“If I can bring joy into the world, if I can get people to stop thinking about their pain for a moment, or the fact the tomorrow morning they’re going to get up and tell their boss off… then I’ll be successful.
– Bobby McFerrin
Mast Cell Activation Disease (MCAD)
Mast cells are immune cells that are manufactured in bone marrow and are distributed in all tissues of the body, especially at environmental interfaces. Mast cells react to potential threats to the body such as infection and mediate inflammatory responses such as hypersensitivity and allergic reactions.
Mast Cell Activation Disease (MCAD) is a condition associated with abnormal mast cells that feature dysregulated activation in response to threats or even inappropriate activation when there is no threat at all. When activated, mast cells release their contents, called mediators, which both promote and regulate activity in other cells related to immunological as well as non-immunological processes.
See:
Histamine Intolerance
Supplements:
Purchasing Supplements
To purchase supplements reviewed on this web site or discussed with Dr. Ehlenberger, a discount can be applied to usual commercial pricing by purchasing from Accurate Clinic’s online Supplement Store after acquiring the discount code from Accurate Clinic:
Accurate Clinic’s Supplement Store
or, call Toll-Free: 877-846-7122 (Option 1)
Resources:
.
Mast Cells
Mast cells function as sentinels or guards and are able to sense a wide range of potential injury to the body such as infections or environmental toxins. When a mast cell senses a threat, it “activates,” producing and releasing chemical “mediators” directed at assisting the body in managing the threat. They are primary players in allergic reactions and the inflammatory responses to injury and infection.
Mast cell activation is linked to certain cancers, cardiovascular diseases, connective tissue disorders, allergy, asthma and irritable bowel syndrome (IBS). Mast cell dysregulation can drive seasonal allergies and auto-immune conditions such as rheumatoid arthritis (RA) and Lupus. Mast cells and inflammation of the brain have been linked to depression, anxiety and other mental health conditions. They may also be linked to Ehler Danlos Syndrome, autonomic dysfunction (dysautonomia) celiac disease and Interstitial Cystitis (IC).
Mast cells have also been implicated in the evolution of central sensitivity, an important facet of chronic pain. Therapy directed at mast cells holds promise as a means of managing chronic pain.
Understanding Activated Mast Cells
The underlying feature of mast cell disorders is inappropriate mast cell activation. When activation is triggered, mast cells release their contents, mediators, with over 200 different mediators identified. People with mast cell activation may experience episodes of severe symptoms that last 15-30 minutes or longer. These mediators can result in a multitude of symptoms including:
- Skin rashes, itching or flushing
- Flushing
- Abdominal pain and/or bloating
- Nausea & vomiting or diarrhea
- Headache
- Muscle and joint pain
- Bone pain and skeletal lesions
- Mood changes including depression
- Anxiety
- Fatigue (tiredness)
- Allergic reactions, including an increased risk of anaphylaxis, a medical emergency
Triggers that can activate mast cells include:
- Heat
- Cold
- Abrupt changes in temperature
- Sunlight
- Physical exertion/fatigue
- Stress or emotional upset
- Perfumes or odors
- Medications such as antibiotics, certain anesthetics, NSAIDs (ibuprofen, toradol)
- Certain opioids: morphine, demerol
- Aspirin (however, aspirin can also be used as a treatment for those with high prostaglandin levels
- Topical medications: benzocaine.
- Venomous stings/bites: bees, wasps, hornets, spiders, jellyfish and snakes
- Foods: shellfish, peanuts, nuts, citrus, and high histamine foods
- Infections: viruses, bacterial and fungal
Delayed reactions may occur in mast cell activation patients when encountering a trigger or allergen to which they are allergic. There are acute, protracted and delayed phases of reactions. The immediate phase is within minutes to hours, the protracted phase is up to 8 hours and the delayed reactions occur up to 24-48 hours after exposure to the trigger. Less than 1% of patients present only the delayed phase. In mast cell activation patients, foods and environmental triggers can induce delayed reactions up to 24-48 hours due to delayed absorption and delayed metabolism. It is a good idea to keep a diary when a reaction has occured to facilitate tracing to a trigger.
Due to the increased risk for severe allergic reactions, all mast cell disorder patients should carry two doses of self-injectable epinephrine (Epi-Pen), unless otherwise contraindicated. Glucagon may need to be administered for patients on beta-blockers. It is important to self-administer the epinephrine while lying down, to maximize rapid absorption of the drug.
Certain medications have been identified as potential triggers for mast cell activation and should be avoided or used with caution in MCAD (See list).
Mast Cell Activation Disease (MCAD)
Mast Cell Activation Disease (MCAD) comprises a collection of disorders characterized by (1) accumulation of genetically altered or dysregulated mast cells and/or (2) abnormal release of these cells’ mediators. These mediators affect functions in potentially every organ system, often without causing abnormalities in routine laboratory or radiologic testing.
MCAD has recently become appreciated to be fairly common and thus should be considered routinely in the differential diagnosis of patients with chronic multi-system poly-morbidity or patients in whom a definitively diagnosed major illness does not well account for the entirety of the patient’s presentation. It has been proposed that MCAD may actually masquerade as a subset of various conditions such as fibromyalgia, irritable bowel syndrome and interstitial cystitis.
Symptoms often manifest initially from infancy to adolescence but are recognized only in retrospect as MCAD-related. Symptoms often occur in a temporally staggered fashion, waxing and waning over years to decades. Patients with most types of MCAD often initially enjoy symptom-free periods interspersed with symptomatic periods. Over time, symptom-free intervals shorten, and then symptoms become chronic with fluctuating intensity but with an overall trend toward steadily increasing intensity. Symptoms may involve multiple organ systems including skin, endocrine, gastrointestional tract, liver, cardiovascular and may include neuropsychiatric conditions.
Diagnoses Related to Mast Cell Activation Disease (MCAD)
Diagnostic terminology related to the condition of Mast Cell Activation Disease (MCAD) can be a little confusing. MCAD is an umbrella term that includes Mast Cell Activation Syndrome (MCAS) and Systemic Mastocytosis (SM). Those with SM have systemic reactions to mast cell-derived triggers and usually present with clinical signs of anaphylaxis, and some have an underlying IgE-dependent allergy.
MCAD may be primary or secondary. If it is primary, the condition is related to an underlying defect in the mast cells based on inherited or acquired genetic mutations. Most patients with secondary MCAD have an underlying IgE-dependent allergy but these remain at a higher risk of developing an MCAD. However, in some cases, an IgE-independent allergy or a suspected but not confirmed allergy (no allergen and/or specific IgE against allergens detected) is present. Rarely, an autoimmune disorder, chronic infection, or neoplastic or preneoplastic disorders is the cause. A patient may have both a primary and secondary MCAD, which is a high-risk situation. For example, a patient may have SM as well as a bee or wasp venom allergy. These patients usually require specific, chronic therapy.
Lastly, some patients fall into a third category when a primary cause is excluded and no secondary cause can be identified. This category is referred to as idiopathic MCAD.
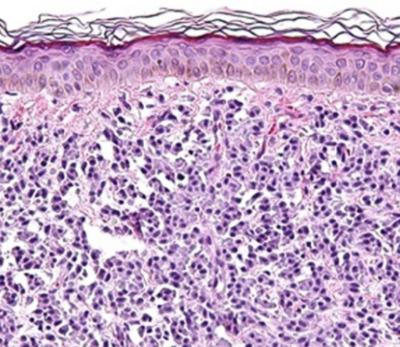
MCAS patients do not fulfill all criteria for SM but nevertheless exhibit typical symptoms although generally milder than those with SM. People with SM have bone marrow involvement in which the patient’s bone marrow produces too many mast cells that may be deformed and may not function properly or be easily activated. These cells may live longer than normal mast cells, leading to an increased number of mast cells. In MCADs, mast cells activate in abnormal ways in response to threats and may even activate when there is no threat at all. A diagnosis of SM has strict diagnostic criteria and is confirmed by a bone marrow or skin biopsy and is further divided into subtypes including:
- Cutaneous Mastocytosis (CM) – Affecting mainly children, mast cells gather in the skin but are not found in large numbers elsewhere in the body. The most common symptom of CM is abnormal growths (lesions) on the skin, such as bumps and spots, which can sometimes blister.
- Indolent mastocytosis (IM) – This accounts for about 90% of adult systemic mastocytosis cases. Symptoms vary from person to person and are usually mild to moderate but can be severe. Most patients with IM have skin involvement and may have benign organ involvement.
- Aggressive mastocytosis (AM) – In AM, symptoms are more wide-ranging and severe than IM. Mast cells multiply in organs including the spleen, liver, and digestive system, to the degree they compromise the functions of those organs.
- Systemic mastocytosis with associated blood (hematological) non-mast-cell-lineage disease (SM-AHNMD) – This diagnosis is applied when a malignancy such as leukemia develops together with systemic mastocytosis.
- Mast cell leukemia (MCL) – An advanced form of mastocytosis in which there usually are seen large numbers of mast cells circulating in the blood.
Causes of MCAD
The cause(s) of MCAD are not understood, but it is believed that there may be an association with mutations in kinases (particularly in the tyrosine kinase Kit) known as the KIT mutation which makes mast cells more sensitive to the effects of a signaling protein called stem cell factor (SCF). SCF plays an important role in the production and survival of blood cells and mast cells inside the bone marrow. In some cases of MCAD it appears the KIT mutation is inherited, but in most cases the mutation is acquired for no known reason. While the KIT mutation is necessary to develop a clonal mast cell population, other abnormalities yet to be determined must be added for the development of a clinically symptomatic disease.
Diagnosis of MCAD
MCAD should first be suspected on clinical findings, based on compatible mast cell mediator-related symptoms, sometimes including typical skin lesions. The clinical presentation of MCAD can be quite variable, due to both the widespread distribution of mast cells in the body and the wide range of abnormal patterns of mediator manifestation and symptoms that can occur in virtually any organs or tissue.
If clinical history suggests possible MCAD, consideration should be given to obtaining ultrasounds of internal organs: thyroid, liver, gall bladder and/or spleen. Gasroscopy and colonoscoy with biopsies, along with a bone density (DXA) scan should also be considered. When the above clinical information is consistent with the diagnosis of MCAD, skin or bone marrow biopsies are usually recommended to confirm and determine classification of the diagnosis. To establish the diagnosis of the rare patients with primary (i.e. clonal) MCAD, a very limited range of laboratory testing is routinely available such as the KIT mutational analysis.
MCAD in general has long been thought to be rare. However, although SM and MCL as defined by the WHO criteria are truly rare, it is likely that mast cell activation syndrome (MCAS) is fairly common with an estimated prevalence of 17% in the general population. Evidence suggests that pathological mast cells underlying MCAS are also involved in the etiology of many medical conditions including idiopathic anaphylaxis, interstitial cystitis, some subsets of fibromyalgia and irritable bowel syndrome, as well as neurologic and psychiatric symptoms and diseases.
MCAS is usually due to acquired mast cell clonality, driven by one of a large number of mast cell mutational profiles. Unfortunately, such mutational profiling in mast cells is not presently available in clinical laboratories. As such, the diagnosis of MCAS is necessarily based on clinical findings primarily, but there is still a lack of consensus among physicians as to the definitive criteria for its diagnosis.
Mast Cell Activation Syndrome (MCAS)
MCAS is a chronic multisystem disorder with inflammatory and allergic themes, and is diagnosed mainly by a clinical presentation and laboratory evidence consistent with chronic mast cell activation in the absence of any other diseases better accounting for all of the findings. They may or may not have increased mast cell mediators (commonly tryptase or histamine) during or shortly after an attack. These patients often respond to the same medications used to treat systemic mastocytosis.
Diagnosis of Mast Cell Activation Syndrome
- An MCAS patient must have signs/symptoms consistent with chronic mast cell activation (MCA) that are aberrant or abnormal, even if just to a modest degree or only episodic.
- An MCAS patient must have signs/symptoms of aberrant MCA in at least two organ systems
- An MCAS patient must not have another disease process that better accounts for the symptoms/signs
In addition to these criteria, as of 2020 there are two separate proposed consensus to further define the diagnosis of MCAS. The “consensus-1” proposal considers only severe, recurrent flares of a small number of specific symptoms in determining a diagnosis of MCAS. The “consensus-2” proposal considers a far wider range of symptoms which often respond to mast cell-targeted therapies, making the diagnosis reasonable to consider in appropriate clinical context.
The proposals also differ in their laboratory criteria. The consensus-1 requires that a rise in serum tryptase levels by at least 20% over the individual’s baseline tryptase level, plus 2 ng/mL of tryptase (eg, from 15 ng/mL baseline to at least 3 (20%) plus 2 ng/mL = 20 ng/mL; or from 40 ng/mL to at least 8 (20%) plus 2 ng/mL = 50 ng/mL) within a 3-4-hour window after the suspected MCAS episode or reaction. If a patient cannot be shown to have “20% + 2,” then elevations in a few other relatively mast cell-specific mediators can be considered diagnostic. These other mediators include prostaglandin D2 (PGD2) or its immediate 11-β-PGF2α metabolite, and the urinary histamine metabolite, N-methylhistamine (N-MH).
The “consensus-2” allows measure of a slightly wider range of mediators relatively specific to the mast cell, especially tryptase and heparin, which rise above their normal ranges to be taken as diagnostic laboratory evidence of MCAS in the proper clinical context. Like tryptase, heparin is highly specific to the mast cell, and research suggests an elevated plasma heparin level is likely the single most sensitive marker of MCAS, with 80% of patients who have symptoms consistent with MCAS showing increased levels of plasma heparin. Other mediators include chromogranin A (CgA), heparin, PGD2, histamine, N-MH, 11-β-PGF2α, and leukotriene E4 (LTE4).
Finally, the “consensus-1” diagnosis of MCAS requires that patients demonstrate at least a partial response to antihistamines and/or cromolyn as an essential diagnostic criterion, while the “consensus-2” diagnosis allows such a response to be considered a minor diagnostic criterion but not required.
Additional research is required to determine which proposed consensus will prove to be the best but in the meantime, diagnosing MCAS in routine clinical practice can be based on either of the two diagnostic criteria.
The next step: Who should be worked up for Mast Cell Activation Syndrome (MCAS)?
Evaluation for the possible diagnosis of MCAS should be considered in patients with multi-system symptoms as listed above, particularly those patients who’s symptoms are not well explained by previously established diagnoses. However, noting that MCAS may be associated with diagnoses that include conditions such as fibromyalgia, irritable bowel syndrome, interstitial cystitis, migraine headaches and others. Although it is believed that MCAS may be related to acquired mutations of genes associated with mast cell dysregulation, those patients with family histories positive for possible MCAS may particularly warrant investigation.
What is involved with the evaluation for MCAS?
The first step is to fill out a questionnaire designed to identify possible MCAS-related symptoms. If the questionnaire results suggest a reasonable possibility of MCAS, further assessment by a clinician may warrant consideration for laboratory evaluation that could include testing for mast cell-specific mediators in the blood (tryptase, heparin) or urine (histamine metabolite, N-methylhistamine (N-MH), depending on affordability.
The next step in the evaluation includes a trial course of treatment with dual histamine blockade for 2-4 weeks (for example, Zyrtec® (cetirizine) plus Pepcid® (famitodine) and the additional supplements, quercetin with vitamin C described below. If the course of treatment results in significant improvement in symptoms, the diagnosis may be established, especially if laboratory testing is positive.
However, given the episodic and intermittent nature of the symptoms related to MCAS, negative laboratory testing and/or an initial treatment trial that fails to identify benefit does not definitively exclude MCAS as a diagnosis. It may be appropriate to perform a repeat evaluation at another time when a patient is experiencing an exacerbation of their symptoms suspected to represent MCAS.
Other conditions that may mimic MCAD
There are many conditions that are associated with symptoms shared by MCAD and a detailed exploration of these conditions is beyond the scope of this page. However, malabsorption and food intolerance syndromes, particularly histamine intolerance (HIT), have been identified in up to 20% of the population in westernized countries with findings that can mimic or overlap with MCAD.
Histamine Intolerance (HIT)
Histamine Intolerance (HIT) is a condition associated with nonspecific gastrointestinal (GI) symptoms and extra-intestinal symptoms. In HIT, there is a disproportionate amount of histamine in the body which is thought to result from eating food with high histamine content along with having a reduced ability to digest histamine.
Symptoms associatecd with HIT include bloating as the most common symptom along with other symptoms such as postprandial fullness, diarrhea, abdominal pain, nausea, dizziness, headache, itching, flushing, rashes, runny nose, nasal congestion, sneezing, and shortness of breath.
See:Histamine Intolerance
COVID-19 and Mast Cell Activation
While in most cases of COVID-19 the clinical course is benign, in 15-20% of cases the disease is quite serious with a mortality rate of 3% or more, yet the specific causes of severe outcomes remain unclear. The one complication of COVID-19 responsible for the most severe cases and deaths is Severe Acute Respiratory Syndrome (SARS), which results in acute lung injury which may lead further to pulmonary and multi-organ failure. This condition appears linked to inflammatory processes caused by a “cytokine storm,” manifest as a hyper-immune response with pulmonary cytokines released in the lungs. Cytokines are protein substances such as histamine that are secreted by certain cells of the immune system, especially mast cells, that impact the function of other cells. Mast cells (MCs) are activated by SARS-CoV-2, the virus responsible for COVID-19.
A major goal of COVID-19 management is to prevent or reduce the severity of cytokine storm. It has been reasonably proposed the way to do so is to impact mast cells to reduce their release of cytokines, including histamine, through the use of mast cell stabilizer substances. Furthermore, it has been proposed to block the actions of cytokines such as histamine through the use of antihistamines (see below). If it is possible to blunt the cytokine system, the risk of progressing to severe and/or critical disease should lessen. (See: COVID-19).
COVID-19 Vaccinations
Treatment of Mast Cell Activation Disease (MCAD)
Because there is no cure for MCAD, the goal of treatment is to relieve the symptoms. Treatment options depend on the nature of the mast cell activity and the severity of the symptoms. The first step is to identify and reduce or avoid the individual patient’s unique triggers (chemical, physical, or otherwise), although it is not uncommon to have no identifiable, reliable trigger. Certain medications are best avoided by people with suspected MCAS/MCAD, particularly those medications known to trigger release of histamines (See list).
Treatment is then directed at two levels: (1) baseline chronic therapy to reduce mast cell activity and (2) symptomatic therapy directed at the individual’s specific symptomology. Emergency management of severe symptoms related to MCAD have been advised by the The Mast Cell Disease Society, Inc. and can be downloaded here.
Baseline therapy (continuous oral combination therapy to reduce mast cell activity)
(1) Antihistamines
Antihistamines are most commonly used to treat allergic symptoms such as hives and itching. Antihistamines block the effects of histamine, one of the major mediators released by activated mast cells, responsible for the wheal and flare of hives. There are 4 types of histamine receptors, H1-4.
Histamine receptors are transmembrane receptors on cells which mediate cellular responses to histamine, a mediator of an inflammatory response generated by mast cells. Currently, four histamine receptors have been identified, although medications have generally been directed only at H1 and H2 receptors. Histamine receptors are widely distributed in the body in nerve, smooth muscle (vascular, gastric and bronchial), blood, heart, immune system and the endocrine system.
Historically, histamine receptor antagonist medications are functionally targeted based on their properties: as anti-inflammatory (H1 receptors), anti-ulcer (H2 receptors) and sleep-inducing (H1 receptors). In some cases, “dual-histamine receptor blockade,” using both H1 and H2 antagonists in combination has been employed for treating conditions such as recurrent urticaria (hives). Unfortunately. there are currenttly no FDA-approved H1-H2 receptor combination drugs available.
H1 Antihistamines:
In the lung, the H1 receptors mediates the contraction of airway smooth muscle and is implicated in heightened airway hyperresponsiveness in COVID-19 (see above). Other effects of the H1 receptor include urticaria and increased vascular permeability. H1 antihistamines medications are histamine receptor antagonists that block activation of H1 receptors on mast cells and antagonize H1-mediated symptoms:
(a) Benadryl (diphenhydramine) or;
(b) Zyrtec® (cetirizine) or Xyzal(levocetirizine) or;
(c) Atarax/Vistaril (hydroxyzine)
H2 Antihistamines:
Similarly, these medications are histamine receptor antagonists that block activation of H2 receptors on mast cells and antagonize H2-mediated symptoms:
(a) Pepcid® (famitodine)
(b) Axid (Nizatidine)
(c) Tagamet (cimetidine)
Dual-histamine Receptor Blockade
The combined use of both H1 and H2 antihistamines, or “dual-histamine receptor blockade,” is recommended as baseline management of MCAD.
When the combination of cetirizine (10 mg twice a day) and famitodine (20 mg twice a day) was studied and reported in a June 2020 publication, it was found this c0mbination exhibited beneficial reductions in inpatient mortality and symptom progression. While this was a small “proof-of-concept” study that needs further research to confirm their findings, the authors concluded this dual combination is safe and effective in management of COVID-19.
Additionally, another COVID-19 study evaluaing famotidine alone in doses ranging from 10 to 40 mg found a reduced risk of death and intubation. In comparison, use of proton pump inhibitors (that reduce gastric acid independent of a histamine mechanism) were not associated with reduced risk of death or intubation, reinforcing the conclusion that the famotidine benefit is histamine-mediated.
Long term side effects with antihistamines
There is growing recognition of the detrimental effects on thinking (mental clouding and other cognitive impairments) caused by long term use of antihistamines. Patients at increased risk of this are patients >65 years and patients taking 50 mg of benadryl (diphenhydramine)/day for >3 years or doxepin (25 mg for 6 years). Also, high doses of sedating antihistamines such as diphenhydramine can cause increased seizure activity, seen mostly in children. A tolerance to or a dependence upon diphenhydramine may result in a need for even higher doses. Caution and restraint must be used when taking antihistamines long term and titrate to the lowest dose necessary to control symptoms.
Other Antihistamines
In addition to H1 and H2 antihistamines, it has also been proposed that antihistaminew with anti-eosinophilic action (ketotifen, rupatadine)
and antihistamines with anti-serotonin action (cyproheptadine)
be considered for trial. Tricyclic antidepressants with combined antihistamine action (doxepin) have also been suggested.
(3) Cromolyn sodium
Cromolyn is a mast cell stabilizers used to prevent asthma and symptoms of seasonal or chronic allergic rhinitis. It works by blocking a calcium channel that is essential for mast cell degranulation (the release of chemical mediator-containing secretory granules which occurs after exposure to a specific antigen). It has been successfully used in the management of inflammatory bowel diseases (ulceratice colitis, Crohn’s) and interstitial cystitis, conditions sometimes associated with dysregulated mast cell activity.
(4) Vitamin C
Vitamin C increases degradation of histamine and inhibits mast cell degranulation. Dosing limited to not more than 750 mg/day. Additionally, studies suggest that the combination of quercetin with Vitamin C offers a synergistic benefit.
Treatment of Anaphylaxis and Severe Allergic Reactions due to MCAS
In cases of life-threatening symptoms of MCAS such as anaphylaxis, the use of epinephrine (EpiPen, AnaPen) is indicated. Any patient with this history should always have a prescription of injectable epinephrine on hand.
Complementary and Alternative Medical (CAM) Therapy
Because conventional medical care for MCAD offers only imperfect relief for many afflicted patients, Complementary and Alternative Medicine (CAM) approaches are suggested to offer additional benefit. CAM treatment in this case includes the use of nutraceuticals. The term “nutraceutical,” derived from “nutrition” and “pharmaceutical,” refers to a product that is isolated from herbs, botanicals or foods that has physiological benefit by supporting the structure or function of the body or providing protection against diseases.
Palmitoylethanolamide (PEA)
Palmitoylethanolamide (PEA) is a naturally occuring, biologically active lipid that acts on the endocannabinoid system and interacts with inflammatory cells in the nervous system. Sometimes referred to as a cannabinomimetic compounds (i.e. an agents able to modulate endocannabinoid function), PEA has been shown to stabilize mast cells. What is particularly exciting about PEA is that it is a naturally occuring agent produced by the body that has no reported serious side effects or drug-drug interactions, making it an extraordinarily safe treatment option
While little research is available at this time on PEA in MCAD, it has preliminary research to suggest potential benefit.
See: Palmitoylethanolamide (PEA)
Flavonoids
Flavoniods with research-supported benefit for stabilizing mast cells include quercetin, luteolin and others.
Quercetin
Quercetin is the most plentiful, most studied representative of polyphenols, flavonoids subgroup, flavonols. Its main food sources include: onions, broccoli, apples, berries, grapes, some herbs, teaa and wine. While generally found at relatively low concentrations of 15–30 mg/kg (fresh weight), several vegetable varieties have much more extensive content such as onions and shallots.
Quercetin stabilizes mast cells and suppresses mast cell activity including the inhibition of histamine release, pro-inflammatory cytokines, leukotrienes creation, and suppression of interleukin IL-4 production.
Quercetin has strong antioxidant and anti-allergic properties and may reduce the inflammation involved with severe infection. It stimulates the immune system, and, has a broad range of antiviral properties which can potentially interfere with COVID-19 infection including virus entry into cells and virus replication.
The benefits of quercetin can be enhanced by the co-administration of vitamin C.
Cannabinoids
It appears that to date there is no high-quality research evaluating cannabinoids to treat patients with MCAS or mastocytosis. One must therefore turn to preclinical studies to judge their potential for benefit.
Early research suggests that cannabinoids stabilize mast cells. There are two primary cell receptors in the human endocannabinoid system, CB1 and CB2. CB1 receptors are abundantly present in the brain and spinal cord. They are found in very high concentration in the hypothalamus and the amygdala, which are responsible for appetite regulation, control of stress and anxiety, reducing nausea and memory and emotion processing. CB1 receptors are also present in nerve endings where they reduce pain sensations. CB2 receptors are mostly located in the immune cells of the peripheral nervous system and play a dominant role in reducing inflammation.
Mast cells contain both CB1 and CB2 receptors, which when activated inhibit mast cell release. Cannabinoids, both endocannabinoids (natural., manufactured in the body) and phytocannabinoids (found in mariuana) have been found to suppress mast cell degranulation, the process of releasing their mediators.
Cannabidiol (CBD) alone without THC may be less effective at treating dysfunctional mast cells because while THC has a strong binding affinity for both CB1 and CB2 receptors, CBD does not bind directly to either receptors but instead act indirectly through other pathways to reduce inflammation. However, anecdotally in the online MCAS community CBD seems to be helpful for some patients, particular those with high pain levels, inflammation, and insomnia.
Low Dose Naltrexone (LDN)
Naltrexone is an opioid antagonist that has been used conventionally for the treatment of alcoholism and opioid addiction. Low-dose naltrexone (LDN) is used off-label for treatment of pain and inflammation in many pain conditions including multiple sclerosis, Crohn’s disease and fibromyalgia. LDN inhibits cellular proliferation of T- and B- cells and block Toll-like receptor 4 (TLR4) and reduces production of multiple cytokines including IL-6, thought to be the mechanisms by which it provides anti-inflammatory benefit and pain relief. It has been proposed as an alternative treatment option to stabilize mast cells.
Ketamine
Ketamine has a pronounced inhibitory effect on mast cells.
Pain Related to MCAD
Mast cell activation results in many different symptoms including: hives, rash, anaphylaxis, hot flushing of skin, palpitations, nausea, fatigue, anxiety and pain. Pain is a common symptom in MCAD and may include headache, abdominal pain, skeletal pain, bone pain, muscle pain, joint pain, eye discomfort, and ear/nose/throat pain.
Mast cell-related pain is often described as migratory or referring to a particular area of the body or even the whole body. In a survey on symptoms of 420 patients with mast cell disorders, pain was reported in the chest (36.7%), stomach (72.9%), upper abdomen (46.4%), lower abdomen (56.4%), bones (56.4%), joints (61.4%), muscles, and nerves or connective tissues (50%). Pain can severely impact quality of life in MCAD patients.
Treatment of pain in MCAD can be very challenging, in part because of the difficulty in defining the source of the pain but also because the classical analgesics – most narcotics and non-steroidal anti-inflammatory drugs (NSAIDS) – can actually trigger MCAD and not only be ineffective but may make symptoms worse. Pain management in MCAD should be treated individually and whenever possible, directed at the specific mast cell mediator-related causes
Trigger-based Pain Management in MCAD
Because mast cells are found throughout the body, especially near environmental surfaces, their activation is often triggered by environmental factors and agents. On important family of triggers is food. As noted above, mast cell activation dysregulation often masquerades as, or misdiagnosed as, other conditions such as fibromyalgia, non-celiac gluten sensitivity and irritable bowel syndrome (IBS).
These conditions are often characterized by symptoms including abdominal pain, cramps, nausea and diarrhea that respond to elimination of specific foods in the diet that may trigger these symptoms. By avoidance of food containing gluten, cow’s milk proteins, beef, and baker’s yeast, all known mast cell triggers, a significant pain reduction can often be obtained. As such, an elimination diet should be the first therapeutic action before starting medication therapy.
Opioids in MACD
Patients suffering from mast cell activation symptoms with opioids should avoid codeine, morphine and meperidine (demerol), because of histamine-release. Some research suggests that tramadol and hydromorphone (dilaudid) are safer, while fentanyl does not appear to trigger mast cell activation.
In a 2004 report, the opiate codeine and the synthetic opioids meperidine, fentanyl, alfentanil, sufentanil, remifentanil, buprenorphine, and the opioid antagonist naloxone were tested. Only codeine and meperidine induced mast cell activation with the release of tryptase and histamine, leading to protein extravasation, flare reactions, and itch sensations. Because naloxone did not attenuate these effects, it is unlikely that μ-opioid receptors are involved in the activation of mast cells.
Muscle Pain
Approximately 75% of MCAD patients have muscle pain, often accompanied by peripheral (usually distal) sensory and/or motor neuropathies including paresthesias. Pain associated with release of mediators from mast cells in the muscle is often described as pulsatile, beginning suddenly with high intensity and also disappearing suddenly in varying locations.
Muscular pain can often be induced by applying pressure at points in muscles all over the body, characteristic also of fibromyalgia. In fact, a large number of patients with MCAD are diagnosed with fibromyalgia before their diagnosis of MCAD is made. It is believed that at least a subset of fibromyalgia may be a clinical manifestation of MCAD.
The pathogenesis of pain in these MCAD/FMS patients appears to be based on the activation of mast cells by locally released corticotrophin releasing hormone (CRH) and substance P via CRH and NK1 receptors, respectively. This activation can lead to a feed-forward neuroendocrine sensitization of the peripheral and central nervous system and increased pain. In addition, in the periphery, mast cells closely surrounding the primary afferent A, δ and C pain fibers trigger pain by releasing their mediators. This neuropathic pain is often poorly (if at all) responsive to the traditional drugs used to manage neuropathic pain and in fact, some of these drugs may actually worsen the severity of symptoms by further increasing mast cell activity.
Management of muscle pain in MCAD includes dose escalation of H1 antihistamines and dipyrone, warm epsom baths but NOT massage
Nerve Pain
Related to the release of mediators from mast cells located adjacent to pain fibers; nerve pain is of varying intensity and described as migratory or referring to a particular area of the body or generalized to the entire body. Traditional agents for nerve pain such as gabapentin (Neurontin) and pregabalin (Lyrica) may not be effective and topiramate (Topamax) may trigger worsening of mast cell activation.
Alternative compounds advised include palmitoylethanolamide (PEA) and alpha lipoic acid. Cannabinoids and minocycline have also been proposed as beneficial.
Bone Pain
Like muscle pain, bone pain associated with MCAD is often also pulsatile but sometimes boring in character and frequently begins and disappears suddenly and is often described as migratory. For treatment, dose escalation of an H1 antihistamine is advised along with dipyrone and in the case of osteopenia or osteoporosis, bisphosphonates may be recommended.
Drug Therapy of Intestinal Pain
Many patients with MCAD have complaints of abdominal pain and/or cramping often accompanied by bloating-gassiness diarrhea, constipation which are often diagnosed as irritable bowel syndrome (IBS). Research suggests mast cell infiltration and activation may cause many of the symptoms in IBS. The mast cell stabilizer, cromolyn, has been shown to reduce the visceral pain and hypersensitivity in many IBS patients and is also recommended to treat pain and intestinal symptoms in the MCAD. H2 antihistamines such as Pepsid (famotidine) is also recommended along with proton pump inhibitors such as prilosec. For diarrhea, montelukast and/or Zofran (ondansetron, a 5-HT3 receptor inhibitor) are advised. Cholestyramine and nystatin have also been suggested.
Drug Therapy of Headache/Migraine Syndromes
Migraines are episodic, typically unilateral, throbbing headaches that occur more frequently in patients with allergy and asthma implying involvement of meningeal and/or brain mast cells. Mast cells are definitive players in allergic reactions and are also in inflammatory diseases, especially asthma. Headache syndromes/migraine are present in more than 60% of the MCAD patients and treatment requires considerations outside of usual headache management.
Neuropeptides such as calcitonin gene-related peptide (CGRP), pituitary adenylate cyclase activating peptide (PACAP), and substance P (SP) activate mast cells leading to their degranulation and secretion of vasoactive, pro-inflammatory, and nerve-sensitizing mediators which contribute to the development of migraines.
Degranulation of meningeal mast cells leads to the sensitization of trigeminal vascular nerve processing and is believed to be one of the mechanisms underlying the migraine pain pathway. Brain mast cells also secrete pro-inflammatory and vasodilatory molecules such as interleukin-6 (IL-6) in response to corticotropin-releasing hormone (CRH), a mediator of stress as part of the HPA axis which is known to precipitate or exacerbate migraines.
First-line therapy is the application of acetaminophen, dipyrone, and NSAIDs, which should be used with particular caution due to the potential for NSAIDs to activate mast cells. When using NSAIDs, celecoxib (Celebrex) is less likely to activate mast cells than ibuprofen or aspirin.
If headache is resistant to these treatments, decreased potassium in the biophase of meningeal nerves may be the underlying cause. A therapeutic trial with oral substitution of K+ for 2 – 3 days would support the diagnosis. Another possible cause could be unrecognized MCAD-related nocturnal hypertension which would be an indication for antihypertensive therapy.
In MCAD patients, triptans, e.g., sumatriptan (Imitrex), should be used cautiously, since they may increase the number of mast cells and they may aggravate MCAD-related headache/migraines.
CGRP-based therapeutic antibodies and small molecule receptor antagonists.
A new class of migraine medications, calcitonin gene-related peptide (CGRP) receptor blockers, may offer significant benefit in the management of migraine headaches without increased risk of activating mast cells. CGRP is a potent vasodilator, especially of cranial vessels and leads to neurogenic inflammation by activating mast cells that can sensitize neurons and cause further vasodilation in the dura layer of the meninges.
Two CGRP receptor antagonists, ubrogepant (Ubrelvy) and rimegepant (Nurtec), have become available and appear effective for aborting acute migraine headaches. In addition, three monoclonal antibodies have now been approved by the FDA: Erenumab (Aimovig), blocks the CGRP receptor and fremanezumab (Ajovy) and galcanezumab (Emgality) that block the CGRP ligand. The antibodies may be effective for reducing migraine frequency and severity for at least 15 months with minimal adverse effects.
Treatment of Intraoperative/Postsurgical Pain and Inflammatory Pain
In order to prevent triggering mast cells in connection with surgical or endoscopic procedures, it may be possible to shield mast cells with a MCAD-specific intravenous pre-medication composed of a glucocorticoid (e.g., 30 – 100 mg prednisone depending on the disease intensity), 50 mg ranitidine, and 1 mg dimetinden maleate per 10 kg body weight. These medications should be given about 30 minutes before the beginning of the operative or endoscopic procedure. Injectable solutions containing ethanol should not be used in MCAD patients, since these patients are often highly intolerant even to the smallest quantities of ethanol.
In the intra- and postoperative period, the opioid analgesics meperidine (demerol), morphine, and codeine should be avoided, because of their high risk of inducing a massive mast mediator release. Opioid alternatives with a lower risk for inducing mast cell activation are remifentanil, alfentanil, fentanyl and oxycodone. Ketamine is an analgesic with an inhibitory effect on mast cells and can be used to prevent or treat postoperative surgical pain or non-surgical acute pain.
Other Symptomatic Treatment Options
Topical steroid creams (Cutaneous Mastocytosis – CM)
Mild to moderate cases of cutaneous mastocytosis are treated with topical steroid creams. which reduces the mast cells that can release histamine and trigger swelling (inflammation) in the skin.
Acute and chronic immunosuppressive therapies
Treatment with the following classes of medications is deferred to specialists experienced in the treatment of MCAD.
Though typically not first-choice, acute and chronic immunosuppressive therapies can be considered and may be particularly appropriate for patients possibly manifesting an autoimmune component of the disease (for example, suggested by the presence of anti-IgE or anti-IgE-receptor antibodies). Glucocorticoids may be beneficial for decreasing production of cytokines and reduced mast cell activation. Doses >20 mg prednisone equivalent per day are often needed to effectively control refractory acute and chronic symptoms. Glucocorticoids chronic toxicity profile related to long-term use is problematic.
The use of the antileukotriene class of medications (montelukast) may be effective for severe cases with respiratory system imvolvement.
If symptoms are resistant to therapy, as a next therapeutic step toward reducing mast cell activity by decreasing mediator release, treatment with ciclosporine (cyclosporine A), low dose methotrexate or azathioprine can be considered. Recently, anti-IgE treatment with monoclonal antibody omalizumab (Xolair) has helped with severe symptoms of MCAD. Omalizumab should be considered in cases of MCAD resistant to standard evidence-based therapy. As with all medications used to treat MCAD, their therapeutic success is strongly dependent on the individual patient.
Others
The use of azathioprine, methotrexate, ciclosporine, hydroxyurea, and tamoxifen in MCADs have been explored but discussion of their roles is beyond the scope of this website.
Resources
References
Mast Cell Activation Disease (MCAD)
MCAD – Overviews
- Mast cell activation disease – a concise practical guide for diagnostic workup and therapeutic options – 2011
- Pharmacological treatment options for mast cell activation disease – 2016
- A practical guide for treatment of pain in patients with systemic mast cell activation disease. – 2017
- Often seen, rarely recognized- mast cell activation disease–a guide to diagnosis and therapeutic options – PubMed 2016
- Mast cell stabilisers – PubMed 2016
- Characterization of Mast Cell Activation Syndrome – 2018
- Resveratrol Suppresses Gut-Derived NLRP3 Inflammasome Partly through Stabilizing Mast Cells in a Rat Model. -2018
- Controlling Mast Cell Activation and Homeostasis – Work Influenced by Bill Paul That Continues Today – 2018
- Mast Cell Regulation and Irritable Bowel Syndrome – Effects of Food Components with Potential Nutraceutical Use – 2020
- Recent advances in our understanding of mast cell activation – or should it be mast cell mediator disorders? – 2019
- Recent advances in the understanding and therapeutic management of mastocytosis – 2019
- Coronavirus 2019, Microthromboses, and Platelet Activating Factor – 2020
- Research Progress of the Antiviral Bioactivities of Natural Flavonoids – 2020
- Mast Cells and Irritable Bowel Syndrome – From the Bench to the Bedside – 2016
- Mast Cells in Gut and Brain and Their Potential Role as an Emerging Therapeutic Target for Neural Diseases – 2019
- The Role of Neuroinflammation in Postoperative Cognitive Dysfunction – Moving From Hypothesis to Treatment – 2018
- Brain “fog,” inflammation and obesity – key aspects of neuropsychiatric disorders improved by luteolin – 2015
- Nutraceuticals against Neurodegeneration – A Mechanistic Insight – 2016 Cerebral mast cells contribute to postoperative cognitive dysfunction by promoting blood brain barrier disruption – PubMed 2016
- Activated brain mast cells contribute to postoperative cognitive dysfunction by evoking microglia activation and neuronal apoptosis – 2016
- Mast Cell Neural Interactions in Health and Disease – 2019
- Mast Cells and Neuroinflammation – 2014
- Mast cell–glia axis in neuroinflammation and therapeutic potential of the anandamide congener palmitoylethanolamide – 2012
- Mast Cell – Glia Dialogue in Chronic Pain and Neuropathic Pain- Blood-Brain Barrier Implications – PubMed 2016
- Recent advances in mast cell activation and regulation – 2020
- Mast Cell Activation, Neuroinflammation, and Tight Junction Protein Derangement in Acute Traumatic Brain Injury – 2020
- Deepening the Mechanisms of Visceral Pain Persistence – An Evaluation of the Gut-Spinal Cord Relationship – 2020
- Mast cell degranulation distinctly activates trigemino-cervical and lumbosacral pain pathways and elicits widespread tactile pain hypersensitivity – 2012
- Mast Cells in Cardiac Fibrosis – New Insights Suggest Opportunities for Intervention 0 2019
- Mast cells – versatile gatekeepers of pain – 2015
- Irritable bowel syndrome – An inflammatory disease involving mast cells – 2011
- Mast cells signal their importance in health and disease – PubMed 2018
- 2020-TMS-ER-Protocol-2 Medications to Treat Mast Cell Diseases
- Systemic mastocytosis in adults – 2017 update on diagnosis, risk stratification and management – 2016
- TREATMENTS FOR MAST CELL DISEASES
- Comparing histamine intolerance and non-clonal mast cell activation syndrome – 2020
- Non-Clonal Mast Cell Activation – A Growing Body of Evidence – 2019
- Quercetin Is More Effective than Cromolyn in Blocking Human Mast Cell Cytokine Release and Inhibits Contact Dermatitis and Photosensitivity in Humans – 2012
- Mast Cell Disorders – Protean Manifestations and Treatment Responses – 2018
- The Mastocytosis Society Survey on Mast Cell Disorders – Patient Experiences and Perceptions – 2014
MCAD – Diagnosis
MCAD – Histamine Intolerance
- Evaluation of symptoms and symptom combinations in histamine intolerance – 2019
- Comparing histamine intolerance and non-clonal mast cell activation syndrome – 2020
MCAD – Treatment
- Study of Immunomodulation Using Naltrexone and Ketamine for COVID-19 – Full Text View – ClinicalTrials.gov – 2020
- Utility of hydroxyurea in mast cell activation syndrome – 2013
- Successful mast-cell-targeted treatment of chronic dyspareunia, vaginitis, and dysfunctional uterine bleeding – PubMed 2019
- Case Report – Treatment of systemic mastocytosis with sunitinib – 2017
- Chronic Pain Treatment – The Influence of Tricyclic Antidepressants on Serotonin Release and Uptake in Mast Cells – 2013
- TREATMENTS FOR MAST CELL DISEASES
- The Inhibitory Effects of Tetracycline on Mastocytosis – 2019
MCAD – Mast Cells and Cannabinoids
- Mast cells express a peripheral cannabinoid receptor with differential sensitivity to anandamide and palmitoylethanolamide. – 1995
- Cannabinomimetic control of mast cell mediator release- new perspective in chronic inflammation – 2008
- Cannabinoid receptor-specific mechanisms to alleviate pain in sickle cell anemia via inhibition of mast cell activation and neurogenic inflammation – 2016
- MCAS and Cannabidiol (CBD)- 2018
- Medical Cannabis & Mast Cell Activation Syndrome – 2019
- Cannabinoids in Pain Treatment – An Overview – 2019
- Cannabinoid receptor 1 controls human mucosal-type mast cell degranulation and maturation in situ – 2013
MCAD – Cardiovascular
MCAD – Bowel Disorders
MCAD – Mast Cells and COVID-19
- Covid-19 hyperinflammation and post-Covid-19 illness may be rooted in mast cell activation syndrome – 2020
- COVID‐19, pulmonary mast cells, cytokine storms, and beneficial actions of luteolin – 2020
- Dual-histamine receptor blockade with cetirizine – famotidine reduces pulmonary symptoms in COVID-19 patients – 2020
MCAD – Mast Cells and Microbiome
- Man and the Microbiome- A New Theory of Everything? – PubMed 2019
- Disentangling What We Know About Microbes and Mental Health – 2019
- The Evolving Role of Gut Microbiota in the Management of Irritable Bowel Syndrome – An Overview of the Current Knowledge – 2020
- Gut microbiota regulates neuropathic pain – potential mechanisms and therapeutic strategy – 2020
- Stress and the Microbiota–Gut–Brain Axis in Visceral Pain – Relevance to Irritable Bowel Syndrome – 2015
- Visceral pain – gut microbiota, a new hope? – 2019
- The Role of the Gastrointestinal Microbiota in Visceral Pain – PubMed 2017
- Gut-brain Axis and migraine headache – a comprehensive review – 2020
MCAD – Mast Cells and Opioids
- Opioid-Induced Mast Cell Activation and Vascular Responses Is Not Mediated by μ-Opioid Receptors – An In Vivo Microdialysis Study in Human Skin – 2004
- Which opioids in case of mast cell activation disorders? – 2019
MCAD – Mast Cells and Pain
- Mast cells synthesize, store, and release nerve growth factor. – 1994
- Chronic Pain Treatment – The Influence of Tricyclic Antidepressants on Serotonin Release and Uptake in Mast Cells – 2013
- Mast Cell-Mediated Mechanisms of Nociception – 2015
- A practical guide for treatment of pain in patients with systemic mast cell activation disease. – 2017
- Mast cell-neural interactions contribute to pain and itch – 2018
- Mast Cells in Stress, Pain, Blood-Brain Barrier, Neuroinflammation and Alzheimer’s Disease – 2019
- Mast Cells, Neuroinflammation and Pain in Fibromyalgia Syndrome – 2019
- Cannabinomimetic control of mast cell mediator release: new perspective in chronic inflammation. – PubMed – NCBI
- Involvement of mast cells in a mouse model of postoperative pain. – PubMed – NCBI – 2011
- Potential Mechanisms Underlying Centralized Pain and Emerging Therapeutic Interventions – 2018
- Calcitonin Gene-Related Peptide (CGRP) and Cluster Headache – 2020
- Primary headache syndromes in systemic mastocytosis – 2011
- Gut-brain Axis and migraine headache – a comprehensive review – 2020
- The role of mast cells in migraine pathophysiology – PubMed 2005
MCAD – Curcumin
- Twenty-first century mast cell stabilizers – 2013
- Curcumin and Health – 2016
- Curcumin Ingestion Inhibits Mastocytosis and Suppresses Intestinal Anaphylaxis in a Murine Model of Food Allergy – 2015
- Curcumin, a constituent of curry, suppresses IgE-mediated allergic response and mast cell activation at the level of Syk – PubMed 2007
MCAD – Palmitoylethanolamide (PEA)
- Mast cells express a peripheral cannabinoid receptor with differential sensitivity to anandamide and palmitoylethanolamide. – 1995
- New insights in mast cell modulation by palmitoylethanolamide – PubMed 2013
- Mast cells, glia and neuroinflammation – partners in crime? – 2013
- The pharmacology of palmitoylethanolamide and first data on the therapeutic efficacy of some of its new formulations – 2017
- Glia and mast cells as targets for palmitoylethanolamide, an anti-inflammatory and neuroprotective lipid mediator. – PubMed – NCBI
- Mast cell–glia axis in neuroinflammation and therapeutic potential of the anandamide congener palmitoylethanolamide – 2012
MCAD – Psychiatric Illness
MCAD – Restless Legs Syndrome
MCAD – Sickle Cell Disease
MCAD – Quercetin
- Quercetin and Vitamin C – An Experimental, Synergistic Therapy for the Prevention and Treatment of SARS-CoV-2 Related Disease (COVID-19) – 2020
- Quercetin Is More Effective than Cromolyn in Blocking Human Mast Cell Cytokine Release and Inhibits Contact Dermatitis and Photosensitivity in Humans – 2012
- Quercetin Inhibits the Production of IL-1β-Induced Inflammatory Cytokines and Chemokines in ARPE-19 Cells via the MAPK and NF-κB Signaling Pathways – 2020
- Quercetin and Its Anti-Allergic Immune Response – 2016
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
Accurate Supplement Prices
.
