Acute Pain:
Suzetrigine
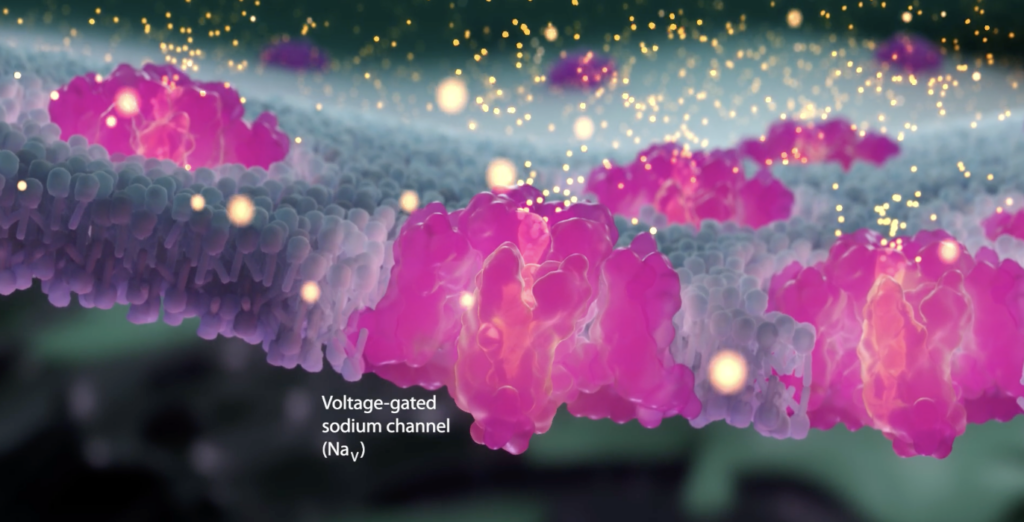
Vertex artist’s rendition of a sodium channel
With expected release in early 2025, a new option for the treatment of moderate-to-severe acute pain will become available. While still investigational, suzetrigine represents a novel non-opioid class of analgesic medications, the first new class of medicine to treat acute pain in over twenty years.
It is hoped that this new pain medication will offer an opportunity to not only lessen the experience of acute pain but also reduce the transition from acute to chronic pain. Additionally, there is preliminary evidence to suggest that it may also be effective for the treatment of diabetic peripheral neuropathy pain.
What is Suzetrigine?
Suzetrigine is a small-molecule, non-opioid analgesic that works to relieve moderate to severe pain by inhibiting pain signaling in the peripheral nervous system only, it does not enter the central nervous system (spinal cord or brain). Because of this limited area of activity, suzetrigine is not expected to allow potential for addiction, nor is it expected to contribute to accidental overdose if combined with opioids. Suzetrigine is being developed by Vertex Pharmaceuticals and has completed two Phase III trials.
Clinical Trials of Suzetrigine
Two phase 2 clinical trials of suzetrigine have’been conducted involving participants with acute pain after abdominoplasty (tummy tuck) or bunionectomy. As compared to placebo, suzetrigine was found to be effective over 48 hours for the acute pain associated with these conditions. Side effects, including headache and constipation, were common but only mild to moderate severity. (ClinicalTrials.gov numbers, NCT04977336 and NCT05034952).
Acute Pain
Acute pain is the first response to damaged tissue, followed by inflammation that triggers swelling of the area and promotes tissue repair However, if the pain persists for more than 3 months, it is defined as chronic and it becomes a pathological condition in itself. This temporal parameter is used to define the distinction between acute and chronic pain because there are no biomarkers or measurable physiological conditions that distinguish acute from chronic pain.
Potential Benefits for Osteoarthritis
Osteoarthritis (OA) is a currently incurable, chronic, progressive, and debilitating musculoskeletal condition. One of its hall- mark symptoms is chronic nociceptive and neuropathic pain, which significantly reduces the quality of life of patients with OA. Although research into the mechanisms of OA pain is ongoing and several pain pathways are well understood, the true source of OA pain remains unclear. Voltage-gated sodium ion channels are key mediators of OA pain and are involved in all major synovial joint tissues in the context of pain generation. As such, this new class of medication may have the potential to target pain in patients with OA.
Rotator Cuff Pain
Chronic pain in biceps tendinopathy, characterized by pain and weakness in the tendon of the long head of biceps brachii muscle, is presumed to arise from neurogenic inflammation, central pain sensitization, excitatory nerve augmentation, inhibitory nerve loss, and/or dysregulation of supraspinal structures. Multiple ion channels are involved in these pain pathways including TRPV1 and 3, TRPA1, TRPM8, Nav1.7, Nav1.8, and Nav1.9, suggesting potential benefit of suzetrigine for acute rotator cuff injury.
Transitioning from Acute to Chronic Pain
Relatively little is known about the molecular mechanisms responsible for how the increased sensitivity of primary peripheral nerve develops (owing to injury or inflammation, increased sensitivity of the respective primary afferent fibers develops) or how central sensitization develops (upon repeated stimuli, increased spinal neuronal excitability with diminished firing threshold occurs). What is known is that transitioning from acute to chronic pain involves the development of peripheral and central sensitization and that reducing the severity of acute pain reduces the likelihood of it evolving into chronic pain. It stands to reason therefore that if suzetrigine effectively reduces the severity of acute pain by reducing pain signaling in the peripheral nerves, it is likely that doing so may reduce the development of peripheral and central sensitization and the subsequent transition of acute to chronic pain. (See “Avoiding The Transition of Acute to Chronic Pain”).
How Suzetrigine Works: Sodium Channels and Pain Signaling
The experience of pain originates when pain receptors (nociceptors) at the site of injury are triggered and these receptors send signals along peripheral nerves in the form the form of action potentials. These action potentials propagate signals through the nerves in the peripheral nervous system, or PNS, where they then enter the spinal cord and into the central nervous system, or CNS. In the dorsal horn of the spinal cord these pain signals are then propagated to several brain regions resulting in the perception of pain.
The propagation of nerve signals is driven by voltage-gated sodium channels, or NaVs. Following pain receptor stimulation, sodium channels in pain-sensing neurons open, allowing an influx of sodium ions which generates action potentials that are ultimately signaled to the brain. There are nine NaV subtypes distributed throughout the body with some of them them predominantly expressed in the CNS, while others are found in the heart or muscle.
Three NaV subtypes are predominantly expressed in the peripheral nociceptive neurons in the PNS:
- NaV1.7 has been associated with certain neuropathies.
- NaV1.8 has been associated with the transmission of nociceptive stimuli.
- NaV1.9 has been associated with episodic pain syndromes.
About Suzetrigine (VX-548)
Suzetrigine (formerly VX-548) is an investigational oral, selective NaV1.8 pain signal inhibitor that is highly selective for NaV1.8 relative to other NaV channels. NaV1.8 is a voltage-gated sodium channel that is selectively expressed in peripheral pain-sensing neurons (nociceptors), where its role is to transmit pain signals (action potentials). NaV1.8 is a genetically validated target for the treatment of pain, and suzetrigine has demonstrated a favorable benefit/risk profile in three Phase 3 studies and two Phase 2 studies in patients with moderate-to-severe acute pain. Suzetrigine also demonstrated positive results and a well-tolerated profile in a Phase 2 study in patients with pain associated with diabetic peripheral neuropathy, a type of chronic peripheral neuropathic pain. Vertex’s approach is to selectively inhibit NaV1.8 using small molecules with the objective of creating a new class of pain signal inhibitors that have the potential to provide effective relief of pain without the limitations of currently available therapies, including the addictive potential of opioids.
Aside from concerns regarding loss or impairment of function after being injured, most people’s primary concern revolves around their pain and it’s effective management. This is especially true for patients who, prior to their acute injury, already suffer from chronic pain and belong to a population that research has shown to be hypersensitive to pain.
Management of pain in the days and weeks after an injury is important in itself. But it is also important because how well that acute pain is managed can impact the ultimate duration and severity of that pain. The goal of pain management is not “zero pain” but pain that is tolerable and allows the patient to function. What is most important to understand, however, is that the most significant, consistent factor contributing to the risk of progression of acute to chronic post-injury pain is the duration of severe acute post-injury pain which can lead to peripheral and central sensitization (See “Avoiding The Transition of Acute to Chronic Pain”).
See:
- Acute Pain – Avoiding Transition to Chronic Pain
- The Transition of Acute Post-Injury Opioid Use to Chronic Opioid Use
See also:
- Central Sensitization
- Neurobiology of Pain
- Gabapentin & Lyrica
- Palmitoylethanolamide (PEA)
- Dextromethorphan
- Ketamine
- Levorphanol
see also:
Definitions and Terms Related to Pain
Key to Links:
- Grey text – handout
- Red text – another page on this website
- Blue text – Journal publication
References:
Suzetrigine
- Vertex Announces FDA Acceptance of New Drug Application for Suzetrigine for the Treatment of Moderate-to-Severe Acute Pain – 2024
- Selective Inhibition of NaV1.8 with VX-548 for Acute Pain – PubMed – 2023
- Sodium Channels in Pain – 2024
- www.sodiumchannels.com
Regulation of pain & ion channels
- Peripheral mechanisms of peripheral neuropathic pain – 2023
- Communicating pain – emerging axonal signaling in peripheral neuropathic pain – 2024
- Pain Management Strategies in Osteoarthritis – 2024
- Regulation of pain neurotransmitters and chondrocytes metabolism mediated by voltage-gated ion channels- A narrative review – 2023
- Ion channels involved in inflammation and pain in osteoarthritis and related musculoskeletal disorders – 2023
- Ion channels in osteoarthritis_ emerging roles and potential targets – PubMed – 2024
Acute Post-Injury Pain – Overviews
- Preventing chronic pain following acute pain – risk factors, preventive strategies, and their efficacy – 2011
- Ohio Guideline for the Management of Acute Pain Outside of Emergency Departments – 2016
- Clinical Practice Guidelines for Pain Management in Acute Musculoskeletal Injury – 2019
- Medical Management of Acute Pain – 2019
- Pain Management Best Practices Inter-Agency Task Force Report – 2019
- Medical Management of Acute Pain – 2019
- Treatments for Acute Pain – A Systematic Review – 2020
- Best Practices Guidelines for Acute Pain Management in Trauma Patients – 2020
- chronic post-hernia repair pain-2023
Acute Post-Injury Pain – Acetaminophen (Tylenol)
- AM404, an inhibitor of anandamide uptake, prevents pain behaviour and modulates cytokine and apoptotic pathways in a rat model of neuropathic pain – 2006
- AM404, paracetamol metabolite, prevents prostaglandin synthesis in activated microglia by inhibiting COX activity – 2017
- First evidence of the conversion of paracetamol to AM404 in human cerebrospinal fluid – 2017
- Acetaminophen metabolites p-aminophenol and AM404 inhibit microglial activation – 2018
- Pharmacological Management of Adults with Chronic Non-Cancer Pain in General Practice – 2020
- Analgesic Effect of Acetaminophen – A Review of Known and Novel Mechanisms of Action – 2020
Acute Post-Injury Pain – Oxidative Stress
- Roles of Reactive Oxygen and Nitrogen Species in Pain – 2011
- Clinical Relevance of Biomarkers of Oxidative Stress – 2015
- The Interplay between Oxidative Stress, Exercise, and Pain in Health and Disease – Potential Role of Autonomic Regulation and Epigenetic Mechanisms – 2020
- Neuropathic Pain – Delving into the Oxidative Origin and the Possible Implication of Transient Receptor Potential Channels – 2018
Acute Post-Injury Pain – Massage
Massage for Low Back Pain – 2009
Acute Post-Injury Pain – Ultrasound Therapy
- Overview of Therapeutic Ultrasound Applications and Safety Considerations – 2012
- Randomized controlled study of the antinociceptive effect of ultrasound on trigger point sensitivity novel applications in myofascial therapy? – PubMed – 2007
- Effectiveness of ultrasound therapy for myofascial pain syndrome – a systematic review and meta-analysis – 2017
- Effect of Therapeutic Sequence of Hot Pack and Ultrasound on Physiological Response Over Trigger Point of Upper Trapezius – 2015
- Effectiveness of Ultrasound Therapy on Myofascial Pain Syndrome of the Upper Trapezius – Randomized, Single-Blind, Placebo-Controlled Study – 2018
Acute Post-Injury Pain – Muscle Relaxers
- Randomized-controlled trial of methocarbamol as a novel treatment for muscle cramps in cirrhotic patients – PubMed – 2019
- Randomized placebo-controlled study of baclofen in the treatment of muscle cramps in patients with liver cirrhosis – PubMed – 2016
- Pilot study of orphenadrine as a novel treatment for muscle cramps in patients with liver cirrhosis – 2018
Acute Post-Injury Pain – Myofascial Pain
- Effectiveness of Ultrasound Therapy on Myofascial Pain Syndrome of the Upper Trapezius – Randomized, Single-Blind, Placebo-Controlled Study – 2018
- Myofascial Pain Syndrome in the Elderly and Self-Exercise – A Single-Blind, Randomized, Controlled Trial – 2016
- Effect of Therapeutic Sequence of Hot Pack and Ultrasound on Physiological Response Over Trigger Point of Upper Trapezius – 2015
- Effectiveness of ultrasound therapy for myofascial pain syndrome – a systematic review and meta-analysis – 2017
- Randomized controlled study of the antinociceptive effect of ultrasound on trigger point sensitivity novel applications in myofascial therapy? – PubMed – 2007
Myofascial Pain – Muscle Cramps
- Association Between Long-term Quinine Exposure and All-Cause Mortality – 2017
- Muscle Cramps Do Not Improve With Correction of Vitamin D Insufficiency – 2019
- Criteria in diagnosing nocturnal leg cramps – a systematic review – 2017
- Treatment of nocturnal leg cramps by blockade of the medial branch of the deep peroneal nerve after lumbar spine surgery – 2015
- Nocturnal Cramps in Patients with Lumbar Spinal Canal Stenosis Treated Conservatively – A Prospective Study – 2014
- Magnesium – Biochemistry, Nutrition, Detection, and Social Impact of Diseases Linked to Its Deficiency – 2021
- What is the role of magnesium for skeletal muscle cramps? A Cochrane Review summary with commentary – 2021
- Magnesium for skeletal muscle cramps – PubMed – 2020
- Non‐drug therapies for lower limb muscle cramps – 2012
- Non-drug therapies for the secondary prevention of lower limb muscle cramps – PubMed – 2021
- Nocturnal leg cramps in older people – 2002
- Assessment – symptomatic treatment for muscle cramps (an evidence-based review) report of the therapeutics and technology assessment subcommittee of the American academy of neurology – PubMed – 2010
- A scoping review to identify and map the multidimensional domains of pain in adults with advanced liver disease – 2020
- Randomized-controlled trial of methocarbamol as a novel treatment for muscle cramps in cirrhotic patients – PubMed – 2019
- Randomized placebo-controlled study of baclofen in the treatment of muscle cramps in patients with liver cirrhosis – PubMed – 2016
- Pilot study of orphenadrine as a novel treatment for muscle cramps in patients with liver cirrhosis – 2018
Reducing Acute Post-Injury Pain – Physical Therapy
Preventing Pain Related to Surgery – Overviews
- perioperative-pain-management- 2007 pubmed-ncbi
- Pharmacotherapy for the prevention of chronic pain after surgery in adults (Review) – 2013
- optimizing-pain-management-to-facilitate-enhanced-recovery-after-surgery-pathways 2015 -pubmed-ncbi
- development-of-a-management-algorithm-for-post-operative-pain-mapp-after-total-knee-and-total-hip-replacement-2014
- Post-operative Opioid-Induced Hyperalgesia – ICM Case Summaries – 2016
- The Complexity Model – A Novel Approach to Improve Chronic Pain Care – 2014
- Postoperative_pain_from_mechanisms_to_treatment.
- Mechanisms of acute and chronic pain after surgery: update from findings in experimental animal models. – PubMed – NCBI – 2018
- Short-term pre- and post-operative stress prolongs incision-induced pain hypersensitivity without changing basal pain perception – 2015
- Age and preoperative pain are major confounders for sex differences in postoperative pain outcome – A prospective database analysis – 2017
- Optimizing pain management to facilitate Enhanced Recovery After Surgery pathways. – PubMed – NCBI – 2015
- Reward Circuitry Plasticity in Pain Perception and Modulation – 2017
- Surgically-Induced Neuropathic Pain (SNPP) – Understanding the Perioperative Process – 2013
- Preventing Chronic Pain following Acute Pain – Risk Factors, Preventive Strategies, and their Efficacy – 2011
- Regular physical activity prevents development of chronic pain and activation of central neurons – 2013
- Regional anaesthesia to prevent chronic pain after surgery – a Cochrane systematic review and meta-analysis – 2013
- Pharmacotherapy for the prevention of chronic pain after surgery in adults – 2017
- A systematic review of therapeutic interventions to reduce acute and chronic post-surgical pain after amputation, thoracotomy or mastectomy. – 2015
- Analysis of perioperative pain management in vascular surgery indicates that practice does not adhere with guidelines – a retrospective cross-sectional study – 2017
- Efficacy and safety of multimodal analgesic techniques for preventing chronic postsurgery pain under different surgical categories – a meta-analysis – 2017
- Postoperative pain—from mechanisms to treatment – 2017
- Local anaesthetics and regional anaesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children – 2018
- Chronic postsurgical pain – current evidence for prevention and management – 2018
- Preventive analgesia and novel strategies for the prevention of chronic post-surgical pain. – (2015)
- Poorly controlled postoperative pain – prevalence, consequences, and prevention – 2017
- Designing the ideal perioperative pain management plan starts with multimodal analgesia – 2018
- Special indications for Opioid Free Anaesthesia and Analgesia, patient and procedure related: Including obesity, sleep apnoea, chronic obstructive … – PubMed – NCBI – 2017
- Chronic pain patient and anaesthesia – 2019
- New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults – 2017
- Multimodal Analgesia, Current Concepts, and Acute Pain Considerations. – PubMed – NCBI -2017
- Recent Advances in Postoperative Pain Management – 2010
- Effect of perioperative systemic alpha2-agonists on postoperative morphine consumption and pain intensity – systematic review of randomized controlled trials- 2011
- Cannabinoids for Postoperative Pain – 2007
- Educating Patients Regarding Pain Management and Safe Opioid Use After Surgery – 2020
Preventing Pain Related to Surgery – Phantom Limb Pain
- Strategies for prevention of lower limb post-amputation pain: A clinical narrative review – 2018
- Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: a prospective, randomized, clinical trial. – PubMed – NCBI – 2011
- Chronic post-amputation pain – peri-operative management – Review 0- 2017
Reducing Acute Post-Injury Pain – Physical Therapy
Preventing Pain Related to Surgery – Enhanced Recovery After Surgery (ERAS)
- Enhanced Recovery After Surgery: A Review. – PubMed – NCBI – 2017
- Pain management within an enhanced recovery program after thoracic surgery – 2018
- Optimizing pain management to facilitate Enhanced Recovery After Surgery pathways. – PubMed – NCBI – 2015
Preventing Pain Related to Surgery – Neuroinflammation, Glial Cells & Mast Cells
- Involvement of mast cells in a mouse model of postoperative pain. – PubMed – NCBI – 2011
- An Inflammation-Centric View of Neurological Disease – Beyond the Neuron – 2018
- Rescue of Noradrenergic System as a Novel Pharmacological Strategy in the Treatment of Chronic Pain – Focus on Microglia Activation – 2019
Preventing Pain Related to Surgery – Resolving Inflammation
- Vagus nerve controls resolution and pro-resolving mediators of inflammation – 2014
- The Resolution Code of Acute Inflammation – Novel Pro-Resolving Lipid Mediators in Resolution – 2015
- Resolvins in inflammation: emergence of the pro-resolving superfamily of mediators. – PubMed – NCBI – 2018
- Resolvins and protectins – mediating solutions to inflammation – 2009
- Resolvins and inflammatory pain – 2011
- Resolution of inflammation – an integrated view – 2013
- Protectins and maresins – New pro-resolving families of mediators in acute inflammation and resolution bioactive metabolome – 2014
- Proresolving lipid mediators and mechanisms in the resolution of acute inflammation – 2014
- Novel Pro-Resolving Lipid Mediators in Inflammation Are Leads for Resolution Physiology – 2014
- Novel Anti-Inflammatory — Pro-Resolving Mediators and Their Receptors – 2011
- Lipid Mediators in the Resolution of Inflammation – 2015
- PPARγ activation ameliorates postoperative cognitive decline probably through suppressing hippocampal neuroinflammation in aged mice. – PubMed – NCBI – 2017
- Postoperative cognitive dysfunction in the aged: the collision of neuroinflammaging with perioperative neuroinflammation. – PubMed – NCBI – 2018
- The Role of Neuroinflammation in Postoperative Cognitive Dysfunction – Moving From Hypothesis to Treatment – 2018
- Treating inflammation and infection in the 21st century: new hints from decoding resolution mediators and mechanisms – 2017
- Structural Elucidation and Physiologic Functions of Specialized Pro-Resolving Mediators and Their Receptors – 2017
- LPS is a Switch for Inflammation in the Gut and Beyond
- Identification of specialized pro-resolving mediator clusters from healthy adults after intravenous low-dose endotoxin and omega-3 supplementation – a methodological validation – 2018
- The Protectin Family of Specialized Pro-resolving Mediators – Potent Immunoresolvents Enabling Innovative Approaches to Target Obesity and Diabetes – 2018
- Protectins and Maresins – New Pro-Resolving Families of Mediators in Acute Inflammation and Resolution Bioactive Metabolome – 2014
- Functional Metabolomics Reveals Novel Active Products in the DHA Metabolome – 2012
Preventing Pain Related to Surgery – Alpha-2 Agonists
Preventing Pain Related to Surgery – Buprenorphine
- Role of buprenorphine in acute postoperative pain – 2016
- Efficacy and Safety of Transdermal Buprenorphine versus Oral Tramadol:Acetaminophen in Patients with Persistent Postoperative Pain after Spinal Surgery – 2017
- Low-dose buprenorphine infusion to prevent postoperative hyperalgesia in patients undergoing major lung surgery and remifentanil infusion a double-blind, randomized, active-controlled trial – 2017
Preventing Pain Related to Surgery – Diet
Preventing Pain Related to Surgery – Genetics
- genotyping-test-with-clinical-factors-better-management-of-acute-postoperative-pain-2015
- the-impact-of-genetic-variation-on-sensitivity-to-opioid-analgesics-in-patients-with-postoperative-pain-a-systematic-review-and-meta-analysis-2015
- Chronic postsurgical pain – is there a possible genetic link? – 2017
Preventing Pain Related to Surgery – Epigenetics
- Epigenetic-regulation-of-spinal-cord-gene-expression-controls-opioid-induced-hyperalgesia-2014
- Epigenetic-regulation-of-opioid-induced-hyperalgesia-dependence-and-tolerance-in-mice-2013
- Epigenetic-regulation-of-persistent-pain-2015
- Chronic-opioid-use-is-associated-with-increased-dna-methylation-correlating-with-increased-clinical-pain-pubmed-ncbi
- Could targeting epigenetic processes relieve chronic pain states? – PubMed – NCBI
- Epigenetic-mechanisms-of-chronic-pain-2015
- Telomeres and epigenetics – Potential relevance to chronic pain – 2012
- Epigenetics of chronic pain after thoracic surgery. – PubMed – NCBI
- Epigenetics-in-the-perioperative-period-2015
Preventing Pain Related to Surgery – Gabapentin & Pregabalin
- Do surgical patients benefit from perioperative gabapentin:pregabalin? A systematic review of efficacy and safety. – PubMed – NCBI
- Perioperative administration of gabapentin 1,200 mg day−1 and pregabalin 300 mg day−1 for pain following lumbar laminectomy and discectomy – 2011
- Preemptive use of gabapentin in abdominal hysterectomy: a systematic review and meta-analysis. – PubMed – NCBI
- The Effect of Gabapentin on Acute Postoperative Pain in Patients Undergoing Total Knee Arthroplasty – 2016
- The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. – PubMed – NCBI
- The use of gabapentin in the management of postoperative pain after total hip arthroplasty – 2016
- The use of gabapentin in the management of postoperative pain after total knee arthroplasty – 2016
- Use of gabapentin for perioperative pain control – A meta-analysis – 2007
- The efficacy of gabapentin:pregabalin in improving pain after tonsillectomy: A meta-analysis. – PubMed – NCBI
- Effects of gabapentin on postoperative pain, nausea and vomiting after abdominal hysterectomy: a double blind randomized clinical trial. – PubMed – NCBI
- Gabapentin and postoperative pain – a systematic review of randomized controlled trials 2006 – PubMed Health
- Preoperative Preemptive Drug Administration for Acute Postoperative Pain – A Systematic Review And Meta-Analysis – 2016
- the-effects-of-preoperative-oral-pregabalin-and-perioperative-intravenous-lidocaine-infusion-on-postoperative-morphine-requirement-in-patients-undergoing-laparatomy-2015
- perioperative-pain-management- 2007 pubmed-ncbi
- optimizing-pain-management-to-facilitate-enhanced-recovery-after-surgery-pathways 2015 -pubmed-ncbi
- Treatment_of_Neuropathic_Pain_The_Role_of_Unique_Opioid_Agents_-_2016
- The Anti-Allodynic Gabapentinoids – Myths, Paradoxes, and Acute Effects – 2016
- Gabapentinoids as a Part of Multi-modal Drug Regime for Pain Relief following Laproscopic Cholecystectomy: A Randomized Study – 2017
- Effects of pregabalin and gabapentin on postoperative pain and opioid consumption after laparoscopic cholecystectomy – 2017
- Do surgical patients benefit from perioperative gabapentin:pregabalin? A systematic review of efficacy and safety. – PubMed – NCBI
- Impact of pregabalin on acute and persistent postoperative pain: a systematic review and meta-analysis. – PubMed – NCBI
- Effects of pregabalin and gabapentin on postoperative pain and opioid consumption after laparoscopic cholecystectomy – 2017
- Effect of Perioperative Gabapentin on Postoperative Pain Resolution and Opioid Cessation in a Mixed Surgical Cohort – 2018
Preventing Pain Related to Surgery – Ketamine & NMDA Antagonists
- Role of Ketamine in Acute Postoperative Pain Management – A Narrative Review – 2015
- Perioperative ketamine for acute postoperative pain. – PubMed – NCBI
- Ketamine decreases postoperative pain scores in patients taking opioids for chronic pain: results of a prospective, randomized, double-blind study. – PubMed – NCBI
- Intraoperative ketamine reduces perioperative opiate consumption in opiate-dependent patients with chronic back pain undergoing back surgery. – PubMed – NCBI
- Ketamine as an Adjunct to Postoperative Pain Management in Opioid Tolerant Patients After Spinal Fusions – A Prospective Randomized Trial – 2007
- The efficacy of N-methyl-D-aspartate receptor antagonists on improving the postoperative pain intensity and satisfaction after remifentanil-based a… – PubMed – NCBI
- The clinical role of NMDA receptor antagonists for the treatment of postoperative pain. – PubMed – NCBI
- Ketamine – an old drug revitalized in pain medicine – 2017
- Effect of ketamine combined with magnesium sulfate in neuropathic pain patients (KETAPAIN) – study protocol for a randomized controlled trial – 2017
- A systematic review and meta-analysis of ketamine for the prevention of persistent post-surgical pain. – PubMed – NCBI – 2014
- Ketamine for pain – 2017
- Ketamine for pain management – 2018
- Butorphanol and Ketamine Combined in Infusion Solutions for Patient-Controlled Analgesia Administration – A Long-Term Stability Study – 2015
- Multimodal Analgesia, Current Concepts, and Acute Pain Considerations. – PubMed – NCBI -2017
Preventing Pain Related to Surgery – Magnesium
- Perioperative systemic magnesium to minimize postoperative pain: a meta-analysis of randomized controlled trials. – PubMed – NCBI
- Peri-operative intravenous administration of magnesium sulphate and postoperative pain – a meta-analysis – 2013
- Effect of magnesium sulfate on morphine activity retention to control pain after herniorrhaphy. – PubMed – NCBI
- Effect of ketamine combined with magnesium sulfate in neuropathic pain patients (KETAPAIN) – study protocol for a randomized controlled trial – 2017
Preventing Pain Related to Surgery – NSAIDs
See: NSAIDs
- Sulfonamide cross-reactivity: is there evidence to support broad cross-allergenicity? – PubMed – NCBI – 2013
- Should celecoxib be contraindicated in patients who are allergic to sulfonamides? Revisiting the meaning of ‘sulfa’ allergy. – PubMed – NCBI 2001
Preventing Pain Related to Surgery – Nefopam
- nefopam-after-total-hip-arthroplasty-role-in-multimodal-analgesia-pubmed-ncbi
- nefopam-analgesia-and-its-role-in-multimodal-analgesia-a-review-of-preclinical-and-clinical-studies-pubmed-ncbi
- preventive-analgesic-efficacy-of-nefopam-in-acute-and-chronic-pain-after-breast-cancer-surgery-2016
- neuronal-sensitization-and-its-behavioral-correlates-in-a-rat-model-of-neuropathy-are-prevented-by-a-cyclic-analog-of-orphenadrine-pubmed-ncbi
Preventing Pain Related to Surgery – Tapentadol (Nucynta)
Preventing Pain Related to Surgery – Vitamin C
Chronic Regional Pain Syndrome (CRPS)/Reflex Sympathetic Dystrophy (RSD)
- Efficacy of vitamin C in preventing complex regional pain syndrome after wrist fracture – A systematic review and meta-analysis – 2017
- [Vitamin C and prevention of reflex sympathetic dystrophy following surgical management of distal radius fractures]. – PubMed – NCBI
- Complex regional pain syndrome – recent updates – 2013
- Give vitamin C to avert lingering pain after fracture – 2008
- Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures – a randomised trial – 1999
- Effect of vitamin C on prevention of complex regional pain syndrome type I in foot and ankle surgery. – PubMed – NCBI – 2009
Preventing Pain Related to Surgery – Vitamin C
Lumbar Surgery
Preventing Pain Related to Surgery – Vitamin D
- The Preoperative Supplementation With Vitamin D Attenuated Pain Intensity and Reduced the Level of Pro-inflammatory Markers in Patients After Posterior Lumbar Interbody Fusion – 2019
- Vitamin D and Its Potential Interplay With Pain Signaling Pathways – 2020
- Vitamin D for the treatment of chronic painful conditions in adults – 2014
- Vitamin D in Pain Management – 2017
- Is there a role for vitamin D in the treatment of chronic pain? – 2017
- Vitamin D Deficiency and Pain – Clinical Evidence of Low Levels of Vitamin D and Supplementation in Chronic Pain States- 2015
Opioids – Transitioning from Short Term to Long Term Use
- How acute pain leads to chronic opioid use – 2018
- Characteristics of initial prescription episodes and likelihood of long-term opioid use – United States, 2006-2015
- New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults – 2017
Emphasis on Education
Accurate Clinic promotes patient education as the foundation of it’s medical care. In Dr. Ehlenberger’s integrative approach to patient care, including conventional and complementary and alternative medical (CAM) treatments, he may encourage or provide advice about the use of supplements. However, the specifics of choice of supplement, dosing and duration of treatment should be individualized through discussion with Dr. Ehlenberger. The following information and reference articles are presented to provide the reader with some of the latest research to facilitate evidence-based, informed decisions regarding the use of conventional as well as CAM treatments.
For medical-legal reasons, access to these links is limited to patients enrolled in an Accurate Clinic medical program.
Please note also, that many of the benefits for medications described on this web site include “off-label” use for a medication. Off-label prescribing refers to the use of medication for a condition not named in its FDA approval. Physicians are free to prescribe any medication they want, as long as there is some evidence for usefulness. And remember that the lack of an FDA indication does not necessarily mean lack of efficacy—it sometimes means that no drug company has deemed the investment in clinical trials worth the eventual pay off.
Should you wish more information regarding any of the subjects listed – or not listed – here, please contact Dr. Ehlenberger. He has literally thousands of published articles to share on hundreds of topics associated with pain management, weight loss, nutrition, addiction recovery and emergency medicine. It would take years for you to read them, as it did him.
For more information, please contact Accurate Clinic.
Supplements recommended by Dr. Ehlenberger may be purchased commercially online or at Accurate Clinic.
Please read about our statement regarding the sale of products recommended by Dr. Ehlenberger.
