neuronal responses in a rat model of neuropathic pain. Anesthesia & Analgesia, 107(6), 2153-2159.
Reduced Wind-Up: NAV1.8 inhibitors can attenuate wind-up (a form of short-term central sensitization) in spinal cord neurons evoked by repetitive C-fiber stimulation.
Reference: Jarvis, M. F., et al. (2007). (See above, demonstrated reduced wind-up).
Reduced Central Sensitization Markers: Administration of NAV1.8 inhibitors reduces markers associated with central sensitization, such as c-Fos expression in the spinal dorsal horn in pain models.
C-Fos expression refers to the activation and increase of the protein c-Fos in cells, particularly neurons, which is used as a marker to map neuronal activation. For example, when neurons become active, c-Fos expression increases, allowing the identification of which nerves or brain regions are involved in a particular process, such as learning, memory, or drug-induced effects.
Reference: Xu, H., et al. (2021). The Nav1.8 channel blocker A-803467 inhibits the recruitment of spinal microglia and astrocytes and attenuates mechanical allodynia in a rat model of neuropathic pain. Brain Research Bulletin, 177, 151-162. (While focused on glia, c-Fos reduction is often seen).
Reduced Secondary Hyperalgesia in Humans: As mentioned above, the reduction of capsaicin-induced secondary hyperalgesia by NAV1.8 inhibitors in human volunteers is a strong indicator of reduced central sensitization. Secondary hyperalgesia relies on central sensitization mechanisms in the spinal cord.
Reference: Kort, M. E., et al. (2010). (See above).
Reference: Moyer, B. D., et al. (2018). Nav1.8 inhibition by VX-150/Journavx increases mechanical pain threshold in the human capsaicin model. Journal of Pain Research, 11, 1741-1751. (More detailed analysis of VX-150/Journavx effect on secondary hyperalgesia).
Evidence in Primate Spinal Cord: A highly selective NAV1.8 inhibitor (MRK-2) significantly reduced c-Fos expression in the superficial dorsal horn of non-human primates following UVB burn injury, providing translational evidence for reduced central neuronal activation.
Reference: Shields, S. D., et al. (2021). Pharmacological inhibition of NaV1.8 is analgesic in non-human primate models of inflammatory and neuropathic pain. Brain, 144(12), 3656-3669. (Key reference for central effect evidence)
3. Clinical Trial Evidence (Indirect Support):
While VX-150/Journavx is the only NAV1.8 inhibitor FDA-approved, clinical trials provide indirect support for the mechanism translating to clinical pain states involving sensitization:
VX-150 (Vixotrigine): Showed significant efficacy in Phase 2 trials for post-herpetic neuralgia (PHN) and small fiber neuropathy (SFN), both conditions involving significant peripheral and central sensitization. The efficacy in these neuropathic pain states supports the role of NAV1.8 in pathological pain signaling.
Reference: Price, N., et al. (2020). Efficacy and safety of vixotrigine in post-herpetic neuralgia: Results of a phase 2, randomized, double-blind, placebo-controlled study. Pain Medicine, 21(Supplement_1), S14-S22.
Other Candidates (e.g., Funapide, BIIB074/Vixotrigine): While development paths have been mixed (some discontinued for lack of efficacy in certain indications like osteoarthritis or trigeminal neuralgia), positive signals in specific pain states (like PHN) reinforce the potential utility in conditions driven by sensitization. The reasons for failure in some trials are complex and may relate to target engagement, patient selection, or trial design rather than invalidating the mechanism per se.
Key Limitations & Caveats
1. Central Penetration: Journavx has limited CNS penetration to avoid potential CNS side effects. Its primary site of action is the peripheral nerve terminal and the dorsal root ganglion (DRG) in the spinal cord. The reduction in central sensitization is primarily achieved by reducing the peripheral drive, not by directly blocking NAV1.8 channels within the spinal cord (where expression is very low). The primate study using a peripherally restricted inhibitor (MRK-2) showing reduced spinal c-Fos is strong evidence for this indirect mechanism.
Conclusion
Substantial evidence supports that NAV1.8 inhibitors reduce peripheral sensitization by directly dampening the hyperexcitability of nociceptors in response to inflammatory mediators and nerve injury. By reducing this abnormal peripheral input, they subsequently attenuate the development and maintenance of central sensitization in the spinal cord, as evidenced by reduced dorsal horn neuronal firing, wind-up, c-Fos expression, and secondary hyperalgesia in preclinical models and human experimental pain.
While primarily acting peripherally, their ability to modulate central sensitization pathways through reduced nociceptive drive is a key mechanism for their potential efficacy in treating chronic inflammatory and neuropathic pain conditions. The clinical trial results in conditions like PHN provide promising translational support for this dual effect.
References:
Suzetrigine
- Vertex Announces FDA Acceptance of New Drug Application for Suzetrigine for the Treatment of Moderate-to-Severe Acute Pain – 2024
- Selective Inhibition of NaV1.8 with VX-548 for Acute Pain – PubMed – 2023
- Sodium Channels in Pain – 2024
- www.sodiumchannels.com
- Nav1.7 and Nav1.8- Role in the pathophysiology of pain – 2019
- A Phase 3, Single-Arm Study of Suzetrigine, a Non-Opioid, Pain Signal Inhibitor For Treatment of Acute Pain From Surgical and Non-surgical Conditions 2024
Suzetrigine – Synergy
Regulation of pain & ion channels
- Peripheral mechanisms of peripheral neuropathic pain – 2023
- Communicating pain – emerging axonal signaling in peripheral neuropathic pain – 2024
- Pain Management Strategies in Osteoarthritis – 2024
- Regulation of pain neurotransmitters and chondrocytes metabolism mediated by voltage-gated ion channels- A narrative review – 2023
- Ion channels involved in inflammation and pain in osteoarthritis and related musculoskeletal disorders – 2023
- Ion channels in osteoarthritis_ emerging roles and potential targets – PubMed – 2024
Acute Post-Injury Pain – Overviews
- Preventing chronic pain following acute pain – risk factors, preventive strategies, and their efficacy – 2011
- Ohio Guideline for the Management of Acute Pain Outside of Emergency Departments – 2016
- Clinical Practice Guidelines for Pain Management in Acute Musculoskeletal Injury – 2019
- Medical Management of Acute Pain – 2019
- Pain Management Best Practices Inter-Agency Task Force Report – 2019
- Medical Management of Acute Pain – 2019
- Treatments for Acute Pain – A Systematic Review – 2020
- Best Practices Guidelines for Acute Pain Management in Trauma Patients – 2020
- chronic post-hernia repair pain-2023
Acute Post-Injury Pain – Acetaminophen (Tylenol)
- AM404, an inhibitor of anandamide uptake, prevents pain behaviour and modulates cytokine and apoptotic pathways in a rat model of neuropathic pain – 2006
- AM404, paracetamol metabolite, prevents prostaglandin synthesis in activated microglia by inhibiting COX activity – 2017
- First evidence of the conversion of paracetamol to AM404 in human cerebrospinal fluid – 2017
- Acetaminophen metabolites p-aminophenol and AM404 inhibit microglial activation – 2018
- Pharmacological Management of Adults with Chronic Non-Cancer Pain in General Practice – 2020
- Analgesic Effect of Acetaminophen – A Review of Known and Novel Mechanisms of Action – 2020
Acute Post-Injury Pain – Oxidative Stress
- Roles of Reactive Oxygen and Nitrogen Species in Pain – 2011
- Clinical Relevance of Biomarkers of Oxidative Stress – 2015
- The Interplay between Oxidative Stress, Exercise, and Pain in Health and Disease – Potential Role of Autonomic Regulation and Epigenetic Mechanisms – 2020
- Neuropathic Pain – Delving into the Oxidative Origin and the Possible Implication of Transient Receptor Potential Channels – 2018
Acute Post-Injury Pain – Massage
Massage for Low Back Pain – 2009
Acute Post-Injury Pain – Ultrasound Therapy
- Overview of Therapeutic Ultrasound Applications and Safety Considerations – 2012
- Randomized controlled study of the antinociceptive effect of ultrasound on trigger point sensitivity novel applications in myofascial therapy? – PubMed – 2007
- Effectiveness of ultrasound therapy for myofascial pain syndrome – a systematic review and meta-analysis – 2017
- Effect of Therapeutic Sequence of Hot Pack and Ultrasound on Physiological Response Over Trigger Point of Upper Trapezius – 2015
- Effectiveness of Ultrasound Therapy on Myofascial Pain Syndrome of the Upper Trapezius – Randomized, Single-Blind, Placebo-Controlled Study – 2018
Acute Post-Injury Pain – Muscle Relaxers
- Randomized-controlled trial of methocarbamol as a novel treatment for muscle cramps in cirrhotic patients – PubMed – 2019
- Randomized placebo-controlled study of baclofen in the treatment of muscle cramps in patients with liver cirrhosis – PubMed – 2016
- Pilot study of orphenadrine as a novel treatment for muscle cramps in patients with liver cirrhosis – 2018
Acute Post-Injury Pain – Myofascial Pain
- Effectiveness of Ultrasound Therapy on Myofascial Pain Syndrome of the Upper Trapezius – Randomized, Single-Blind, Placebo-Controlled Study – 2018
- Myofascial Pain Syndrome in the Elderly and Self-Exercise – A Single-Blind, Randomized, Controlled Trial – 2016
- Effect of Therapeutic Sequence of Hot Pack and Ultrasound on Physiological Response Over Trigger Point of Upper Trapezius – 2015
- Effectiveness of ultrasound therapy for myofascial pain syndrome – a systematic review and meta-analysis – 2017
- Randomized controlled study of the antinociceptive effect of ultrasound on trigger point sensitivity novel applications in myofascial therapy? – PubMed – 2007
Myofascial Pain – Muscle Cramps
- Association Between Long-term Quinine Exposure and All-Cause Mortality – 2017
- Muscle Cramps Do Not Improve With Correction of Vitamin D Insufficiency – 2019
- Criteria in diagnosing nocturnal leg cramps – a systematic review – 2017
- Treatment of nocturnal leg cramps by blockade of the medial branch of the deep peroneal nerve after lumbar spine surgery – 2015
- Nocturnal Cramps in Patients with Lumbar Spinal Canal Stenosis Treated Conservatively – A Prospective Study – 2014
- Magnesium – Biochemistry, Nutrition, Detection, and Social Impact of Diseases Linked to Its Deficiency – 2021
- What is the role of magnesium for skeletal muscle cramps? A Cochrane Review summary with commentary – 2021
- Magnesium for skeletal muscle cramps – PubMed – 2020
- Non‐drug therapies for lower limb muscle cramps – 2012
- Non-drug therapies for the secondary prevention of lower limb muscle cramps – PubMed – 2021
- Nocturnal leg cramps in older people – 2002
- Assessment – symptomatic treatment for muscle cramps (an evidence-based review) report of the therapeutics and technology assessment subcommittee of the American academy of neurology – PubMed – 2010
- A scoping review to identify and map the multidimensional domains of pain in adults with advanced liver disease – 2020
- Randomized-controlled trial of methocarbamol as a novel treatment for muscle cramps in cirrhotic patients – PubMed – 2019
- Randomized placebo-controlled study of baclofen in the treatment of muscle cramps in patients with liver cirrhosis – PubMed – 2016
- Pilot study of orphenadrine as a novel treatment for muscle cramps in patients with liver cirrhosis – 2018
Reducing Acute Post-Injury Pain – Physical Therapy
Preventing Pain Related to Surgery – Overviews
- perioperative-pain-management- 2007 pubmed-ncbi
- Pharmacotherapy for the prevention of chronic pain after surgery in adults (Review) – 2013
- optimizing-pain-management-to-facilitate-enhanced-recovery-after-surgery-pathways 2015 -pubmed-ncbi
- development-of-a-management-algorithm-for-post-operative-pain-mapp-after-total-knee-and-total-hip-replacement-2014
- Post-operative Opioid-Induced Hyperalgesia – ICM Case Summaries – 2016
- The Complexity Model – A Novel Approach to Improve Chronic Pain Care – 2014
- Postoperative_pain_from_mechanisms_to_treatment.
- Mechanisms of acute and chronic pain after surgery: update from findings in experimental animal models. – PubMed – NCBI – 2018
- Short-term pre- and post-operative stress prolongs incision-induced pain hypersensitivity without changing basal pain perception – 2015
- Age and preoperative pain are major confounders for sex differences in postoperative pain outcome – A prospective database analysis – 2017
- Optimizing pain management to facilitate Enhanced Recovery After Surgery pathways. – PubMed – NCBI – 2015
- Reward Circuitry Plasticity in Pain Perception and Modulation – 2017
- Surgically-Induced Neuropathic Pain (SNPP) – Understanding the Perioperative Process – 2013
- Preventing Chronic Pain following Acute Pain – Risk Factors, Preventive Strategies, and their Efficacy – 2011
- Regular physical activity prevents development of chronic pain and activation of central neurons – 2013
- Regional anaesthesia to prevent chronic pain after surgery – a Cochrane systematic review and meta-analysis – 2013
- Pharmacotherapy for the prevention of chronic pain after surgery in adults – 2017
- A systematic review of therapeutic interventions to reduce acute and chronic post-surgical pain after amputation, thoracotomy or mastectomy. – 2015
- Analysis of perioperative pain management in vascular surgery indicates that practice does not adhere with guidelines – a retrospective cross-sectional study – 2017
- Efficacy and safety of multimodal analgesic techniques for preventing chronic postsurgery pain under different surgical categories – a meta-analysis – 2017
- Postoperative pain—from mechanisms to treatment – 2017
- Local anaesthetics and regional anaesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children – 2018
- Chronic postsurgical pain – current evidence for prevention and management – 2018
- Preventive analgesia and novel strategies for the prevention of chronic post-surgical pain. – (2015)
- Poorly controlled postoperative pain – prevalence, consequences, and prevention – 2017
- Designing the ideal perioperative pain management plan starts with multimodal analgesia – 2018
- Special indications for Opioid Free Anaesthesia and Analgesia, patient and procedure related: Including obesity, sleep apnoea, chronic obstructive … – PubMed – NCBI – 2017
- Chronic pain patient and anaesthesia – 2019
- New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults – 2017
- Multimodal Analgesia, Current Concepts, and Acute Pain Considerations. – PubMed – NCBI -2017
- Recent Advances in Postoperative Pain Management – 2010
- Effect of perioperative systemic alpha2-agonists on postoperative morphine consumption and pain intensity – systematic review of randomized controlled trials- 2011
- Cannabinoids for Postoperative Pain – 2007
- Educating Patients Regarding Pain Management and Safe Opioid Use After Surgery – 2020
Preventing Pain Related to Surgery – Phantom Limb Pain
- Strategies for prevention of lower limb post-amputation pain: A clinical narrative review – 2018
- Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: a prospective, randomized, clinical trial. – PubMed – NCBI – 2011
- Chronic post-amputation pain – peri-operative management – Review 0- 2017
Reducing Acute Post-Injury Pain – Physical Therapy
Preventing Pain Related to Surgery – Enhanced Recovery After Surgery (ERAS)
- Enhanced Recovery After Surgery: A Review. – PubMed – NCBI – 2017
- Pain management within an enhanced recovery program after thoracic surgery – 2018
- Optimizing pain management to facilitate Enhanced Recovery After Surgery pathways. – PubMed – NCBI – 2015
Preventing Pain Related to Surgery – Neuroinflammation, Glial Cells & Mast Cells
- Involvement of mast cells in a mouse model of postoperative pain. – PubMed – NCBI – 2011
- An Inflammation-Centric View of Neurological Disease – Beyond the Neuron – 2018
- Rescue of Noradrenergic System as a Novel Pharmacological Strategy in the Treatment of Chronic Pain – Focus on Microglia Activation – 2019
Preventing Pain Related to Surgery – Resolving Inflammation
- Vagus nerve controls resolution and pro-resolving mediators of inflammation – 2014
- The Resolution Code of Acute Inflammation – Novel Pro-Resolving Lipid Mediators in Resolution – 2015
- Resolvins in inflammation: emergence of the pro-resolving superfamily of mediators. – PubMed – NCBI – 2018
- Resolvins and protectins – mediating solutions to inflammation – 2009
- Resolvins and inflammatory pain – 2011
- Resolution of inflammation – an integrated view – 2013
- Protectins and maresins – New pro-resolving families of mediators in acute inflammation and resolution bioactive metabolome – 2014
- Proresolving lipid mediators and mechanisms in the resolution of acute inflammation – 2014
- Novel Pro-Resolving Lipid Mediators in Inflammation Are Leads for Resolution Physiology – 2014
- Novel Anti-Inflammatory — Pro-Resolving Mediators and Their Receptors – 2011
- Lipid Mediators in the Resolution of Inflammation – 2015
- PPARγ activation ameliorates postoperative cognitive decline probably through suppressing hippocampal neuroinflammation in aged mice. – PubMed – NCBI – 2017
- Postoperative cognitive dysfunction in the aged: the collision of neuroinflammaging with perioperative neuroinflammation. – PubMed – NCBI – 2018
- The Role of Neuroinflammation in Postoperative Cognitive Dysfunction – Moving From Hypothesis to Treatment – 2018
- Treating inflammation and infection in the 21st century: new hints from decoding resolution mediators and mechanisms – 2017
- Structural Elucidation and Physiologic Functions of Specialized Pro-Resolving Mediators and Their Receptors – 2017
- LPS is a Switch for Inflammation in the Gut and Beyond
- Identification of specialized pro-resolving mediator clusters from healthy adults after intravenous low-dose endotoxin and omega-3 supplementation – a methodological validation – 2018
- The Protectin Family of Specialized Pro-resolving Mediators – Potent Immunoresolvents Enabling Innovative Approaches to Target Obesity and Diabetes – 2018
- Protectins and Maresins – New Pro-Resolving Families of Mediators in Acute Inflammation and Resolution Bioactive Metabolome – 2014
- Functional Metabolomics Reveals Novel Active Products in the DHA Metabolome – 2012
- Anti-Inflammatory and Pro-Resolving Lipid Mediators – 2009
Preventing Pain Related to Surgery – Alpha-2 Agonists
Preventing Pain Related to Surgery – Buprenorphine
- Role of buprenorphine in acute postoperative pain – 2016
- Efficacy and Safety of Transdermal Buprenorphine versus Oral Tramadol:Acetaminophen in Patients with Persistent Postoperative Pain after Spinal Surgery – 2017
- Low-dose buprenorphine infusion to prevent postoperative hyperalgesia in patients undergoing major lung surgery and remifentanil infusion a double-blind, randomized, active-controlled trial – 2017
Preventing Pain Related to Surgery – Diet
Preventing Pain Related to Surgery – Genetics
- genotyping-test-with-clinical-factors-better-management-of-acute-postoperative-pain-2015
- the-impact-of-genetic-variation-on-sensitivity-to-opioid-analgesics-in-patients-with-postoperative-pain-a-systematic-review-and-meta-analysis-2015
- Chronic postsurgical pain – is there a possible genetic link? – 2017
Preventing Pain Related to Surgery – Epigenetics
- Epigenetic-regulation-of-spinal-cord-gene-expression-controls-opioid-induced-hyperalgesia-2014
- Epigenetic-regulation-of-opioid-induced-hyperalgesia-dependence-and-tolerance-in-mice-2013
- Epigenetic-regulation-of-persistent-pain-2015
- Chronic-opioid-use-is-associated-with-increased-dna-methylation-correlating-with-increased-clinical-pain-pubmed-ncbi
- Could targeting epigenetic processes relieve chronic pain states? – PubMed – NCBI
- Epigenetic-mechanisms-of-chronic-pain-2015
- Telomeres and epigenetics – Potential relevance to chronic pain – 2012
- Epigenetics of chronic pain after thoracic surgery. – PubMed – NCBI
- Epigenetics-in-the-perioperative-period-2015
Preventing Pain Related to Surgery – Gabapentin & Pregabalin
- Do surgical patients benefit from perioperative gabapentin:pregabalin? A systematic review of efficacy and safety. – PubMed – NCBI
- Perioperative administration of gabapentin 1,200 mg day−1 and pregabalin 300 mg day−1 for pain following lumbar laminectomy and discectomy – 2011
- Preemptive use of gabapentin in abdominal hysterectomy: a systematic review and meta-analysis. – PubMed – NCBI
- The Effect of Gabapentin on Acute Postoperative Pain in Patients Undergoing Total Knee Arthroplasty – 2016
- The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. – PubMed – NCBI
- The use of gabapentin in the management of postoperative pain after total hip arthroplasty – 2016
- The use of gabapentin in the management of postoperative pain after total knee arthroplasty – 2016
- Use of gabapentin for perioperative pain control – A meta-analysis – 2007
- The efficacy of gabapentin:pregabalin in improving pain after tonsillectomy: A meta-analysis. – PubMed – NCBI
- Effects of gabapentin on postoperative pain, nausea and vomiting after abdominal hysterectomy: a double blind randomized clinical trial. – PubMed – NCBI
- Gabapentin and postoperative pain – a systematic review of randomized controlled trials 2006 – PubMed Health
- Preoperative Preemptive Drug Administration for Acute Postoperative Pain – A Systematic Review And Meta-Analysis – 2016
- the-effects-of-preoperative-oral-pregabalin-and-perioperative-intravenous-lidocaine-infusion-on-postoperative-morphine-requirement-in-patients-undergoing-laparatomy-2015
- perioperative-pain-management- 2007 pubmed-ncbi
- optimizing-pain-management-to-facilitate-enhanced-recovery-after-surgery-pathways 2015 -pubmed-ncbi
- Treatment_of_Neuropathic_Pain_The_Role_of_Unique_Opioid_Agents_-_2016
- The Anti-Allodynic Gabapentinoids – Myths, Paradoxes, and Acute Effects – 2016
- Gabapentinoids as a Part of Multi-modal Drug Regime for Pain Relief following Laproscopic Cholecystectomy: A Randomized Study – 2017
- Effects of pregabalin and gabapentin on postoperative pain and opioid consumption after laparoscopic cholecystectomy – 2017
- Do surgical patients benefit from perioperative gabapentin:pregabalin? A systematic review of efficacy and safety. – PubMed – NCBI
- Impact of pregabalin on acute and persistent postoperative pain: a systematic review and meta-analysis. – PubMed – NCBI
- Effects of pregabalin and gabapentin on postoperative pain and opioid consumption after laparoscopic cholecystectomy – 2017
- Effect of Perioperative Gabapentin on Postoperative Pain Resolution and Opioid Cessation in a Mixed Surgical Cohort – 2018
Preventing Pain Related to Surgery – Ketamine & NMDA Antagonists
- Role of Ketamine in Acute Postoperative Pain Management – A Narrative Review – 2015
- Perioperative ketamine for acute postoperative pain. – PubMed – NCBI
- Ketamine decreases postoperative pain scores in patients taking opioids for chronic pain: results of a prospective, randomized, double-blind study. – PubMed – NCBI
- Intraoperative ketamine reduces perioperative opiate consumption in opiate-dependent patients with chronic back pain undergoing back surgery. – PubMed – NCBI
- Ketamine as an Adjunct to Postoperative Pain Management in Opioid Tolerant Patients After Spinal Fusions – A Prospective Randomized Trial – 2007
- The efficacy of N-methyl-D-aspartate receptor antagonists on improving the postoperative pain intensity and satisfaction after remifentanil-based a… – PubMed – NCBI
- The clinical role of NMDA receptor antagonists for the treatment of postoperative pain. – PubMed – NCBI
- Ketamine – an old drug revitalized in pain medicine – 2017
- Effect of ketamine combined with magnesium sulfate in neuropathic pain patients (KETAPAIN) – study protocol for a randomized controlled trial – 2017
- A systematic review and meta-analysis of ketamine for the prevention of persistent post-surgical pain. – PubMed – NCBI – 2014
- Ketamine for pain – 2017
- Ketamine for pain management – 2018
- Butorphanol and Ketamine Combined in Infusion Solutions for Patient-Controlled Analgesia Administration – A Long-Term Stability Study – 2015
- Multimodal Analgesia, Current Concepts, and Acute Pain Considerations. – PubMed – NCBI -2017
Preventing Pain Related to Surgery – Magnesium
- Perioperative systemic magnesium to minimize postoperative pain: a meta-analysis of randomized controlled trials. – PubMed – NCBI
- Peri-operative intravenous administration of magnesium sulphate and postoperative pain – a meta-analysis – 2013
- Effect of magnesium sulfate on morphine activity retention to control pain after herniorrhaphy. – PubMed – NCBI
- Effect of ketamine combined with magnesium sulfate in neuropathic pain patients (KETAPAIN) – study protocol for a randomized controlled trial – 2017
Preventing Pain Related to Surgery – NSAIDs
See: NSAIDs
- Sulfonamide cross-reactivity: is there evidence to support broad cross-allergenicity? – PubMed – NCBI – 2013
- Should celecoxib be contraindicated in patients who are allergic to sulfonamides? Revisiting the meaning of ‘sulfa’ allergy. – PubMed – NCBI 2001
Preventing Pain Related to Surgery – Nefopam
- nefopam-after-total-hip-arthroplasty-role-in-multimodal-analgesia-pubmed-ncbi
- nefopam-analgesia-and-its-role-in-multimodal-analgesia-a-review-of-preclinical-and-clinical-studies-pubmed-ncbi
- preventive-analgesic-efficacy-of-nefopam-in-acute-and-chronic-pain-after-breast-cancer-surgery-2016
- neuronal-sensitization-and-its-behavioral-correlates-in-a-rat-model-of-neuropathy-are-prevented-by-a-cyclic-analog-of-orphenadrine-pubmed-ncbi
Preventing Pain Related to Surgery – Tapentadol (Nucynta)
Preventing Pain Related to Surgery – Vitamin C
Chronic Regional Pain Syndrome (CRPS)/Reflex Sympathetic Dystrophy (RSD)
- Efficacy of vitamin C in preventing complex regional pain syndrome after wrist fracture – A systematic review and meta-analysis – 2017
- [Vitamin C and prevention of reflex sympathetic dystrophy following surgical management of distal radius fractures]. – PubMed – NCBI
- Complex regional pain syndrome – recent updates – 2013
- Give vitamin C to avert lingering pain after fracture – 2008
- Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures – a randomised trial – 1999
- Effect of vitamin C on prevention of complex regional pain syndrome type I in foot and ankle surgery. – PubMed – NCBI – 2009
Preventing Pain Related to Surgery – Vitamin C
Lumbar Surgery
Preventing Pain Related to Surgery – Vitamin D
- The Preoperative Supplementation With Vitamin D Attenuated Pain Intensity and Reduced the Level of Pro-inflammatory Markers in Patients After Posterior Lumbar Interbody Fusion – 2019
- Vitamin D and Its Potential Interplay With Pain Signaling Pathways – 2020
- Vitamin D for the treatment of chronic painful conditions in adults – 2014
- Vitamin D in Pain Management – 2017
- Is there a role for vitamin D in the treatment of chronic pain? – 2017
- Vitamin D Deficiency and Pain – Clinical Evidence of Low Levels of Vitamin D and Supplementation in Chronic Pain States- 2015
Opioids – Transitioning from Short Term to Long Term Use
- How acute pain leads to chronic opioid use – 2018
- Characteristics of initial prescription episodes and likelihood of long-term opioid use – United States, 2006-2015
- New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults – 2017
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Please note also, that many of the benefits for medications described on this web site include “off-label” use for a medication. Off-label prescribing refers to the use of medication for a condition not named in its FDA approval. Physicians are free to prescribe any medication they want, as long as there is some evidence for usefulness. And remember that the lack of an FDA indication does not necessarily mean lack of efficacy—it sometimes means that no drug company has deemed the investment in clinical trials worth the eventual pay off.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
